Clin Orthop Surg.
2017 Sep;9(3):392-395. 10.4055/cios.2017.9.3.392.
Retrograde Intramedullary Nailing for Humerus Fracture in a Supine Position: Performing an Unfamiliar Procedure in a Familiar Position
- Affiliations
-
- 1Department of Orthopaedic Surgery, Konyang University College of Medicine, Daejeon, Korea. oeo-oeoeo@hanmail.net
- KMID: 2412277
- DOI: http://doi.org/10.4055/cios.2017.9.3.392
Abstract
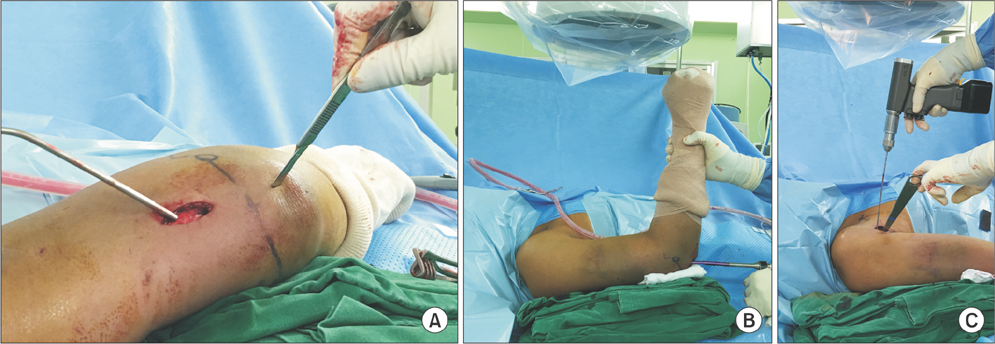
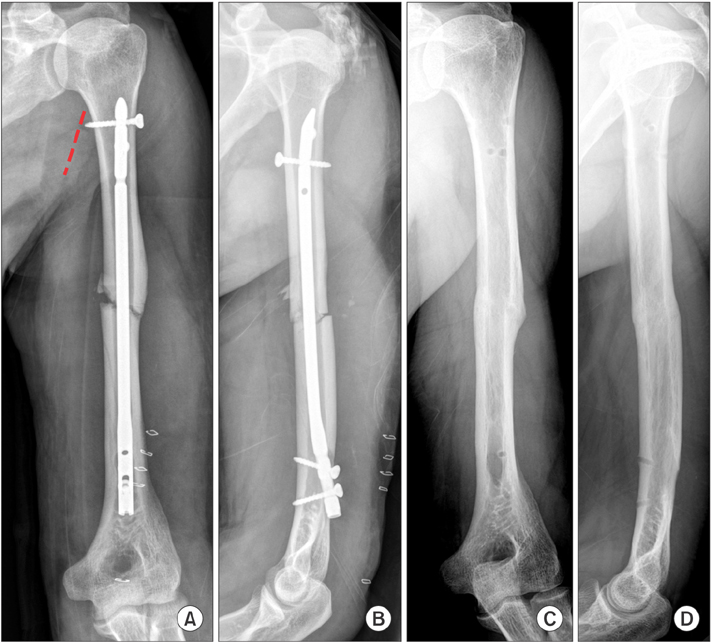
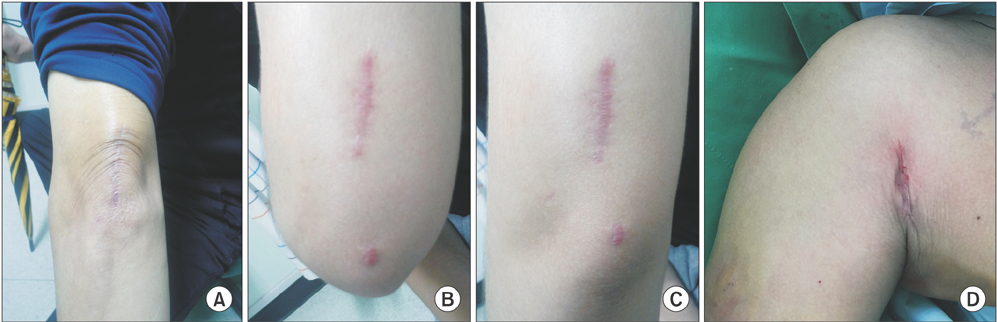
- Intramedullary (IM) nailing for humeral shaft fracture has provided excellent outcomes in terms of fracture biology and cosmetic appearance because of the relatively small incision involved. However, antegrade nailing causes issues such as iatrogenic rotator cuff injury. Retrograde nail fixation method could avoid cuff injury, but has shortcomings such as the need for the prone or lateral decubitus position during surgery. We report that the retrograde IM nail fixation technique performed in a supine position and some ancillary techniques for minimizing scars or complications can provide the advantages of both retrograde nailing and supine position during surgery.
MeSH Terms
Figure
Reference
-
1. Kumar R, Singh P, Chaudhary LJ, Singh S. Humeral shaft fracture management, a prospective study; nailing or plating. J Clin Orthop Trauma. 2012; 3(1):37–42.
Article2. Strohm PC, Reising K, Hammer T, Sudkamp NP, Jaeger M, Schmal H. Humerus shaft fractures: where are we today? Acta Chir Orthop Traumatol Cech. 2011; 78(3):185–189.3. Verdano MA, Pellegrini A, Schiavi P, Somenzi L, Concari G, Ceccarelli F. Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop. 2013; 37(10):2001–2007.
Article4. Baltov A, Mihail R, Dian E. Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury. 2014; 45:Suppl 1. S9–S15.
Article5. Logters TT, Wild M, Windolf J, Linhart W. Axillary nerve palsy after retrograde humeral nailing: clinical confirmation of an anatomical fear. Arch Orthop Trauma Surg. 2008; 128(12):1431–1435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramedullary Nailing of Femoral Shaft Fractures : Comparison between with and without the Fracture Table
- Lateral Positioning for Proximal Femoral Nailing of the Intertrochanteric Fracture: Surgical Technique
- Retrograde Kuntscher nailing in treatment of fracture of humerus shaft
- Interlocking Intramedullary Nailing of the Humerus Shaft Fractures
- Plain Radiograph Analysis of the Distal Humerus Posterior Bowing That May Affect Interlocking Intramedullary Nailing for Humerus Shaft Fracture