Investig Clin Urol.
2018 May;59(3):187-193. 10.4111/icu.2018.59.3.187.
Prostate calcifications: A case series supporting the microbial biofilm theory
- Affiliations
-
- 1Department of Urology, Santa Chiara Regional Hospital, Trento, Italy. ktommy@libero.it
- 2Department of Industrial Engineering, University of Trento, Trento, Italy.
- 3Healthcare Research and Innovation Program (IRCS-PAT), Bruno Kessler Foundation, Trento, Italy.
- 4Department of Laboratory Medicine, Azienda Provinciale per i Servizi Sanitari, Trento, Italy.
- 5Sexually Transmitted Disease Centre, Santa Maria Annunziata Hospital, Florence, Italy.
- 6Department of Urology, University of Naples, Naples, Italy.
- 7Department of Urology, Oslo University Hospital, Oslo, Norway.
- KMID: 2410592
- DOI: http://doi.org/10.4111/icu.2018.59.3.187
Abstract
- PURPOSE
Prostate calcifications are a common finding during transrectal prostate ultrasound in both healthy subjects and patients, but their etiopathogenesis and clinical significance are not fully understood. We aimed to establish a new methodology for evaluating the role of microbial biofilms in the genesis of prostate calcifications.
MATERIALS AND METHODS
Ten consecutive patients who had undergone radical prostatectomy were enrolled in this study. All of the patients presented with prostate calcifications during transrectal ultrasound evaluation before surgery and underwent Meares-Stamey tests and clinical evaluation with the National Institutes of Health Chronic Prostatitis Symptom Index and the International Prostate Symptom Score. At the time of radical prostatectomy, the prostate specimen, after removal, was analyzed with ultrasonography under sterile conditions in the operating room. Core biopsy specimens were taken from the site of prostate calcification and subjected to ultrastructural and microbiological analysis.
RESULTS
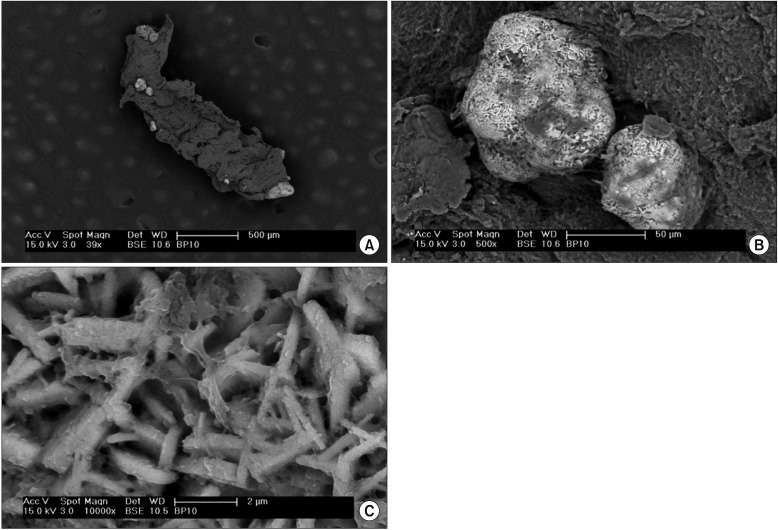
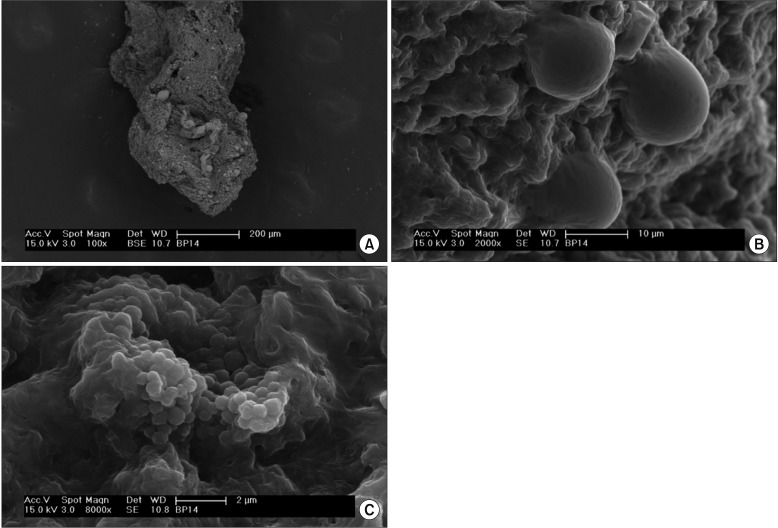
The results of the Meares-Stamey test showed only 1 of 10 patients (10%) with positive cultures for Escherichia coli. Two of five patients (40%) had positive cultures from prostate biopsy specimens. Enterococcus faecalis, Enterococcus raffinosus, and Citrobacter freundii were isolated. Ultrastructural analysis of the prostate biopsy specimens showed prostate calcifications in 6 of 10 patients (60%), and a structured microbial biofilm in 1 patient who had positive cultures for E. faecalis and E. raffinosus.
CONCLUSIONS
Although the findings are supported by a low number of patients, this study highlights the validity of the proposed methodology for investigating the role of bacterial biofilms in the genesis of prostate calcification.
Keyword
MeSH Terms
Figure
Reference
-
1. Yang HJ, Huang KH, Wang CW, Chang HC, Yang TK. Prostate calcification worsen lower urinary tract symptoms in middle-aged men. Urology. 2013; 81:1320–1324. PMID: 23561714.
Article2. Suh JH, Gardner JM, Kee KH, Shen S, Ayala AG, Ro JY. Calcifications in prostate and ejaculatory system: a study on 298 consecutive whole mount sections of prostate from radical prostatectomy or cystoprostatectomy specimens. Ann Diagn Pathol. 2008; 12:165–170. PMID: 18486891.
Article3. Torres Ramírez C, Aguilar Ruiz J, Zuluaga Gómez A, del Río Sámper S, Issa Khozouz N. Structure of primary prostatic endogenous calculi. Arch Esp Urol. 1979; 32:581–590. PMID: 556206.4. Sfanos KS, Wilson BA, De Marzo AM, Isaacs WB. Acute inflammatory proteins constitute the organic matrix of prostatic corpora amylacea and calculi in men with prostate cancer. Proc Natl Acad Sci U S A. 2009; 106:3443–3448. PMID: 19202053.
Article5. Geramoutsos I, Gyftopoulos K, Perimenis P, Thanou V, Liagka D, Siamblis D, et al. Clinical correlation of prostatic lithiasis with chronic pelvic pain syndromes in young adults. Eur Urol. 2004; 45:333–337. PMID: 15036679.
Article6. Klimas R, Bennett B, Gardner WA Jr. Prostatic calculi: a review. Prostate. 1985; 7:91–96. PMID: 3909127.
Article7. Shoskes DA, Lee CT, Murphy D, Kefer J, Wood HM. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2007; 70:235–238. PMID: 17826477.
Article8. Kanamaru S, Kurazono H, Terai A, Monden K, Kumon H, Mizunoe Y, et al. Increased biofilm formation in Escherichia coli isolated from acute prostatitis. Int J Antimicrob Agents. 2006; 28:S21–S25. PMID: 16828264.
Article9. Bartoletti R, Cai T, Nesi G, Albanese S, Meacci F, Mazzoli S, et al. The impact of biofilm-producing bacteria on chronic bacterial prostatitis treatment: results from a longitudinal cohort study. World J Urol. 2014; 32:737–742. PMID: 23918259.
Article10. Giubilei G, Mondaini N, Crisci A, Raugei A, Lombardi G, Travaglini F, et al. The Italian version of the National Institutes of Health Chronic Prostatitis Symptom Index. Eur Urol. 2005; 47:805–811. PMID: 15925077.
Article11. Badía X, García-Losa M, Dal-Ré R. Ten-language translation and harmonization of the International Prostate Symptom Score: developing a methodology for multinational clinical trials. Eur Urol. 1997; 31:129–140. PMID: 9076454.12. Mazzoli S, Cai T, Rupealta V, Gavazzi A, Castricchi Pagliai R, Mondaini N, et al. Interleukin 8 and anti-chlamydia trachomatis mucosal IgA as urogenital immunologic markers in patients with C. trachomatis prostatic infection. Eur Urol. 2007; 51:1385–1393. PMID: 17107749.
Article13. Cai T, Wagenlehner FM, Mazzoli S, Meacci F, Mondaini N, Nesi G, et al. Semen quality in patients with Chlamydia trachomatis genital infection treated concurrently with prulifloxacin and a phytotherapeutic agent. J Androl. 2012; 33:615–623. PMID: 21979301.
Article14. Cai T, Caola I, Tessarolo F, Piccoli F, D'Elia C, Caciagli P, et al. Solidago, orthosiphon, birch and cranberry extracts can decrease microbial colonization and biofilm development in indwelling urinary catheter: a microbiologic and ultrastructural pilot study. World J Urol. 2014; 32:1007–1014. PMID: 24092275.
Article15. Cai T, Tiscione D, Caola I, Tessarolo N, Mondaini F, Meacci G, et al. Prostate calcifications and LUTS: the potential role of bacterial biofilm and prostate inflammation. Eur Urol Suppl. 2014; 13:e561.16. Thomas BA, Robert JT. Prostatic calculi. J Urol. 1927; 18:470–493.
Article17. Finkle AL. The relationship of antecedent genito-urinary infections to the development of prostatic calculi and carcinoma. Bull N Y Acad Med. 1953; 29:585–586. PMID: 13051704.18. Eykyn S, Bultitude MI, Mayo ME, Lloyd-Davies RW. Prostatic calculi as a source of recurrent bacteriuria in the male. Br J Urol. 1974; 46:527–532. PMID: 4609168.
Article19. Meares EM Jr. Infection stones of prostate gland. Laboratory diagnosis and clinical management. Urology. 1974; 4:560–566. PMID: 4215187.20. Dessombz A, Méria P, Bazin D, Daudon M. Prostatic stones: evidence of a specific chemistry related to infection and presence of bacterial imprints. PLoS One. 2012; 7:e51691. PMID: 23272143.
Article21. Soto SM, Smithson A, Martinez JA, Horcajada JP, Mensa J, Vila J. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J Urol. 2007; 177:365–368. PMID: 17162092.
Article22. Lewis K. Multidrug tolerance of biofilms and persister cells. Curr Top Microbiol Immunol. 2008; 322:107–131. PMID: 18453274.
Article23. Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microrganisms. Clin Microbiol Rev. 2002; 15:167–193. PMID: 11932229.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Urinary Catheter Materials on Forming Biofilms of Microorganisms
- A periodontitis-associated multispecies model of an oral biofilm
- Susceptibility of Mutans streptococci in the Planktonic and Biofilm State to Erythrosine
- Invasive potential of biofilm-forming Staphylococci bovine subclinical mastitis isolates
- Primary Lymphosarcoma of the Prostate Gland