Imaging Sci Dent.
2018 Mar;48(1):73-77. 10.5624/isd.2018.48.1.73.
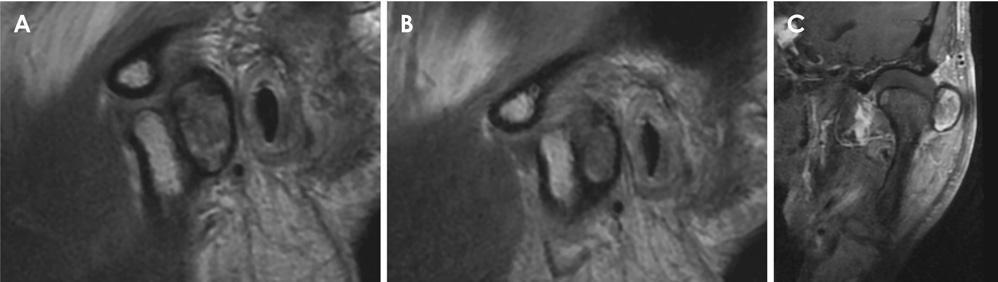
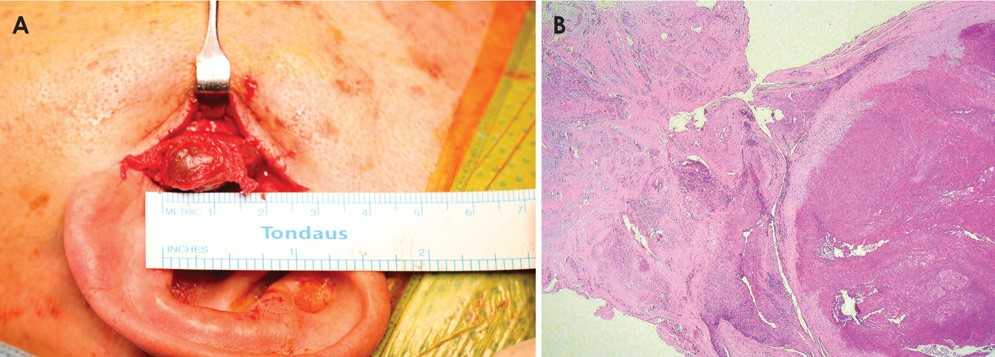
Organized hematoma of temporomandibular joint
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, Yonsei University College of Dentistry, Seoul, Korea. sshan@yuhs.ac
- 2Department of Oral Pathology, Oral Cancer Research Institute, Yonsei University, Seoul, Korea.
- KMID: 2406986
- DOI: http://doi.org/10.5624/isd.2018.48.1.73
Abstract
- Organized hematoma is a pseudo-tumorous lesion mostly occurs at sinonasal cavity and often confused with malignant neoplasm. The initiation of this lesion is blood accumulation, probably due to trauma, and this hematoma develops into organized hematoma as it encapsulated with fibrous band and neo-vascularized. Since it is uninformed at temporomandibular joint (TMJ) region, imaging diagnosis might be challenging. Also, delayed detection of mass involving TMJ is not uncommon due to confusion with joint disorder. Thus, this report introduced the rare pathology, organized hematoma on TMJ with advanced imaging features. Also, diagnostic point for early detection was described for the TMJ tumors and pseudo-tumors considering complexity of surgical intervention in this region.
MeSH Terms
Figure
Reference
-
1. Hur J, Kim JK, Byun JS, Lee WJ. Imaging characteristics of sinonasal organized hematoma. Acta Radiol. 2015; 56:955–959.
Article2. Ohta N, Watanabe T, Ito T, Kubota T, Suzuki Y, Ishida A, et al. Clinical and pathological characteristics of organized hematoma. Int J Otolaryngol. 2013; 2013:539642.
Article3. Yanagi Y, Asaumi J, Maki Y, Murakami J, Hisatomi M, Matsuzaki H, et al. Incidentally found and unexpected tumors discovered by MRI examination for temporomandibular joint arthrosis. Eur J Radiol. 2003; 47:6–9.
Article4. Poveda-Roda R, Bagán JV, Sanchis JM, Margaix M. Pseudotumors and tumors of the temporomandibular joint. A review. Med Oral Patol Oral Cir Bucal. 2013; 18:e392–e402.
Article5. Som PM, Curtin HD. Head and neck imaging. 5th ed. St. Louis: Mosby;2011.6. Negoro K, Uchida K, Yayama T, Kokubo Y, Baba H. Chronic expanding hematoma of the thigh. Joint Bone Spine. 2012; 79:192–194.
Article7. Wollina U, Heinig B, Langner D. Chronic expanding organized hematoma of the lower leg: a rare cause for nonhealing leg ulcers. Int J Low Extrem Wounds. 2015; 14:295–298.8. Ivankiv T, Ogurtsov O, Pokhylevych G. Organized hematoma mimicking retroperitoneal cystic tumors. Int J Surg Case Rep. 2016; 19:147–149.
Article9. Orhan K, Nishiyama H, Mitsunobu K, Furukawa S, Delilbasi C. Chronic hematic cyst of the temporomandibular joint: MRI features and dynamic magnetic resonance imaging. Eur J Radiol Extra. 2004; 52:97–101.
Article10. Bergin DJ, McCord CD, Dutton JJ, Garrett SN. Chronic hematic cyst of the orbit. Ophthal Plast Reconstr Surg. 1988; 4:31–36.
Article11. Zhou Q, Yang C, Chen MJ, Qiu YT, Qiu WL, Zheng JW. Primary intra- and juxta-articular vascular malformations of the temporomandibular joint: a clinical analysis of 8 consecutive patients. Int J Clin Exp Med. 2015; 8:2247–2253.12. Hu Y, Kuang B, Chen Y, Shu J. Imaging features for diffuse-type tenosynovial giant cell tumor of the temporomandibular joint: a case report. Medicine (Baltimore). 2017; 96:e7383.13. Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint. Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:101–107.14. Holmlund AB. Surgery for TMJ internal derangement. Evaluation of treatment outcome and criteria for success. Int J Oral Maxillofac Surg. 1993; 22:75–77.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organized Hematoma Presenting with Periorbital Swelling: A Case Report and Review of Literatures
- A study on simultation of the mandibular movement of the patients with temporomandibular joint disorder
- Autogenous auricular cartilage graft for repair of temporomandibular joint disk
- A Case of Organized Hematoma after Coblation Assisted Turbinoplasty
- Unrecognized Bilateral Dislocation of Temporomandibular Joint during Orotracheal Intubation