Yonsei Med J.
2018 May;59(3):397-405. 10.3349/ymj.2018.59.3.397.
Delta Neutrophil Index Is Associated with Vasculitis Activity and Risk of Relapse in ANCA-Associated Vasculitis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. sangwonlee@yuhs.ac
- 2Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2407863
- DOI: http://doi.org/10.3349/ymj.2018.59.3.397
Abstract
- PURPOSE
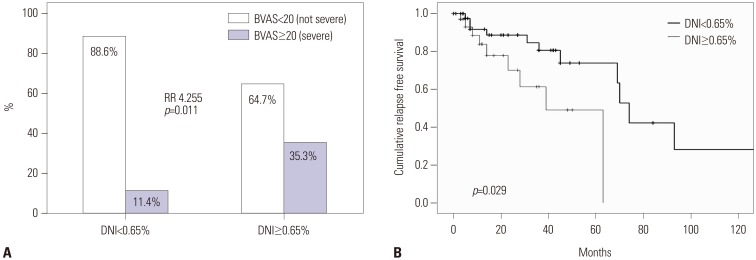
Delta neutrophil index (DNI) represents the immature granulocytes count associated with neutrophil-consumption. We investigated whether DNI might be associated with Birmingham vasculitis activity score (BVAS) at diagnosis and could predict relapse during the follow-up in patients with antineutrophil cytoplasmic antibody-associated vasculitis (AAV).
MATERIALS AND METHODS
We reviewed the medical records of 97 patients having DNI results. Twenty patients had granulomatosis with polyangiitis (GPA), 58 had microscopic polyangiitis (MPA), and 19 had eosinophilic GPA (EGPA). We collected clinical and laboratory data including BVAS, five factor score (FFS), and DNI. The correlation coefficient and cumulative relapse free survival rate were obtained. The optimal cut-off of DNI was extrapolated by calculating the area under the receiver operator characteristic curve.
RESULTS
DNI was significantly related to cross-sectional BVAS. Furthermore, among continuous variables, only DNI could reflect BVAS of GPA and MPA, but not EGPA. Severe AAV was defined as BVAS ≥20 (the highest quartile). At diagnosis, patients having DNI ≥0.65% had a significantly higher risk of severe GPA and MPA than those having not (relative risk 4.255) at diagnosis. During the follow-up, DNI ≥0.65% could predict the higher relapse rate.
CONCLUSION
DNI could reflect BVAS at diagnosis and furthermore, DNI ≥0.65% could not only identify severe AAV at diagnosis, but also predict relapse during the follow-up in patients with GPA and MPA.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Antineutrophil Cytoplasmic Antibody-Associated Vasculitis in Korea: A Narrative Review
Chan-Bum Choi, Yong-Beom Park, Sang-Won Lee
Yonsei Med J. 2019;60(1):10-21. doi: 10.3349/ymj.2019.60.1.10.Controlling Nutritional Status Score is Associated with All-Cause Mortality in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis
Sung Soo Ahn, Seung Min Jung, Jason Jungsik Song, Yong-Beom Park, Sang-Won Lee
Yonsei Med J. 2019;60(12):1164-1173. doi: 10.3349/ymj.2019.60.12.1164.
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013; 65:1–11. PMID: 23045170.
Article2. Millet A, Pederzoli-Ribeil M, Guillevin L, Witko-Sarsat V, Mouthon L. Antineutrophil cytoplasmic antibody-associated vasculitides: is it time to split up the group. Ann Rheum Dis. 2013; 72:1273–1279. PMID: 23606701.
Article3. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007; 66:222–227. PMID: 16901958.
Article4. Leavitt RY, Fauci AS, Bloch DA, Michel BA, Hunder GG, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum. 1990; 33:1101–1107. PMID: 2202308.
Article5. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990; 33:1094–1100. PMID: 2202307.
Article6. de Lind van Wijngaarden RA, van Rijn L, Hagen EC, Watts RA, Gregorini G, Tervaert JW, et al. Hypotheses on the etiology of antineutrophil cytoplasmic autoantibody associated vasculitis: the cause is hidden, but the result is known. Clin J Am Soc Nephrol. 2008; 3:237–252. PMID: 18077783.7. Jennette JC, Falk RJ. Pathogenesis of antineutrophil cytoplasmic autoantibody-mediated disease. Nat Rev Rheumatol. 2014; 10:463–473. PMID: 25003769.
Article8. Jennette JC, Falk RJ, Hu P, Xiao H. Pathogenesis of antineutrophil cytoplasmic autoantibody-associated small-vessel vasculitis. Annu Rev Pathol. 2013; 8:139–160. PMID: 23347350.
Article9. Honda T, Uehara T, Matsumoto G, Arai S, Sugano M. Neutrophil left shift and white blood cell count as markers of bacterial infection. Clin Chim Acta. 2016; 457:46–53. PMID: 27034055.
Article10. Field D, Taube E, Heumann S. Performance evaluation of the immature granulocyte parameter on the Sysmex XE-2100 automated hematology analyzer. Lab Hematol. 2006; 12:11–14. PMID: 16513542.
Article11. Nigro KG, O'Riordan M, Molloy EJ, Walsh MC, Sandhaus LM. Performance of an automated immature granulocyte count as a predictor of neonatal sepsis. Am J Clin Pathol. 2005; 123:618–624. PMID: 15743752.
Article12. Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci. 2008; 38:241–246. PMID: 18715852.13. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008; 36:309–332. PMID: 18538699.
Article14. Pyo JY, Park JS, Park YB, Lee SK, Ha YJ, Lee SW. Delta neutrophil index as a marker for differential diagnosis between flare and infection in febrile systemic lupus erythematosus patients. Lupus. 2013; 22:1102–1109. PMID: 23934401.
Article15. Park HJ, Ha YJ, Pyo JY, Park YB, Lee SK, Lee SW. Delta neutrophil index as an early marker for differential diagnosis of adult-onset Still’s disease and sepsis. Yonsei Med J. 2014; 55:753–759. PMID: 24719144.
Article16. Pyo JY, Ha YJ, Song JJ, Park YB, Lee SK, Lee SW. Delta neutrophil index contributes to the differential diagnosis between acute gout attack and cellulitis within 24 hours after hospitalization. Rheumatology (Oxford). 2017; 56:795–801. PMID: 28115599.
Article17. Csernok E, Moosig F. Current and emerging techniques for ANCA detection in vasculitis. Nat Rev Rheumatol. 2014; 10:494–501. PMID: 24890776.
Article18. Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis. 2009; 68:1827–1832. PMID: 19054820.
Article19. Stone JH, Hoffman GS, Merkel PA, Min YI, Uhlfelder ML, Hellmann DB, et al. A disease-specific activity index for Wegener's granulomatosis: modification of the Birmingham Vasculitis Activity Score. International Network for the Study of the Systemic Vasculitides (INSSYS). Arthritis Rheum. 2001; 44:912–920. PMID: 11318006.20. Gayraud M, Guillevin L, le Toumelin P, Cohen P, Lhote F, Casassus P, et al. Long-term followup of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome: analysis of four prospective trials including 278 patients. Arthritis Rheum. 2001; 44:666–675. PMID: 11263782.
Article21. Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Le Toumelin P. French Vasculitis Study Group (FVSG). assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore). 2011; 90:19–27. PMID: 21200183.22. Mukhtyar C, Hellmich B, Jayne D, Flossmann O, Luqmani R. Remission in antineutrophil cytoplasmic antibody-associated systemic vasculitis. Clin Exp Rheumatol. 2006; 24(6 Suppl 43):S-93-8.23. Mukhtyar C, Flossmann O, Hellmich B, Bacon P, Cid M, Cohen-Tervaert JW, et al. Outcomes from studies of antineutrophil cytoplasm antibody associated vasculitis: a systematic review by the European League Against Rheumatism systemic vasculitis task force. Ann Rheum Dis. 2008; 67:1004–1010. PMID: 17911225.
Article24. Oh YJ, Ahn SS, Park ES, Jung SM, Song JJ, Park YB, et al. Chest and renal involvements, Birmingham vascular activity score more than 13.5 and five factor score (1996) more than 1 at diagnosis are significant predictors of relapse of microscopic polyangiitis. Clin Exp Rheumatol. 2017; 35(Suppl 103):47–54.25. Yoo J, Kim HJ, Ahn SS, Jung SM, Song JJ, Park YB, et al. Clinical and prognostic features of Korean patients with MPO-ANCA, PR3-ANCA and ANCA-negative vasculitis. Clin Exp Rheumatol. 2017; 35(Suppl 103):111–118. PMID: 28339364.26. Nakazawa D, Tomaru U, Suzuki A, Masuda S, Hasegawa R, Kobayashi T, et al. Abnormal conformation and impaired degradation of propylthiouracil-induced neutrophil extracellular traps: implications of disordered neutrophil extracellular traps in a rat model of myeloperoxidase antineutrophil cytoplasmic antibodyassociated vasculitis. Arthritis Rheum. 2012; 64:3779–3787. PMID: 22777766.27. Schreiber A, Kettritz R. The neutrophil in antineutrophil cytoplasmic autoantibody-associated vasculitis. J Leukoc Biol. 2013; 94:623–631. PMID: 23381471.
Article28. Kettritz R. How anti-neutrophil cytoplasmic autoantibodies activate neutrophils. Clin Exp Immunol. 2012; 169:220–228. PMID: 22861361.
Article29. Ooi JD, Chang J, Hickey MJ, Borza DB, Fugger L, Holdsworth SR, et al. The immunodominant myeloperoxidase T-cell epitope induces local cell-mediated injury in antimyeloperoxidase glomerulonephritis. Proc Natl Acad Sci U S A. 2012; 109:E2615–E2624. PMID: 22955884.
Article30. Furuta S, Jayne DR. Antineutrophil cytoplasm antibody-associated vasculitis: recent developments. Kidney Int. 2013; 84:244–249. PMID: 23423257.
Article31. Xiao H, Dairaghi DJ, Powers JP, Ertl LS, Baumgart T, Wang Y, et al. C5a receptor (CD88) blockade protects against MPO-ANCA GN. J Am Soc Nephrol. 2014; 25:225–231. PMID: 24179165.
Article32. Charles Jennette J, Xiao H, Hu P. Complement in ANCA-associated vasculitis. Semin Nephrol. 2013; 33:557–564. PMID: 24161040.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of ANCA-Associated Vasculitis after Propylthiouracil Re-treatment
- Methimazole-Induced Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis in the Peripheral Nerves
- ANCA Associated Vasculitis
- ANCA-Associated Vasculitic Neuropathy with Concurrent Pulmonary Tuberculosis
- Mononeuritis Multiplex in Association with Anti-neutrophil Cytoplasmic Autoantibody(?) Vasculitis: A case report