Allergy Asthma Immunol Res.
2018 May;10(3):189-206. 10.4168/aair.2018.10.3.189.
Allergen-Specific Immunotherapies for Food Allergy
- Affiliations
-
- 1Division of Pediatric Pulmonology, Allergy, and Immunology, Department of Pediatrics, Weill Cornell Medicine, New York, NY, USA.
- 2Division of Pediatric Allergy and Immunology, Department of Pediatrics, Jaffe Food Allergy Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA. anna.nowak-wegrzyn@mssm.edu
- KMID: 2409054
- DOI: http://doi.org/10.4168/aair.2018.10.3.189
Abstract
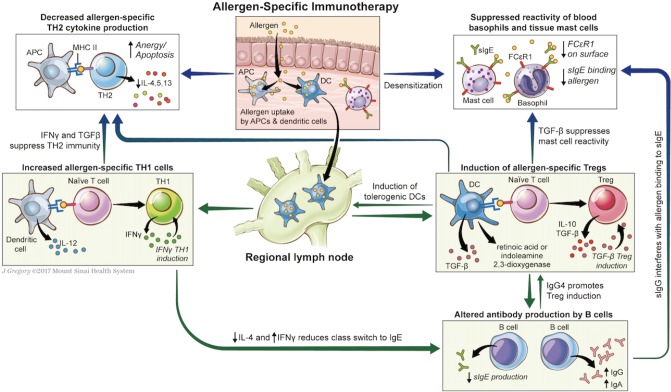
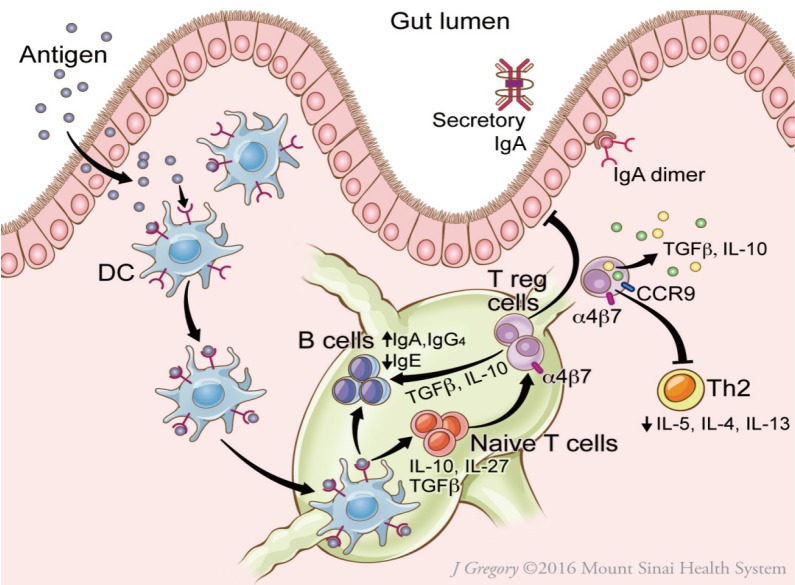
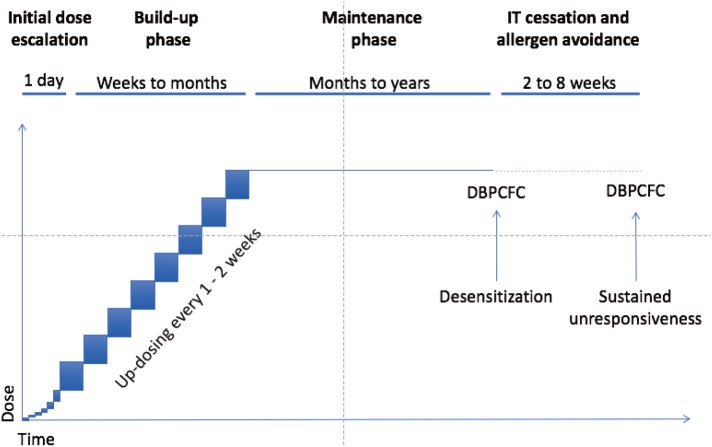
- With rising prevalence of food allergy (FA), allergen-specific immunotherapy (AIT) for FA has become an active area of research in recent years. In AIT, incrementally increasing doses of inciting allergen are given with the goal to increase tolerance, initially through desensitization, which relies on regular exposure to allergen. With prolonged therapy in some subjects, AIT may induce sustained unresponsiveness, in which tolerance is retained after a period of allergen avoidance. Methods of AIT currently under study in humans include oral, sublingual, epicutaneous, and subcutaneous delivery of modified allergenic protein, as well as via DNA-based vaccines encoding allergen with lysosomal-associated membrane protein I. The balance of safety and efficacy varies by type of AIT, as well as by targeted allergen. Age, degree of sensitization, and other comorbidities may affect this balance within an individual patient. More recently, AIT with modified proteins or combined with immunomodulatory therapies has shown promise in making AIT safer and/or more effective. Though methods of AIT are neither currently advised by experts (oral immunotherapy [OIT]) nor widely available, AIT is likely to become a part of recommended management of FA in the coming years. Here, we review and compare methods of AIT currently under study in humans to prepare the practitioner for an exciting new phase in the care of food allergic patients in which improved tolerance to inciting foods will be a real possibility.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Hyperresponsiveness to Boiled Egg Yolk in Early Life Leads to Prolonged Egg Allergy
Satoshi Horino, Hiroshi Kitazawa, Taiki Satou, Katsushi Miura
Allergy Asthma Immunol Res. 2019;11(3):433-437. doi: 10.4168/aair.2019.11.3.433.Subcutaneous Immunotherapy in Patients with Fagales Pollen-Induced Oral Allergy Syndrome
Nasil Kong, Sunyoung Kim, Sang Chul Lee, Kyung Hee Park, Jae-Hyun Lee, Jung-Won Park
Yonsei Med J. 2019;60(4):389-394. doi: 10.3349/ymj.2019.60.4.389.
Reference
-
1. Nwaru BI, Hickstein L, Panesar SS, Roberts G, Muraro A, Sheikh A, et al. Prevalence of common food allergies in Europe: a systematic review and meta-analysis. Allergy. 2014; 69:992–1007. PMID: 24816523.
Article2. Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009; 124:1549–1555. PMID: 19917585.
Article3. Sicherer SH, Muñoz-Furlong A, Godbold JH, Sampson HA. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol. 2010; 125:1322–1326. PMID: 20462634.
Article4. Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014; 134:1016–1025.e43. PMID: 25174862.5. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128:e9–e17. PMID: 21690110.
Article6. Jones SM, Sicherer SH, Burks AW, Leung DY, Lindblad RW, Dawson P, et al. Epicutaneous immunotherapy for the treatment of peanut allergy in children and young adults. J Allergy Clin Immunol. 2017; 139:1242–1252.e9. PMID: 28091362.
Article7. Jones SM, Agbotounou WK, Fleischer DM, Burks AW, Pesek RD, Harris MW, et al. Safety of epicutaneous immunotherapy for the treatment of peanut allergy: a phase 1 study using the Viaskin patch. J Allergy Clin Immunol. 2016; 137:1258–1261.e10. PMID: 26920463.8. Jongejan L, van Ree R, Poulsen LK. Hypoallergenic molecules for subcutaneous immunotherapy. Expert Rev Clin Immunol. 2016; 12:5–7. PMID: 26558320.
Article9. Berin MC, Sampson HA. Mucosal immunology of food allergy. Curr Biol. 2013; 23:R389–R400. PMID: 23660362.
Article10. Jay DC, Nadeau KC. Immune mechanisms of sublingual immunotherapy. Curr Allergy Asthma Rep. 2014; 14:473. PMID: 25195100.
Article11. Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol. 2008; 8:523–532. PMID: 18566595.
Article12. Vickery BP, Berglund JP, Burk CM, Fine JP, Kim EH, Kim JI, et al. Early oral immunotherapy in peanut-allergic preschool children is safe and highly effective. J Allergy Clin Immunol. 2017; 139:173–181.e8. PMID: 27522159.
Article13. Kim EH, Bird JA, Kulis M, Laubach S, Pons L, Shreffler W, et al. Sublingual immunotherapy for peanut allergy: clinical and immunologic evidence of desensitization. J Allergy Clin Immunol. 2011; 127:640–646.e1. PMID: 21281959.
Article14. Blumchen K, Ulbricht H, Staden U, Dobberstein K, Beschorner J, de Oliveira LC, et al. Oral peanut immunotherapy in children with peanut anaphylaxis. J Allergy Clin Immunol. 2010; 126:83–91.e1. PMID: 20542324.
Article15. Varshney P, Jones SM, Scurlock AM, Perry TT, Kemper A, Steele P, et al. A randomized controlled study of peanut oral immunotherapy: clinical desensitization and modulation of the allergic response. J Allergy Clin Immunol. 2011; 127:654–660. PMID: 21377034.
Article16. Vickery BP, Scurlock AM, Jones SM, Burks AW. Mechanisms of immune tolerance relevant to food allergy. J Allergy Clin Immunol. 2011; 127:576–584. PMID: 21277624.
Article17. Vickery BP, Pons L, Kulis M, Steele P, Jones SM, Burks AW. Individualized IgE-based dosing of egg oral immunotherapy and the development of tolerance. Ann Allergy Asthma Immunol. 2010; 105:444–450. PMID: 21130382.
Article18. Akdis CA, Akdis M. Mechanisms of allergen-specific immunotherapy. J Allergy Clin Immunol. 2011; 127:18–27. PMID: 21211639.19. Wambre E, DeLong JH, James EA, Torres-Chinn N, Pfützner W, Möbs C, et al. Specific immunotherapy modifies allergen-specific CD4(+) T-cell responses in an epitope-dependent manner. J Allergy Clin Immunol. 2014; 133:872–879.e7. PMID: 24373351.
Article20. Wawrzyniak M, O'Mahony L, Akdis M. Role of regulatory cells in oral tolerance. Allergy Asthma Immunol Res. 2017; 9:107–115. PMID: 28102055.
Article21. Patil SU, Ogunniyi AO, Calatroni A, Tadigotla VR, Ruiter B, Ma A, et al. Peanut oral immunotherapy transiently expands circulating Ara h 2-specific B cells with a homologous repertoire in unrelated subjects. J Allergy Clin Immunol. 2015; 136:125–134.e12. PMID: 25985925.
Article22. Jones SM, Pons L, Roberts JL, Scurlock AM, Perry TT, Kulis M, et al. Clinical efficacy and immune regulation with peanut oral immunotherapy. J Allergy Clin Immunol. 2009; 124:292–300. 300.e1–300.e97. PMID: 19577283.
Article23. Syed A, Garcia MA, Lyu SC, Bucayu R, Kohli A, Ishida S, et al. Peanut oral immunotherapy results in increased antigen-induced regulatory T-cell function and hypomethylation of forkhead box protein 3 (FOXP3). J Allergy Clin Immunol. 2014; 133:500–510. PMID: 24636474.
Article24. Keet CA, Frischmeyer-Guerrerio PA, Thyagarajan A, Schroeder JT, Hamilton RG, Boden S, et al. The safety and efficacy of sublingual and oral immunotherapy for milk allergy. J Allergy Clin Immunol. 2012; 129:448–455. 455.e1–455.e5. PMID: 22130425.
Article25. Vickery BP, Lin J, Kulis M, Fu Z, Steele PH, Jones SM, et al. Peanut oral immunotherapy modifies IgE and IgG4 responses to major peanut allergens. J Allergy Clin Immunol. 2013; 131:128–134. 134.e1–134.e3. PMID: 23199605.26. Narisety SD, Frischmeyer-Guerrerio PA, Keet CA, Gorelik M, Schroeder J, Hamilton RG, et al. A randomized, double-blind, placebo-controlled pilot study of sublingual versus oral immunotherapy for the treatment of peanut allergy. J Allergy Clin Immunol. 2015; 135:1275–1282. 1282.e1–1282.e6. PMID: 25528358.
Article27. Gorelik M, Narisety SD, Guerrerio Al. Chichester KL, Keet CA, Bieneman AP, et al. Suppression of the immunologic response to peanut during immunotherapy is often transient. J Allergy Clin Immunol. 2015; 135:1283–1292. PMID: 25542883.28. Perezábad L, Reche M, Valbuena T, López-Fandiño R, Molina E, López-Expósito I. Oral Food desensitization in children with IgE-mediated cow's milk allergy: immunological changes underlying desensitization. Allergy Asthma Immunol Res. 2017; 9:35–42. PMID: 27826960.
Article29. Nagai Y, Shiraishi D, Tanaka Y, Nagasawa Y, Ohwada S, Shimauchi H, et al. Transportation of sublingual antigens across sublingual ductal epithelial cells to the ductal antigen-presenting cells in mice. Clin Exp Allergy. 2015; 45:677–686. PMID: 24773115.
Article30. Allam JP, Würtzen PA, Reinartz M, Winter J, Vrtala S, Chen KW, et al. Phl p 5 resorption in human oral mucosa leads to dose-dependent and time-dependent allergen binding by oral mucosal Langerhans cells, attenuates their maturation, and enhances their migratory and TGF-beta1 and IL-10-producing properties. J Allergy Clin Immunol. 2010; 126:638–645.e1. PMID: 20584546.31. Burks AW, Wood RA, Jones SM, Sicherer SH, Fleischer DM, Scurlock AM, et al. Sublingual immunotherapy for peanut allergy: long-term follow-up of a randomized multicenter trial. J Allergy Clin Immunol. 2015; 135:1240–1248. 1248.e1–1248.e3. PMID: 25656999.
Article32. Dioszeghy V, Mondoulet L, Dhelft V, Ligouis M, Puteaux E, Benhamou PH, et al. Epicutaneous immunotherapy results in rapid allergen uptake by dendritic cells through intact skin and downregulates the allergen-specific response in sensitized mice. J Immunol. 2011; 186:5629–5637. PMID: 21490160.
Article33. Tordesillas L, Mondoulet L, Blazquez AB, Benhamou PH, Sampson HA, Berin MC. Epicutaneous immunotherapy induces gastrointestinal LAP+ regulatory T cells and prevents food-induced anaphylaxis. J Allergy Clin Immunol. 2017; 139:189–201.e4. PMID: 27417020.34. Dupont C, Kalach N, Soulaines P, Legoué-Morillon S, Piloquet H, Benhamou PH. Cow's milk epicutaneous immunotherapy in children: a pilot trial of safety, acceptability, and impact on allergic reactivity. J Allergy Clin Immunol. 2010; 125:1165–1167. PMID: 20451043.35. Jonuleit H, Schmitt E, Schuler G, Knop J, Enk AH. Induction of interleukin 10-producing, nonproliferating CD4(+) T cells with regulatory properties by repetitive stimulation with allogeneic immature human dendritic cells. J Exp Med. 2000; 192:1213–1222. PMID: 11067871.
Article36. Freidl R, Gstoettner A, Baranyi U, Swoboda I, Stolz F, Focke-Tejkl M, et al. Blocking antibodies induced by immunization with a hypoallergenic parvalbumin mutant reduce allergic symptoms in a mouse model of fish allergy. J Allergy Clin Immunol. 2017; 139:1897–1905.e1. PMID: 27876628.
Article37. Zuidmeer-Jongejan L, Huber H, Swoboda I, Rigby N, Versteeg SA, Jensen BM, et al. Development of a hypoallergenic recombinant parvalbumin for first-in-man subcutaneous immunotherapy of fish allergy. Int Arch Allergy Immunol. 2015; 166:41–51. PMID: 25765512.
Article38. Bindslev-Jensen C, de Kam PJ, van Twuijver E, Boot DB, El Galta R, Mose AP, et al. SCIT-treatment with a chemically modified, aluminum hydroxide adsorbed peanut extract (HAL-MPE1) was generally safe and well tolerated and showed immunological changes in peanut allergic patients. J Allergy Clin Immunol. 2017; 139:AB191.
Article39. Liu MA. DNA vaccines: an historical perspective and view to the future. Immunol Rev. 2011; 239:62–84. PMID: 21198665.
Article40. Su Y, Connolly M, Marketon A, Heiland T. CryJ-LAMP DNA vaccines for Japanese red cedar allergy induce robust TH1-type immune responses in murine model. J Immunol Res. 2016; 2016:4857869. PMID: 27239481.41. Burks AW, Jones SM, Wood RA, Fleischer DM, Sicherer SH, Lindblad RW, et al. Oral immunotherapy for treatment of egg allergy in children. N Engl J Med. 2012; 367:233–243. PMID: 22808958.
Article42. Vickery BP, Scurlock AM, Kulis M, Steele PH, Kamilaris J, Berglund JP, et al. Sustained unresponsiveness to peanut in subjects who have completed peanut oral immunotherapy. J Allergy Clin Immunol. 2014; 133:468–475. PMID: 24361082.
Article43. Hsiao KC, Ponsonby Al, Axelrad C, Pitkin S, Tang ML, Burks W, et al. Long-term clinical and immunological effects of probiotic and peanut oral immunotherapy after treatment cessation: 4-year follow-up of a randomised, double-blind, placebo-controlled trial. Lancet Child Adolesc Health. 2017; 1:97–105.
Article44. Nadeau KC, Schneider LC, Hoyte L, Borras I, Umetsu DT. Rapid oral desensitization in combination with omalizumab therapy in patients with cow's milk allergy. J Allergy Clin Immunol. 2011; 127:1622–1624. PMID: 21546071.
Article45. Skripak JM, Nash SD, Rowley H, Brereton NH, Oh S, Hamilton RG, et al. A randomized, double-blind, placebo-controlled study of milk oral immunotherapy for cow's milk allergy. J Allergy Clin Immunol. 2008; 122:1154–1160. PMID: 18951617.
Article46. Rodríguez del Río P, Díaz-Perales A, Sanchez-García S, Escudero C, do Santos P, Catarino M, et al. Oral immunotherapy in children with IgE-mediated wheat allergy: outcome and molecular changes. J Investig Allergol Clin Immunol. 2014; 24:240–248.47. MacGinnitie AJ, Rachid R, Gragg H, Little SV, Lakin P, Cianferoni A, et al. Omalizumab facilitates rapid oral desensitization for peanut allergy. J Allergy Clin Immunol. 2017; 139:873–881.e8. PMID: 27609658.
Article48. Lucendo AJ, Arias A, Tenias JM. Relation between eosinophilic esophagitis and oral immunotherapy for food allergy: a systematic review with meta-analysis. Ann Allergy Asthma Immunol. 2014; 113:624–629. PMID: 25216976.
Article49. Anagnostou K, Islam S, King Y, Foley L, Pasea L, Bond S, et al. Assessing the efficacy of oral immunotherapy for the desensitisation of peanut allergy in children (STOP II): a phase 2 randomised controlled trial. Lancet. 2014; 383:1297–1304. PMID: 24485709.
Article50. Shaker MS. An economic analysis of a peanut oral immunotherapy study in children. J Allergy Clin Immunol Pract. 2017; 5:1707–1716. PMID: 28606784.
Article51. Martorell-Calatayud C, Michavila-Gómez A, Martorell-Aragonés A, Molini-Menchón N, Cerdá-Mir JC, Félix-Toledo R, et al. Anti-IgE-assisted desensitization to egg and cow's milk in patients refractory to conventional oral immunotherapy. Pediatr Allergy Immunol. 2016; 27:544–546. PMID: 27003835.
Article52. Bégin P, Dominguez T, Wilson SP, Bacal L, Mehrotra A, Kausch B, et al. Phase 1 results of safety and tolerability in a rush oral immunotherapy protocol to multiple foods using omalizumab. Allergy Asthma Clin Immunol. 2014; 10:7. PMID: 24576338.
Article53. Narisety SD, Skripak JM, Steele P, Hamilton RG, Matsui EC, Burks AW, et al. Open-label maintenance after milk oral immunotherapy for IgE-mediated cow's milk allergy. J Allergy Clin Immunol. 2009; 124:610–612. PMID: 19665770.
Article54. Wood RA, Kim JS, Lindblad R, Nadeau K, Henning AK, Dawson P, et al. A randomized, double-blind, placebo-controlled study of omalizumab combined with oral immunotherapy for the treatment of cow's milk allergy. J Allergy Clin Immunol. 2016; 137:1103–1110.e11. PMID: 26581915.
Article55. Schneider LC, Rachid R, LeBovidge J, Blood E, Mittal M, Umetsu DT. A pilot study of omalizumab to facilitate rapid oral desensitization in high-risk peanut-allergic patients. J Allergy Clin Immunol. 2013; 132:1368–1374. PMID: 24176117.
Article56. Tang ML, Ponsonby Al. Orsini F, Tey D, Robinson M, Su EL, et al. Administration of a probiotic with peanut oral immunotherapy: a randomized trial. J Allergy Clin Immunol. 2015; 135:737–744.e8. PMID: 25592987.57. Wang J, Jones SM, Pongracic JA, Song Y, Yang N, Sicherer SH, et al. Safety, clinical. and immunologic efficacy of a Chinese herbal medicine (Food Allergy Herbal Formula-2) for food allergy. J Allergy Clin Immunol. 2015; 136:962–970.e1. PMID: 26044855.
Article58. Enrique E, Pineda F, Malek T, Bartra J, Basagaña M, Tella R, et al. Sublingual immunotherapy for hazelnut food allergy: a randomized, double-blind, placebo-controlled study with a standardized hazelnut extract. J Allergy Clin Immunol. 2005; 116:1073–1079. PMID: 16275379.
Article59. Fleischer DM, Burks AW, Vickery BP, Scurlock AM, Wood RA, Jones SM, et al. Sublingual immunotherapy for peanut allergy: a randomized, double-blind, placebo-controlled multicenter trial. J Allergy Clin Immunol. 2013; 131:119–127. 127.e1–127.e7. PMID: 23265698.60. Béné J, Ley D, Roboubi R, Gottrand F, Gautier S. Eosinophilic esophagitis after desensitization to dust mites with sublingual immunotherapy. Ann Allergy Asthma Immunol. 2016; 116:583–584. PMID: 27067457.
Article61. Miehlke S, Alpan O, Schröder S, Straumann A. Induction of eosinophilic esophagitis by sublingual pollen immunotherapy. Case Rep Gastroenterol. 2013; 7:363–368. PMID: 24163646.
Article62. Oppenheimer JJ, Nelson HS, Bock SA, Christensen F, Leung DY. Treatment of peanut allergy with rush immunotherapy. J Allergy Clin Immunol. 1992; 90:256–262. PMID: 1500630.
Article63. Nelson HS, Lahr J, Rule R, Bock A, Leung D. Treatment of anaphylactic sensitivity to peanuts by immunotherapy with injections of aqueous peanut extract. J Allergy Clin Immunol. 1997; 99:744–751. PMID: 9215240.64. Wood RA, Sicherer SH, Burks AW, Grishin A, Henning AK, Lindblad R, et al. A phase 1 study of heat/phenol-killed, E. coli-encapsulated, recombinant modified peanut proteins Ara h 1, Ara h 2, and Ara h 3 (EMP-123) for the treatment of peanut allergy. Allergy. 2013; 68:803–808. PMID: 23621498.65. Wasserman RL, Factor JM, Baker JW, Mansfield LE, Katz Y, Hague AR, et al. Oral immunotherapy for peanut allergy: multipractice experience with epinephrine-treated reactions. J Allergy Clin Immunol Pract. 2014; 2:91–96. PMID: 24565775.
Article66. Peters RL, Dharmage SC, Gurrin LC, Koplin JJ, Ponsonby Al. Lowe AJ, et al. The natural history and clinical predictors of egg allergy in the first 2 years of life: a prospective, population-based cohort study. J Allergy Clin Immunol. 2014; 133:485–491. PMID: 24373356.67. Kim JS, Nowak-Węgrzyn A, Sicherer SH, Noone S, Moshier EL, Sampson HA. Dietary baked milk accelerates the resolution of cow's milk allergy in children. J Allergy Clin Immunol. 2011; 128:125–131.e2. PMID: 21601913.
Article68. Virkud YV, Burks AW, Steele PH, Edwards LJ, Berglund JP, Jones SM, et al. Novel baseline predictors of adverse events during oral immunotherapy in children with peanut allergy. J Allergy Clin Immunol. 2017; 139:882–888.e5. PMID: 27609653.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A practical view of immunotherapy for food allergy
- Diagnosis of food allergies: the impact of oral food challenge testing
- Clinical Significance and Interpretation of Allergen-Specific IgE Testing in Regard to Food Allergy
- Skin and oral intervention for food allergy prevention based on dual allergen exposure hypothesis
- Recent advances in food allergen immunotherapy