Comparison Study of Outcomes of Deceased Donor Liver Transplantation before and after Korean Model for End-Stage Liver Disease (MELD) System: Single Center Experience
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. med9370@gmail.com
- KMID: 2408662
- DOI: http://doi.org/10.4285/jkstn.2018.32.1.7
Abstract
- BACKGROUND
In June of 2016, the Model for End-Stage Liver Disease (MELD)-based allocation system replaced the Child-Turcotte-Pugh (CTP) score-based system for deceased donor liver transplantation (DDLT) in Korea. This study was conducted to reveal the changes before and after the MELD system.
METHODS
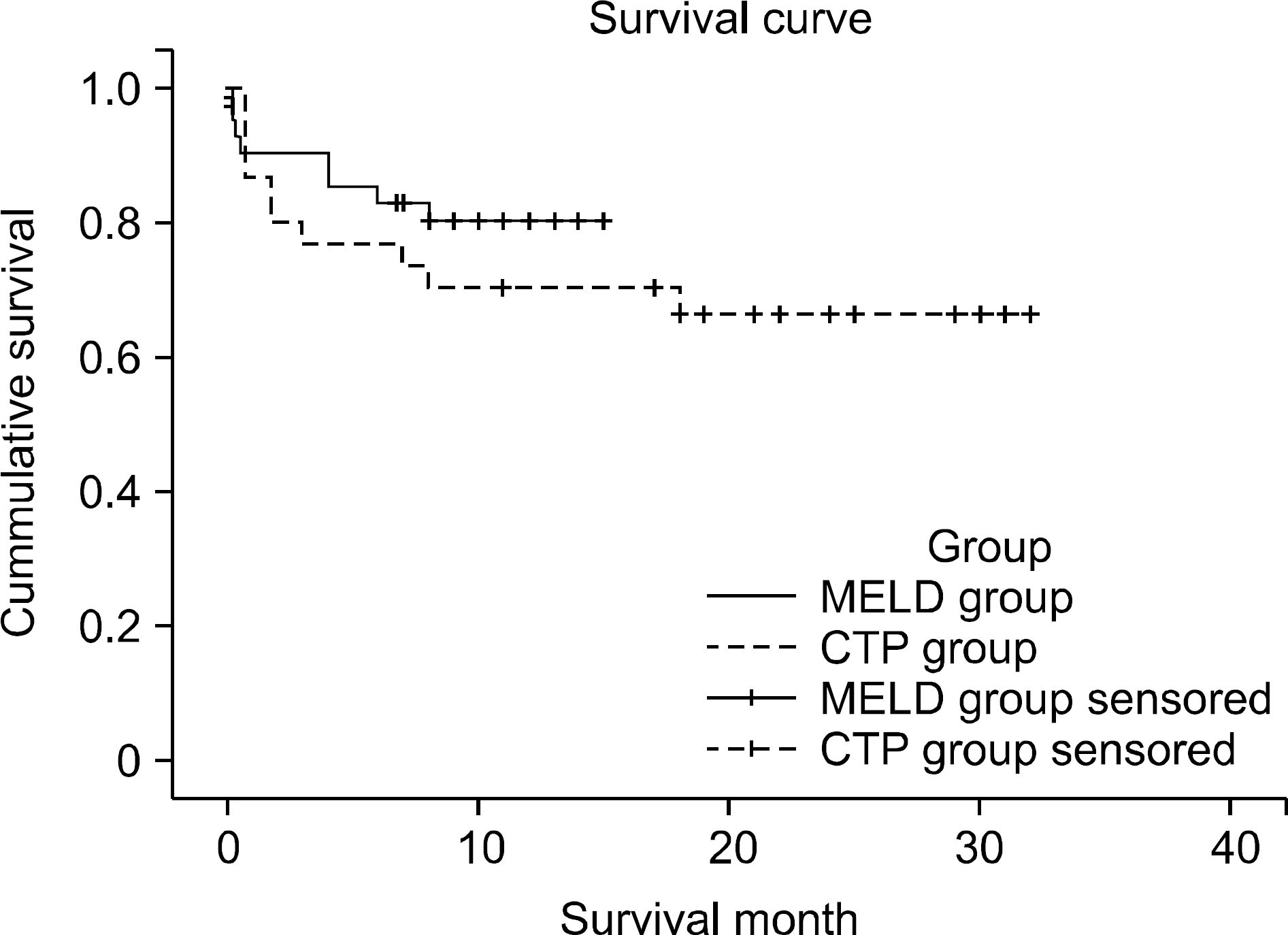
From January 2015 to March 2017, 71 patient datapoints were collected from recipients who underwent DDLT in a single center. Patients were divided into two groups according to the allocation system (41 in the MELD group, 30 in the CTP group).
RESULTS
The MELD score of the two groups differed significantly (36.8±4.5 in the MELD group, 26.0±8.1 in the CTP group, P=0.001). There was no difference in etiology for liver transplantation, 6-month survival rate, or in-hospital stay. However, complication rate and re-admission rate within the first 3 months were higher in the MELD group (78%, 56%). No one received a DDLT because of an incentive system for hepatocellular carcinoma.
CONCLUSIONS
Despite the short-term follow-up period, the new allocation rule reflects the severity of the patients. Almost all patients who underwent DDLT when they had a high MELD score and then suffered from morbidity; however, this problem was associated with organ shortage, not the allocation system.
MeSH Terms
Figure
Cited by 3 articles
-
Current Status of Deceased Donor Liver Transplantation for Alcoholic Liver Disease in Korea in MELD Era
Dong Jin Joo
Korean J Gastroenterol. 2021;77(1):4-11. doi: 10.4166/kjg.2020.167.Impact of Model for End-Stage Liver Disease allocation system on outcomes of deceased donor liver transplantation: A single-center experience
Han Sang Park, Jeong-Moo Lee, Kwangpyo Hong, Eui Soo Han, Suk Kyun Hong, YoungRok Choi, Nam-Joon Yi, Kwang-Woong Lee, Kyung-Suk Suh
Ann Hepatobiliary Pancreat Surg. 2021;25(3):336-341. doi: 10.14701/ahbps.2021.25.3.336.The impact of Model for End-Stage Liver Disease score on deceased donor liver transplant outcomes in low volume liver transplantation center: a retrospective and single-center study
Doo-Ho Lee, Yeon Ho Park, Seok Won Choi, Kug Hyun Nam, Sang Tae Choi, Doojin Kim
Ann Surg Treat Res. 2021;101(6):360-367. doi: 10.4174/astr.2021.101.6.360.
Reference
-
1). Korean Network for Organ Sharing (KONOS). Korean law and regulation related with organ donation and transplantation [Internet]. Seoul: KONOS;c2014. [cited 2018 Mar 12]. Available from:. https://www.konos.go.kr/konosis/index.jsp.2). Wiesner RH., McDiarmid SV., Kamath PS., Edwards EB., Malinchoc M., Kremers WK, et al. MELD and PELD: application of survival models to liver allocation. Liver Transpl. 2001. 7:567–80.
Article3). Malinchoc M., Kamath PS., Gordon FD., Peine CJ., Rank J., ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000. 31:864–71.
Article4). Kim MS. Modification of emergency status in deceased donor liver allocation: evidence for Korean Model of End-stage Liver Disease (MELD) System. J Korean Soc Transplant. 2016. 30:51–8. (김명수. 간장 응급도 기준 개선방안 연구: 한국 형 멜드시스템의 학술적 배경. 대한이식학회지 2016;30;51-8.).
Article5). Dutkowski P., Oberkofler CE., Bechir M., Mullhaupt B., Geier A., Raptis DA, et al. The model for end-stage liver disease allocation system for liver transplantation saves lives, but increases morbidity and cost: a prospective outcome analysis. Liver Transpl. 2011. 17:674–84.
Article6). Cywinski JB., Mascha EJ., You J., Sessler DI., Kapural L., Argalious M, et al. Pre-transplant MELD and sodium MELD scores are poor predictors of graft failure and mortality after liver transplantation. Hepatol Int. 2011. 5:841–9.
Article7). Korean Network for Organ Sharing (KONOS). 2016 Annual data report [Internet]. Seoul: KONOS;c2014. [cited 2018 Mar 12]. Available from:. https://www.konos.go.kr/konosis/index.jsp.8). Kim MS., Lee KW., Whang S., Kwon CHD., You YK., Nah YW, et al. Research for modification of emergency status in deceased donor liver allocation: survival analysis of waiting patients for liver transplantation. J Korean Soc Transplant. 2014. 28:59–68. (김명수, 이광웅, 황신, 권준혁, 유 영경, 나양원, 등. 간장 응급도 기준 개선방안 연구: 간이식 대기자 의 생존분석. 대한이식학회지 2014;28: 59-68.).
Article9). Hong G., Lee KW., Suh S., Yoo T., Kim H., Park MS, et al. The model for end-stage liver disease score-based system predicts short term mortality better than the current Child-Turcotte-Pugh score-based allocation system during waiting for deceased liver transplantation. J Korean Med Sci. 2013. 28:1207–12.
Article10). Mazzaferro V., Regalia E., Doci R., Andreola S., Pulvirenti A., Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996. 334:693–9.
Article11). Freeman RB Jr., Gish RG., Harper A., Davis GL., Vierling J., Lieblein L, et al. Model for end-stage liver disease (MELD) exception guidelines: results and recommendations from the MELD Exception Study Group and Conference (MES SAGE) for the approval of patients who need liver transplantation with diseases not considered by the standard MELD formula. Liver Transpl. 2006. 12(12 Suppl 3):S128–36.12). Cheng SJ., Freeman RB Jr., Wong JB. Predicting the probability of progression-free survival in patients with small hepatocellular carcinoma. Liver Transpl. 2002. 8:323–8.
Article13). Organ Procurement and Transplantation Network (OPTN). Organ Procurement and Transplantation Network (OPTN) policies [Internet]. Richmond: OPTN;2014. [cited 2018 Mar 12]. Available from:. http://optn.transplant.hrsa.gov.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Deceased Donor Liver Transplantation for Alcoholic Liver Disease in Korea in MELD Era
- Impact of Model for End-Stage Liver Disease allocation system on outcomes of deceased donor liver transplantation: A single-center experience
- A study on differences in deceased donor liver transplantation before and after the introduction of the model for end-stage liver disease system: three low volume centers, multi-center trial
- The impact of Model for End-Stage Liver Disease score on deceased donor liver transplant outcomes in low volume liver transplantation center: a retrospective and singlecenter study
- Impact of MELD allocation system on the outcomes of deceased donor liver transplantation: a single-center experience