J Korean Ophthalmol Soc.
2018 May;59(5):437-443. 10.3341/jkos.2018.59.5.437.
Intravitreal Aflibercept Monotherapy for Treating Submacular Hemorrhage Secondary to Neovascular Age-related Macular Degeneration
- Affiliations
-
- 1Sungmo Eye Hospital, Busan, Korea. heesyoon@dreamwiz.com
- KMID: 2411457
- DOI: http://doi.org/10.3341/jkos.2018.59.5.437
Abstract
- PURPOSE
To evaluate the effects of intravitreal aflibercept injection in the treatment of submacular hemorrhage secondary to neovascular age-related macular degeneration (nAMD).
METHODS
This retrospective, observational study included patients diagnosed with nAMD with submacular hemorrhage treated with intravitreal aflibercept monotherapy. A total of 54 eyes of 54 patients were treated with an initial series of three monthly intravitreal aflibercept injections followed by as-needed injections. At the 6 month follow-up, changes in best-corrected visual acuity (BCVA), central macular thickness (CMT), and submacular hemorrhage area (SMH) were evaluated.
RESULTS
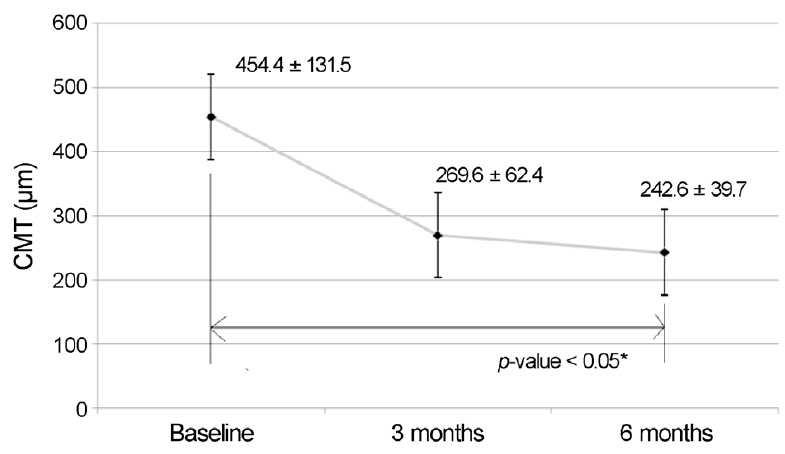
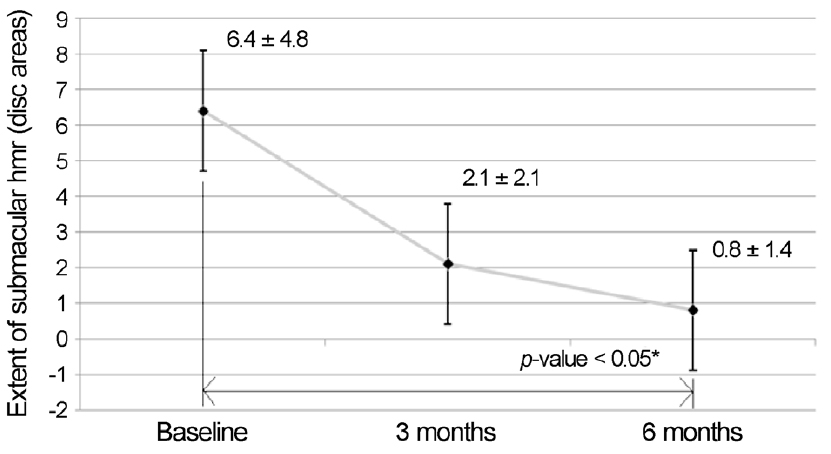
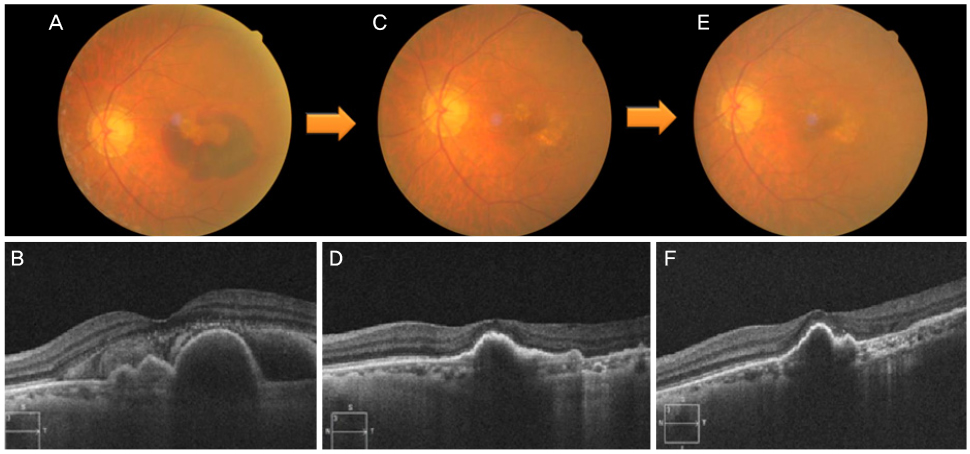
The mean preoperative BCVA was 0.79 ± 0.59 logMAR, which improved significantly to 0.53 ± 0.46 logMAR at 3 months and 0.48 ± 0.50 logMAR at 6 months (p < 0.001, in both). The CMT significantly decreased in all eyes: preoperative, 454.4 ± 131.5 µm, to 242.6 ± 39.7 µm at 6 months. The SMH was also reduced in all eyes: preoperative, 6.4 ± 4.8 disc areas (DAs) to 0.8 ± 1.4 DAs at 6 months. Ten eyes were diagnosed with typical nAMD (18.5%) and 44 eyes were diagnosed polypoidal choroidal vasculopathy (81.5%). There was no significant difference at 6 months in the visual outcomes of the subgroups.
CONCLUSIONS
Intravitreal aflibercept monotherapy is well-tolerated as a treatment in maintaining or improving vision in patients with SMH secondary to nAMD.
Keyword
MeSH Terms
Figure
Reference
-
1. Scupola A, Coscas G, Soubrane G, Balestrazzi E. Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999; 213:97–102.
Article2. Toth CA, Morse LS, Hjelmeland LM, Landers MB 3rd. Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch Ophthalmol. 1991; 109:723–729.
Article3. Lewis H. Intraoperative fibrinolysis of submacular hemorrhage with tissue plasminogen activator and surgical drainage. Am J Ophthalmol. 1994; 118:559–568.
Article4. Sarks SH. Ageing and degeneration in the macular region: a clinico-pathological study. Br J Ophthalmol. 1976; 60:324–341.
Article5. Berrocal MH, Lewis ML, Flynn HW Jr. Variations in the clinical course of submacular hemorrhage. Am J Ophthalmol. 1996; 122:486–493.
Article6. Schouten JS, La Heij EC, Webers CA, et al. A systematic review on the effect of bevacizumab in exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2009; 247:1–11.
Article7. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012; 119:2537–2548.
Article8. Browning DJ, Kaiser PK, Rosenfeld PJ, Stewart MW. Aflibercept for age-related macular degeneration: a game-changer or quiet addition? Am J Ophthalmol. 2012; 154:222–226.
Article9. Seddon JM, Sharma S, Adelman RA. Evaluation of the clinical age-related maculopathy staging system. Ophthalmology. 2006; 113:260–266.
Article10. Park KH, Song SJ, Lee WK, et al. The results of nation-wide registry of age-related macular degeneration in Korea. J Korean Ophthalmol Soc. 2010; 51:516–523.11. Cho H, Shah CP, Weber M, Heier JS. Aflibercept for exudative AMD with persistent fluid on ranibizumab and/or bevacizumab. Br J Ophthalmol. 2013; 97:1032–1035.
Article12. Kim JH, Cho NC, Kim WJ. Intravitreal aflibercept for neovascular age-related macular degeneration resistant to bevacizumab and ranibizumab. J Korean Ophthalmol Soc. 2015; 56:1359–1364.
Article13. Cho HJ, Koh KM, Kim HS, et al. Anti-vascular endothelial growth factor monotherapy in the treatment of submacular hemorrhage secondary to polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013; 156:524–531.
Article14. Kim KH, Kim JH, Chang YS, et al. Clinical outcomes of eyes with submacular hemorrhage secondary to age-related macular degeneration treated with anti-vascular endothelial growth factor. Korean J Ophthalmol. 2015; 29:315–324.
Article15. Kim HS, Cho HJ, Yoo SG, et al. Intravitreal anti-vascular endothelial growth factor monotherapy for large submacular hemorrhage secondary to neovascular age-related macular degeneration. Eye (Lond). 2015; 29:1141–1151.
Article16. Cho HJ, Koh KM, Kim JH, et al. Intravitreal ranibizumab injections with and without pneumatic displacement for treating submacular hemorrhage secondary to neovascular age-related macular degeneration. Retina. 2015; 35:205–212.
Article17. Holash J, Davis S, Papadopoulos N, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci U S A. 2002; 99:11393–11398.
Article18. Zhang Y, Chioreso C, Schweizer ML, Abràmoff MD. Effects of aflibercept for neovascular age-related macular degeneration: a systematic review and meta-analysis of observational comparative studies. Invest Ophthalmol Vis Sci. 2017; 58:5616–5627.19. Shin KH, Lee TG, Kim JH, et al. The efficacy of intravitreal aflibercept in submacular hemorrhage secondary to wet age-related macular degeneration. Korean J Ophthalmol. 2016; 30:369–376.
Article20. Yamamoto A, Okada AA, Kano M, et al. One-year results of intravitreal aflibercept for polypoidal choroidal vasculopathy. Ophthalmology. 2015; 122:1866–1872.
Article21. Iacono P, Parodi MB, Introini U, et al. Intravitreal ranibizumab for choroidal neovascularization with large submacular hemorrhage in age-related macular degeneration. Retina. 2014; 34:281–287.
Article22. Kim JH, Chang YS, Kim JW, et al. Intravitreal anti-vascular endothelial growth factor for submacular hemorrhage from choroidal neovascularization. Ophthalmology. 2014; 121:926–935.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Intravitreal Aflibercept in Submacular Hemorrhage Secondary to Wet Age-related Macular Degeneration
- Intravitreal Tissue Plasminogen Activator and Gas Injection in Submacular Hemorrhage
- Intravitreal Aflibercept for Neovascular Age-Related Macular Degeneration Resistant to Bevacizumab and Ranibizumab
- Intravitreal Injection of tPA and Gas for Submacular Hemorrhage Associated with Age-related Macular Degeneration
- Outcome of Aflibercept-Bevacizumab Alternate Dosing in Neovascular Age-related Macular Degeneration with Limited Response to Aflibercept