Ann Surg Treat Res.
2018 May;94(5):262-269. 10.4174/astr.2018.94.5.262.
Anatomical popliteal artery entrapment syndrome
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. twkwon2@amc.seoul.kr
- 2Department of Surgery, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- 3Department of Anatomy, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2410270
- DOI: http://doi.org/10.4174/astr.2018.94.5.262
Abstract
- PURPOSE
The aim of this study was to analyze anatomical popliteal artery entrapment syndrome (PAES) and to individualize the treatment of this condition according to the anatomical status of the artery and the adjacent structure.
METHODS
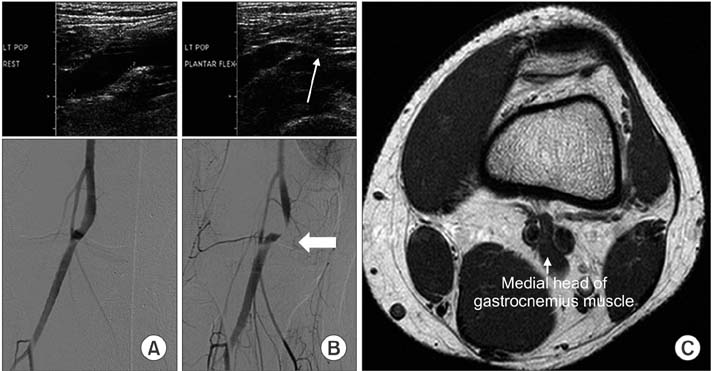
A total of 35 anatomical PAES legs in 23 consecutive patients treated within the Asan Medical Center, Seoul, Korea between 1995 and 2011 were analyzed retrospectively. Anatomical PAES was diagnosed by MRI and/or CT scans of the knee joint, and CT or conventional transfemoral arteriography of the lower extremities.
RESULTS
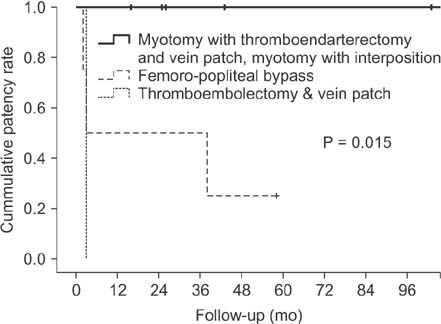
We noted a type II gastrocnemius medial head (GNM) anomaly, a type III GNM anomaly, or an aberrant plantaris muscle in 51.4%, 20%, and 28.6% of PAES legs, respectively. In assessments of the arterial lesions, popliteal or tibial artery occlusion was noted in 19 of 26 symptomatic PAES legs. For cases without popliteal artery lesions, myotomy of the anatomically deranged muscle was performed in 5 of 7 symptomatic and 4 of 9 asymptomatic PAES legs. For occluded popliteal arteries, we performed ten direct repairs of the pathological popliteal artery and 4 femoro-below the knee popliteal bypass surgeries. As a result of the arterial Surgery, 9 direct procedures with myotomy yielded a patent artery, while 3 graft failures were noted in the bypass group. The median follow-up period was 84 months (range, 12-206 months).
CONCLUSION
We recommend that treatment of PAES should be individualized based on pathology, symptoms, and various imaging studies.
Keyword
MeSH Terms
Figure
Reference
-
1. Insua JA, Young JR, Humphries AW. Popliteal artery entrapment syndrome. Arch Surg. 1970; 101:771–775.
Article2. Delaney TA, Gonzalez LL. Occlusion of popliteal artery due to muscular entrapment. Surgery. 1971; 69:97–101.3. Rich NM, Collins GJ Jr, McDonald PT, Kozloff L, Clagett GP, Collins JT. Popliteal vascular entrapment. Its increasing interest. Arch Surg. 1979; 114:1377–1384.4. di Marzo L, Cavallaro A, Sciacca V, Mingoli A, Tamburelli A. Surgical treatment of popliteal artery entrapment syndrome: a ten-year experience. Eur J Vasc Surg. 1991; 5:59–64.
Article5. Turnipseed WD. Popliteal entrapment syndrome. J Vasc Surg. 2002; 35:910–915.
Article6. Liu PT, Moyer AC, Huettl EA, Fowl RJ, Stone WM. Popliteal vascular entrapment syndrome caused by a rare anomalous slip of the lateral head of the gastrocnemius muscle. Skeletal Radiol. 2005; 34:359–363.
Article7. Kim HK, Shin MJ, Kim SM, Lee SH, Hong HJ. Popliteal artery entrapment syndrome: morphological classification utilizing MR imaging. Skeletal Radiol. 2006; 35:648–658.
Article8. Levien LJ, Veller MG. Popliteal artery entrapment syndrome: more common than previously recognized. J Vasc Surg. 1999; 30:587–598.
Article9. Pillai J, Levien LJ, Haagensen M, Candy G, Cluver MD, Veller MG. Assessment of the medial head of the gastrocnemius muscle in functional compression of the popliteal artery. J Vasc Surg. 2008; 48:1189–1196.
Article10. Turnipseed WD, Pozniak M. Popliteal entrapment as a result of neurovascular compression by the soleus and plantaris muscles. J Vasc Surg. 1992; 15:285–293.
Article11. di Marzo L, Cavallaro A. Popliteal vascular entrapment. World J Surg. 2005; 29:Suppl 1. S43–S45.12. Kwon YJ, Kwon TW, Um EH, Shin S, Cho YP, Kim JM, et al. Anatomical popliteal artery entrapment syndrome caused by an aberrant plantaris muscle. Vasc Specialist Int. 2015; 31:95–101.
Article13. Murray A, Halliday M, Croft RJ. Popliteal artery entrapment syndrome. Br J Surg. 1991; 78:1414–1419.
Article14. Chernoff DM, Walker AT, Khorasani R, Polak JF, Jolesz FA. Asymptomatic functional popliteal artery entrapment: demonstration at MR imaging. Radiology. 1995; 195:176–180.
Article15. Collins PS, McDonald PT, Lim RC. Popliteal artery entrapment: an evolving syndrome. J Vasc Surg. 1989; 10:484–489.
Article