Korean J Pain.
2018 Apr;31(2):109-115. 10.3344/kjp.2018.31.2.109.
The outcome of epiduroscopy treatment in patients with chronic low back pain and radicular pain, operated or non-operated for lumbar disc herniation: a retrospective study in 88 patients
- Affiliations
-
- 1Department of Neurosurgery, Faculty of Medicine, Mugla Sitki Kocman University, Mugla, Turkey. burcuhazer@hotmail.com
- 2Department of Translational Medicine-Hand Surgery, Skane University Hospital, Lund University, Malmö, Sweden.
- KMID: 2410833
- DOI: http://doi.org/10.3344/kjp.2018.31.2.109
Abstract
- BACKGROUND
Patients with lumbar disc herniation are treated with physiotherapy/medication and some with surgery. However, even after technically successful surgery some develop a failed back syndrome with persistent pain. Our aim was to evaluate the efficacy of epiduroscopy in patients who suffer chronic low back pain and/or radicular pain with or without surgery and the gender difference in outcome.
METHODS
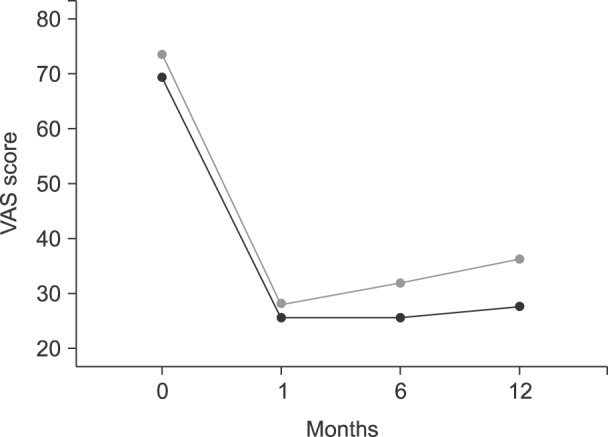
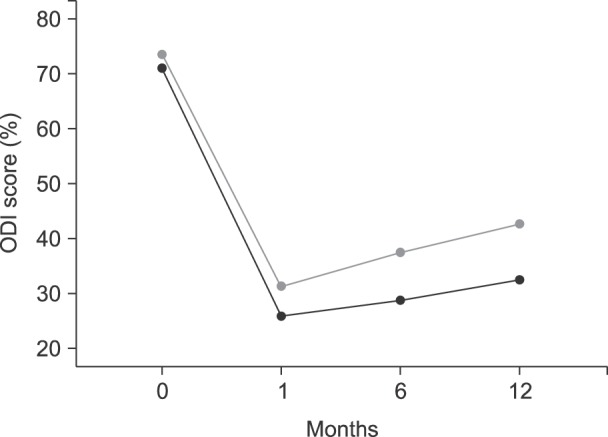
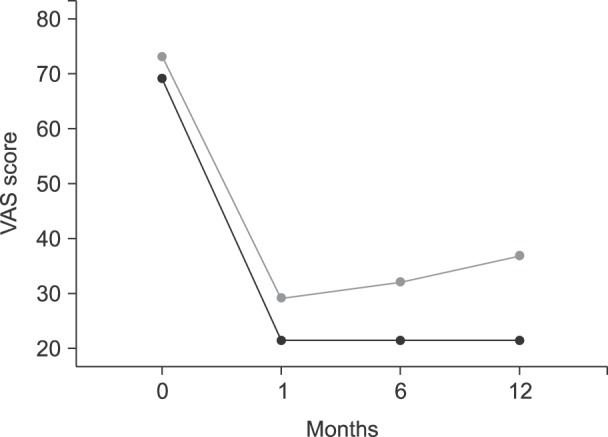
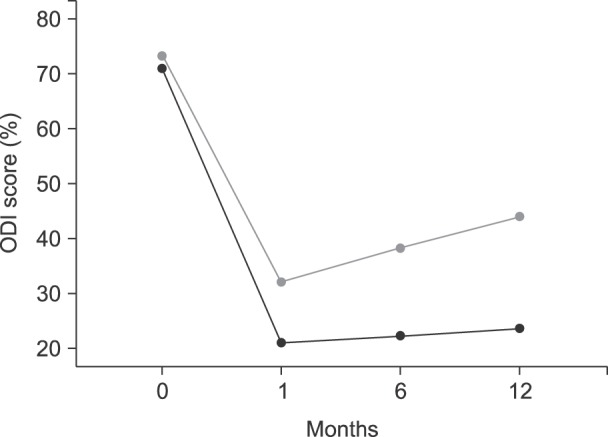
A total of 88 patients were included with a mean age of 52 years (27-82), 54 women and 34 men. 66 of them were operated previously and 22 were non-operated. They all had persistent chronic back pain and radicular pain despite of medication and physical rehabilitation. Visual Analog Scale (VAS) for pain and Oswestry Disability Index (ODI) were evaluated preoperatively, after one month, six months and one-year after the epiduroscopy.
RESULTS
All patients, and also the subgroups (gender and operated/non-operated) improved significantly in pain (VAS) and disability (ODI) at one month. A significant improvement was also seen at one year. No differences were found between men and woman at the different follow-up times. A slight worsening in VAS and ODI was noticed over time except for the non-operated group.
CONCLUSIONS
Epiduroscopy helps to improve the back and leg pain due to lumbar disc herniation in the early stage. At one year an improvement still exists, and the non-operated group seems to benefit most of the procedure.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The role of percutaneous neurolysis in lumbar disc herniation: systematic review and meta-analysis
Laxmaiah Manchikanti, Emilija Knezevic, Nebojsa Nick Knezevic, Mahendra R. Sanapati, Alan D. Kaye, Srinivasa Thota, Joshua A. Hirsch
Korean J Pain. 2021;34(3):346-368. doi: 10.3344/kjp.2021.34.3.346.Complication of epiduroscopy: a brief review and case report
Maurizio Marchesini, Edoardo Flaviano, Valentina Bellini, Marco Baciarello, Elena Giovanna Bignami
Korean J Pain. 2018;31(4):296-304. doi: 10.3344/kjp.2018.31.4.296.
Reference
-
1. Rabinovitch DL, Peliowski A, Furlan AD. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. 2009; 9:509–517. PMID: 19398387.
Article2. Overdevest GM, Vleggeert Lankamp CL, Jacobs WC, Brand R, Koes BW, Peul WC. Recovery of motor deficit accompanying sciatica--subgroup analysis of a randomized controlled trial. Spine J. 2014; 14:1817–1824. PMID: 24200407.
Article3. Leveque JC, Villavicencio AT, Bulsara KR, Rubin L, Gorecki JP. Spinal cord stimulation for failed back surgery syndrome. Neuromodulation. 2001; 4:1–9. PMID: 22151565.
Article4. Jo DH, Kim ED, Oh HJ. The comparison of the result of epiduroscopic laser neural decompression between FBSS or not. Korean J Pain. 2014; 27:63–67. PMID: 24478903.
Article. Schutze G. Epiduroscopy: spinal endoscopy. Heidelberg: Springer;2008. p. 12–16.6. Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003; 4:407–414. PMID: 14622683.
Article7. Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980; 66:271–273. PMID: 6450426.8. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000; 25:2940–2952. PMID: 11074683.
Article9. Miyamoto H, Saura R, Harada T, Doita M, Mizuno K. The role of cyclooxygenase-2 and inflammatory cytokines in pain induction of herniated lumbar intervertebral disc. Kobe J Med Sci. 2000; 46:13–28. PMID: 11193500.10. Lee GW, Jang SJ, Kim JD. The efficacy of epiduroscopic neural decompression with Ho:YAG laser ablation in lumbar spinal stenosis. Eur J Orthop Surg Traumatol. 2014; 24(Suppl 1):S231–S237. PMID: 24398702.
Article11. Di Donato A, Fontana C, Alemanno D, Di Giacomo A. Epiduroscopy in treatment of degenerative chronic low back pain: a prospective analysis and follow-up at 60 months. Clin Res Regul Aff. 2010; 27:69–74.
Article12. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15. PMID: 24478895.
Article13. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013; 16:185–196. PMID: 23703406.14. Kallewaard JW, Vanelderen P, Richardson J, Van Zundert J, Heavner J, Groen GJ. Epiduroscopy for patients with lumbosacral radicular pain. Pain Pract. 2014; 14:365–377. PMID: 23941663.
Article15. Ryu KS, Rathi NK, Kim G, Park CK. Iatrogenic intradural lumbosacral cyst following epiduroscopy. J Korean Neurosurg Soc. 2012; 52:491–494. PMID: 23323173.
Article16. Dullerud R, Graver V, Haakonsen M, Haaland AK, Loeb M, Magnaes B. Influence of fibrinolytic factors on scar formation after lumbar discectomy. A magnetic resonance imaging follow-up study with clinical correlation performed 7 years after surgery. Spine (Phila Pa 1976). 1998; 23:1464–1469. PMID: 9670398.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Addendum: The outcome of epiduroscopy treatment in patients with chronic low back pain and radicular pain, operated or nonoperated for lumbar disc herniation: a retrospective study in 88 patients
- Lumbar Disc Screening Using Back Pain Questionnaires: Oswestry Low Back Pain Score, Aberdeen Low Back Pain Scale, and Acute Low Back Pain Screening Questionnaire
- The Comparison of the Result of Epiduroscopic Laser Neural Decompression between FBSS or Not
- The Effects of Epiduroscopy in Spinal Stenosis: A case report
- The Relationship between Lumbar Shape and Lumbar Disc Herniation