J Korean Ophthalmol Soc.
2018 Apr;59(4):301-306. 10.3341/jkos.2018.59.4.301.
Surgical Outcomes of Endonasal Dacryocystorhinostomy According to the Level of Obstruction in Dacryocystography
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Medical School, Jeonju, Korea. ahnmin@jbnu.ac.kr
- 2Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 3Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2409676
- DOI: http://doi.org/10.3341/jkos.2018.59.4.301
Abstract
- PURPOSE
The success of endonasal dacryocystorhinostomy was assessed according to the level of tear duct obstruction in dacryocystography.
METHODS
Patients visited our clinic with the chief complaint of epiphora between January 2009 and September 2016 who received dacryocystography and were diagnosed with a total nasolacrimal obstruction. Among these patients, 128 eyes from 115 patients who received endonasal dacryocystorhinostomy were selected and their medical records from > 6-month follow-ups were analyzed retrospectively. The patients were divided into four groups according to the level of lacrimal passage obstruction in dacryocystography: common canaliculus obstruction as group 1, lacrimal sac obstruction as group 2, lacrimal sac-nasolacrimal duct junction obstruction as group 3, and nasolacrimal duct obstruction as group 4. Success and failure were determined according to symptom improvements after surgery.
RESULTS
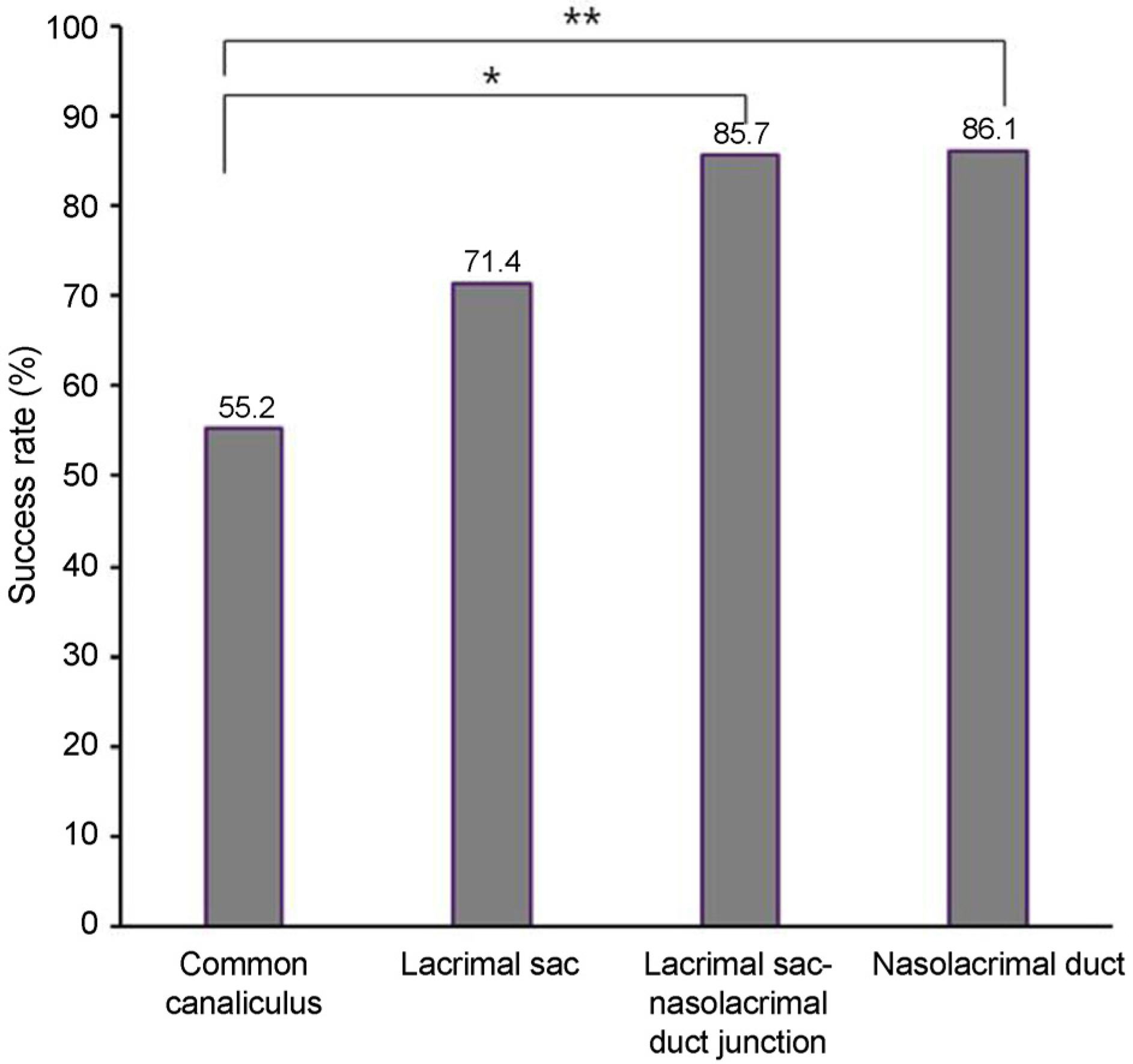
Among the total of 128 eyes, 19 eyes were categorized as group 1 (22.6%), 28 eyes as group 2 (21.9%), 28 eyes as group 3 (21.9%), and 43 eyes as group 4 (33.6%). Nasolacrimal duct obstruction was the most common condition. The success of endonasal dacryocystorhinostomy was 55.2% in group 1, 71.4% in group 2, 85.7% in group 3, and 86.1% in group 4. The surgical success of the patient group with common canaliculus obstruction was significantly lower than the surgical success of the lacrimal sac-nasolacrimal duct junction obstruction and nasolacrimal duct obstruction groups (p = 0.03 and p = 0.01, respectively).
CONCLUSIONS
Determination of the accurate position of obstruction using preoperative dacryocystography is recommended for patients with epiphora caused by tear duct obstruction because this predicted the effects of endonasal dacryocystorhinostomy.
MeSH Terms
Figure
Reference
-
1). Baek SK, Ha MS. Analysis of the results endonasal dacryocystorhinostomy related to nasal cavity state. J Korean Ophthalmol Soc. 2014; 55:633–9.
Article2). Kwon YA, Kim HC, Ha MS, et al. Success rates according to the shape of rhinostomy after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2009; 50:14–8.
Article3). Shin HM, Lew H, Yun YS. Surgical result of endoscopic dacryocystorhinostomy according to opening size of nasal mucosa. J Korean Ophthalmol Soc. 2006; 47:175–80.4). Kim J, Kim H. Characteristics in patients with and without previous dacryocystitis and satisfaction after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2017; 58:1–6.
Article5). Shin IH, Lim HB, Lee JJ, Lee SB. Prognostic factors for successful endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2015; 56:1661–6.
Article6). Park HI, Lee KW, Kang SM. Prognostic factors associated with surgical time of endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2017; 58:757–62.
Article7). Jung JJ, Jang SY, Jang JW, In JH. Comparison result of silicone tube intubation according to syringing and dacryocystography. J Korean Ophthalmol Soc. 2014; 55:1584–8.8). Jeong HW, Cho NC, Ahn M. Result of silicone tube intubation in patients with epiphora who showing normal finding in dacryocystography. J Korean Ophthalmol Soc. 2008; 49:706–12.
Article9). Nemet AY. The etiology of epiphora: a multifactorial issue. Semin Ophthalmol. 2016; 31:275–9.
Article10). Ewing AE. Roentogen ray demonstrations of the lacrimal abscess cavity. Am J Ophthalmol. 1909; 26:1–4.11). Kim CH, Lew H, Yun YS. Correspodence among the canaliculus irrigation test, dacryocystography and Jones test in the epiphora patients. J Korean Ophthalmol Soc. 2007; 48:1017–22.12). Kim JS, Ahn M. Clinical evaluation and classification of nasolacrimal duct obstruction site by dacryocystography. J Korean Ophthalmol Soc. 2005; 46:191–5.13). Kim TH, Lee JH, Ahn JH, et al. Dacryocystographic findings in unilateral epiphora with patent lacrimal drainage system. J Korean Ophthalmol Soc. 2013; 54:839–44.
Article14). Lee DP, Yang SW, Choi WC. The relation between nasal cavity size and success rate in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2000; 41:1118–23.15). Lee YJ, Moon SW, Cho HY, Jeong JH. Clinical outcome of dacryocystorhinostomy with septal deviation. J Korean Ophthalmol Soc. 2008; 49:713–20.
Article16). Lim IS, Jeong SK, Park YG. A study of factors related to surgical success rate of dacyocystorhinostomy. J Korean Ophthalmol Soc. 1997; 38:1322–7.17). Dave TV, Mohammed FA, Ali MJ, Naik MN. Etiologic analysis of 100 anatomically failed dacryocystorhinostomies. Clinical Ophthalmol. 2016; 10:1419–22.18). Lee HC, Chung WS. Success rate of endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 1996; 37:211–8.19). Kim JH, Kim JM, Woo KI. The role of dacryocystography in evaluation of nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2006; 47:1713–9.20). Nomura K, Arakawa K, Sugawara M, et al. Factors influencing endoscopic dacryocystorhinostomy outcome. Eur Arch Otorhinolaryngol. 2017; 274:2773–7.
Article21). Yung MW, Hardman-Lea S. Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol. 2002; 86:792–4.
Article22). Choi JC, Jin HR, Moon YE, et al. The surgical outcome of endoscopic dacryocystorhinostomy according to the obstruction levels of lacrimal drainage system. Clin Exp Otorhinolaryngol. 2009; 2:141–4.
Article23). Rose GE. The lacrimal paradox: toward a greater understanding of success in lacrimal surgery. Ophthal Plast Reconstr Surg. 2004; 20:262–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcomes of Endonasal Dacryocystorhinostomy with Canalicular Trephination in Canalicular Obstruction
- Clinical Experience of Lacrimal Surgery
- Surgical Outcomes of Dacryocystorhinostomy in Lacrimal Drainage Obstruction after Systemic Chemotherapy or Radioactive Iodine Therapy
- The Clinical Study of Lacrimal Sump Syndrome after Endonasal Dacryocystorhinostomy
- Classification of Nasolacrimal Duct Obstruction According to Dacryocystographic Finding and Its Clinical Ssignificance