Korean J Ophthalmol.
2018 Apr;32(2):95-102. 10.3341/kjo.2017.0111.
Lamina Cribrosa Changes after Laser In Situ Keratomileusis in Myopic Eyes
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ckee@skku.edu
- KMID: 2408948
- DOI: http://doi.org/10.3341/kjo.2017.0111
Abstract
- PURPOSE
To determine deep optic nerve head structure changes after transient intraocular pressure elevation during laser in situ keratomileusis (LASIK) for myopia.
METHODS
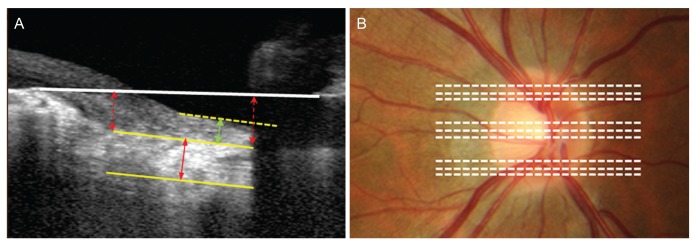
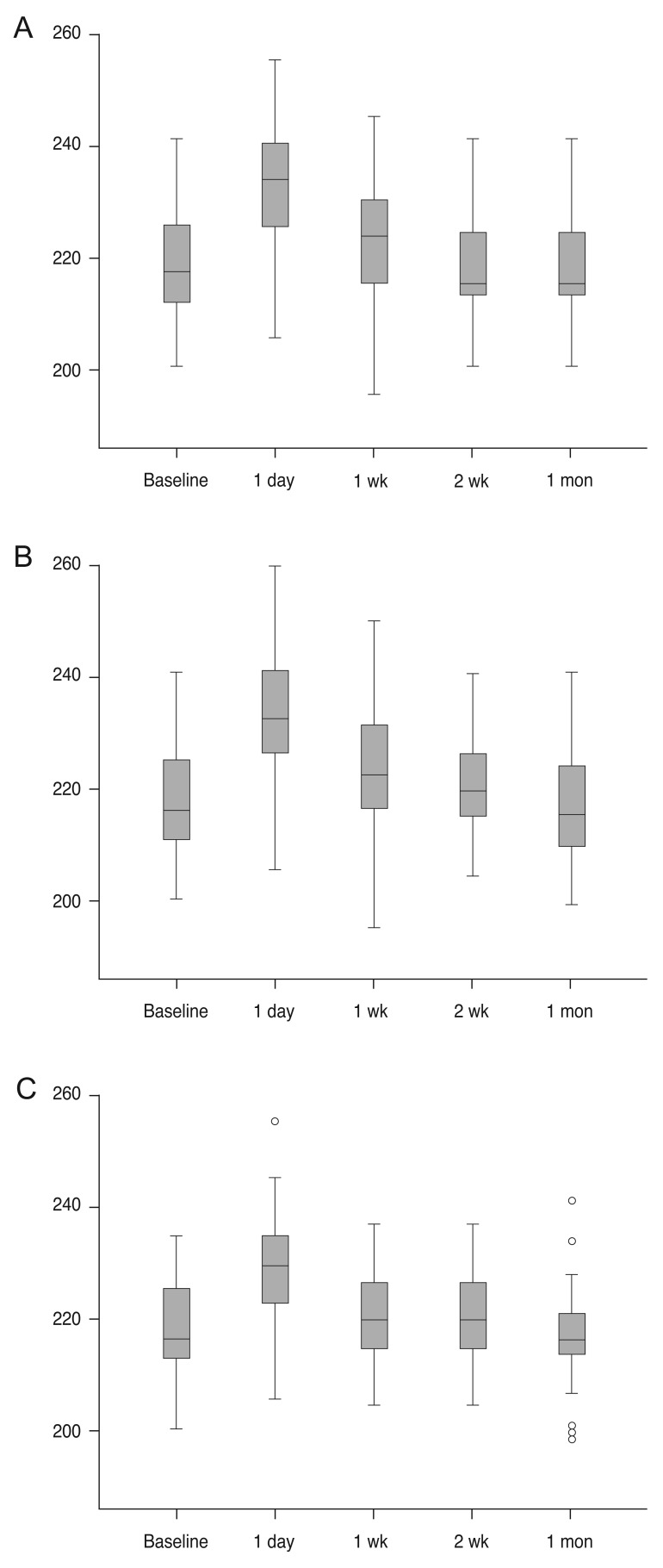
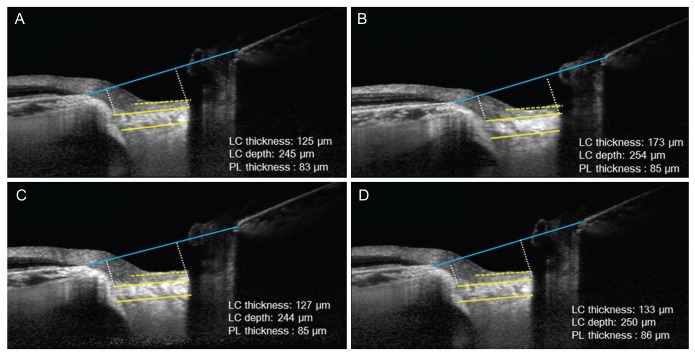
Enhanced depth imaging-optical coherence tomography was performed in each myopic eye that underwent LASIK surgery. Enhanced depth imaging-optical coherence tomography images were created at postoperative 1 day, 1 week, 2 weeks, and 1 month. Lamina cribrosa (LC) thickness, LC depth and prelaminar thickness at the superior, middle and inferior portions of the optic nerve head were measured by two investigators.
RESULTS
Forty eyes in 40 patients were included in the present study. During follow-up, there were no significant differences in prelaminar thickness or LC depth. The LC demonstrated increased thickness at postoperative 1 day at all three locations (superior, middle, and inferior) (p < 0.001, p < 0.001, p < 0.001, respectively). However, no significant changes were observed at postoperative 1 week, 2 weeks, and 1 month.
CONCLUSIONS
The LC thickness could increase at 1 day after LASIK surgery. However, the thickness will gradually return to baseline morphology. Temporary intraocular pressure increase during LASIK does not appear to induce irreversible LC thickness changes.
MeSH Terms
Figure
Reference
-
1. Yuen LH, Chan WK, Koh J, et al. A 10-year prospective audit of LASIK outcomes for myopia in 37,932 eyes at a single institution in Asia. Ophthalmology. 2010; 117:1236–1244. PMID: 20153899.
Article2. Chan KC, Poostchi A, Wong T, et al. Visual field changes after transient elevation of intraocular pressure in eyes with and without glaucoma. Ophthalmology. 2008; 115:667–672. PMID: 17716733.
Article3. Lleo-Perez A, Sanchis Gimeno J. Changes in the visual field following laser in situ keratomileusis for myopia. Ophthalmic Physiol Opt. 2007; 27:201–209. PMID: 17324211.4. Quigley HA, Addicks EM, Green WR, Maumenee AE. Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol. 1981; 99:635–649. PMID: 6164357.5. Minckler DS, Bunt AH, Johanson GW. Orthograde and retrograde axoplasmic transport during acute ocular hypertension in the monkey. Invest Ophthalmol Vis Sci. 1977; 16:426–441. PMID: 67096.6. Kasetsuwan N, Pangilinan RT, Moreira LL, et al. Real time intraocular pressure and lamellar corneal flap thickness in keratomileusis. Cornea. 2001; 20:41–44. PMID: 11189002.
Article7. Han JC, Choi DY, Kwun YK, et al. Evaluation of lamina cribrosa thickness and depth in ocular hypertension. Jpn J Ophthalmol. 2016; 60:14–19. PMID: 26361960.
Article8. Bernstein SL, Johnson MA, Miller NR. Nonarteritic anterior ischemic optic neuropathy (NAION) and its experimental models. Prog Retin Eye Res. 2011; 30:167–187. PMID: 21376134.
Article9. Cameron BD, Saffra NA, Strominger MB. Laser in situ keratomileusis-induced optic neuropathy. Ophthalmology. 2001; 108:660–665. PMID: 11297479.
Article10. Maden A, Yilmaz S, Yurdakul NS. Nonarteritic ischemic optic neuropathy after LASIK with femtosecond laser flap creation. J Neuroophthalmol. 2008; 28:242–243. PMID: 18769298.
Article11. Smith BT, Park CH, Fekrat S. Hemi-retinal vein occlusion following LASIK. Ann Ophthalmol (Skokie). 2006; 38:139–140. PMID: 17416945.
Article12. Lee AG, Kohnen T, Ebner R, et al. Optic neuropathy associated with laser in situ keratomileusis. J Cataract Refract Surg. 2000; 26:1581–1584. PMID: 11084263.
Article13. Shaikh NM, Shaikh S, Singh K, Manche E. Progression to end-stage glaucoma after laser in situ keratomileusis. J Cataract Refract Surg. 2002; 28:356–359. PMID: 11821221.
Article14. Bushley DM, Parmley VC, Paglen P. Visual field defect associated with laser in situ keratomileusis. Am J Ophthalmol. 2000; 129:668–671. PMID: 10844064.
Article15. Weiss HS, Rubinfeld RS, Anderschat JF. Case reports and small case series: LASIK-associated visual field loss in a glaucoma suspect. Arch Ophthalmol. 2001; 119:774–775. PMID: 11346411.16. Whitson JT, McCulley JP, Cavanagh HD, et al. Effect of laser in situ keratomileusis on optic nerve head topography and retinal nerve fiber layer thickness. J Cataract Refract Surg. 2003; 29:2302–2305. PMID: 14709290.
Article17. Hamada N, Kaiya T, Oshika T, et al. Optic disc and retinal nerve fiber layer analysis with scanning laser tomography after LASIK. J Refract Surg. 2006; 22:372–375. PMID: 16629070.
Article18. Zangwill LM, Abunto T, Bowd C, et al. Scanning laser polarimetry retinal nerve fiber layer thickness measurements after LASIK. Ophthalmology. 2005; 112:200–207. PMID: 15691551.
Article19. Kim YJ, Yun SC, Na JH, et al. Glaucoma progression in eyes with a history of refractive corneal surgery. Invest Ophthalmol Vis Sci. 2012; 53:4485–4489. PMID: 22695960.
Article20. Jonas JB, Jonas SB, Jonas RA, et al. Histology of the parapapillary region in high myopia. Am J Ophthalmol. 2011; 152:1021–1029. PMID: 21821229.
Article21. Park HY, Jeon SH, Park CK. Enhanced depth imaging detects lamina cribrosa thickness differences in normal tension glaucoma and primary open-angle glaucoma. Ophthalmology. 2012; 119:10–20. PMID: 22015382.
Article22. Kwun Y, Han JC, Kee C. Comparison of lamina cribrosa thickness in normal tension glaucoma patients with unilateral visual field defect. Am J Ophthalmol. 2015; 159:512–518. PMID: 25498357.
Article23. Roberts MD, Grau V, Grimm J, et al. Remodeling of the connective tissue microarchitecture of the lamina cribrosa in early experimental glaucoma. Invest Ophthalmol Vis Sci. 2009; 50:681–690. PMID: 18806292.
Article24. Yang H, Thompson H, Roberts MD, et al. Deformation of the early glaucomatous monkey optic nerve head connective tissue after acute IOP elevation in 3-D histomorphometric reconstructions. Invest Ophthalmol Vis Sci. 2011; 52:345–363. PMID: 20702834.
Article25. Ozdamar A, Ocakoglu O. Optic nerve head blood flow using scanning laser Doppler flowmetry after laser in situ keratomileusis. J Refract Surg. 2003; 19:433–437. PMID: 12899474.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lamina Cribrosa Thickness in the Fellow Eyes of Patients with Unilateral Retinal Vein Occlusion
- The Effect of Corticosteroid Treatment on Myopic Regression after Laser in situ Keratomileusis[LASIK]
- Ocular deviation after unilateral laser in situ keratomileusis
- The Effect of Corticosteroids on Myopic Regression after Laser in Situ Keratomileusis
- Management of Three Cases of Decentration after Laser In Situ Keratomileusis