J Neurocrit Care.
2017 Dec;10(2):116-121. 10.18700/jnc.170013.
Spontaneous Subclavian Artery Dissection Presenting as Posterior Circulation Infarction
- Affiliations
-
- 1Department of Neurology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Neurology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea. fairlife1071@gmail.com
- KMID: 2405767
- DOI: http://doi.org/10.18700/jnc.170013
Abstract
- BACKGROUND
Spontaneous subclavian artery dissection (SAD) is rare. Moreover, there are very few case reports which document spontaneous SAD accompanied by symptomatic neurological deficits related with ischemic stroke.
CASE REPORT
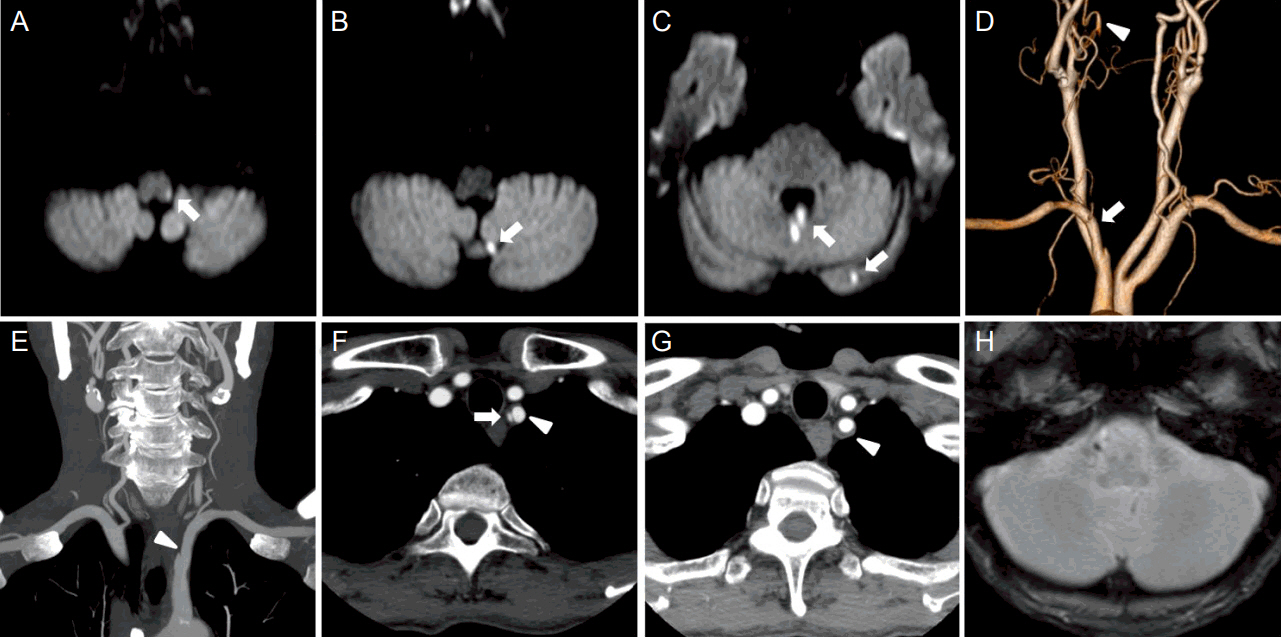
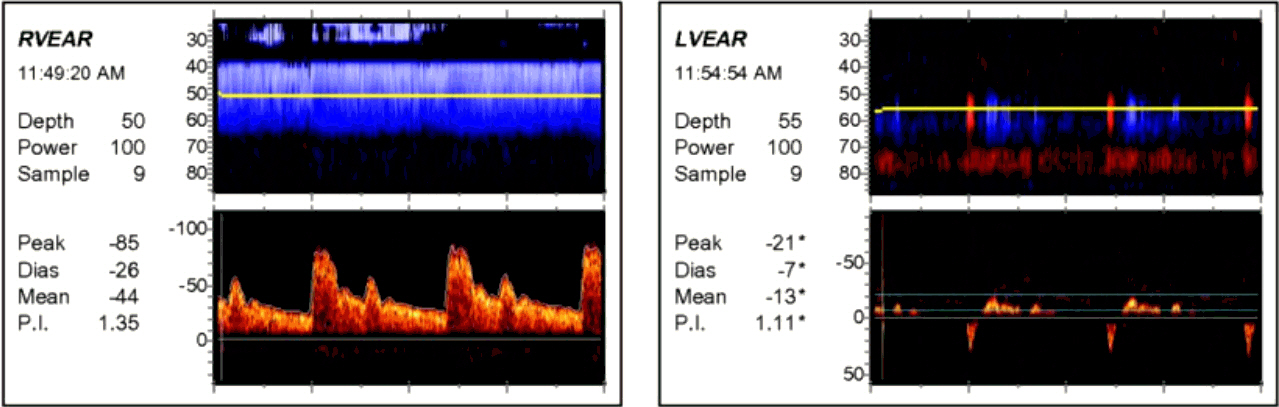
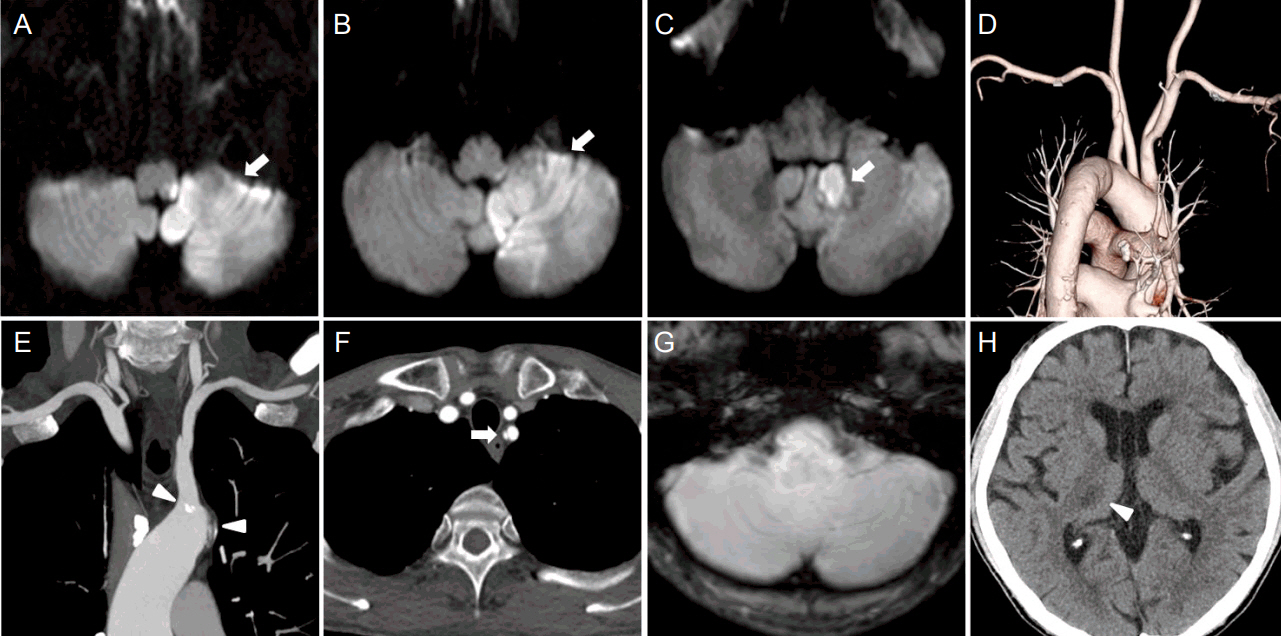
A 71-year-old man without any reported history of trauma presented with left facial hypesthesia, left arm ataxia and gait disturbance, subsequently diagnosed as posterior circulation infarction affecting medulla and cerebellum. The computed tomography angiography revealed spontaneous left SAD with left vertebral artery occlusion, atherosclerotic plaque surrounding the origin of left subclavian artery and normal aortic vasculature. His neurological status did not deteriorate further after dual anti-platelet therapy, and intravenous hydration with volume expander were applied.
CONCLUSIONS
This is an unusual case of spontaneous SAD with lateral medullary infarction as well as cerebellar infarction. Although spontaneous SAD is a distinctly rare disease entity, it should be considered in the differential diagnosis when multiple posterior circulation infarctions are observed.
Keyword
MeSH Terms
Figure
Reference
-
1. Marik PE, McLaughlin MT. Spontaneous subclavian artery dissection: a pain in the neck diagnosis. BMJ Case Rep. 2013; 2013:bcr2013201223.
Article2. Ananthakrishnan G, Bhat R, Zealley I. Spontaneous subclavian artery dissection causing ischemia of the arm: diagnosis and endovascular management. Cardiovasc Intervent Radiol. 2009; 32:326–8.
Article3. Henderson RA, Ward C, Campbell C. Dissecting left subclavian artery aneurysm: an unusual presentation of coarctation of the aorta. Int J Cardiol. 1993; 40:69–70.
Article4. Stanley GA, Arko FR 3rd, Foteh MI, Jessen ME, DiMaio JM. Hybrid endovascular treatment of an anomalous right subclavian artery dissection in a patient with Marfan syndrome. Ann Thorac Surg. 2012; 94:639–41.
Article5. Spies C, Fergusson D. Treatment of an iatrogenic subclavian artery dissection. Catheter Cardiovasc Interv. 2010; 76:35–8.
Article6. Günday M, Ozülkü M, Yıldırım E, Güven A, Ciftçi O. Successful endovascular treatment of subclavian artery dissection after compression trauma. Am J Emerg Med. 2013; 31:457.e1–3.
Article7. Garewal M, Selhorst JB. Subclavian artery dissection and triple infarction of the nervous system. Arch Neurol. 2005; 62:1917–9.
Article8. Iwamuro Y, Nakahara I, Tanaka M, Higashi T, Watanabe Y, Harada K, et al. Occlusion of the vertebral artery secondary to dissection of the subclavian artery--case report. Neurol Med Chir (Tokyo). 2005; 45:97–9.
Article9. Fernandes AF, Lange MC, Piovesan EJ, Zamproni LN, Germiniani FM, Zétola VF. Spontaneous subclavian artery dissection in a young woman with migraine: an unusual etiology of stroke. Arq Neuropsiquiatr. 2010; 68:475–6.
Article10. Schmitter SP, Marx M, Bernstein R, Wack J, Semba CP, Dake MD. Angioplasty-induced subclavian artery dissection in a patient with internal mammary artery graft: treatment with endovascular stent and stent-graft. AJR Am J Roentgenol. 1995; 165:449–51.
Article11. Reivich M, Holling HE, Roberts B, Toole JF. Reversal of blood flow through the vertebral artery and its effect on cerebral circulation. N Engl J Med. 1961; 265:878–85.
Article12. Park MG, Choi JH, Yang TI, Oh SJ, Baik SK, Park KP. Spontaneous isolated posterior inferior cerebellar artery dissection: rare but underdiagnosed cause of ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:1865–70.
Article13. Pessin MS, Daneault N, Kwan ES, Eisengart MA, Caplan LR. Local embolism from vertebral artery occlusion. Stroke. 1988; 19:112–5.
Article14. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160–236.15. Wada T, Takayama K, Taoka T, Nakagawa H, Myouchin K, Miyasaka T, et al. Long-term treatment outcomes after intravascular ultrasound evaluation and stent placement for atherosclerotic subclavian artery obstructive lesions. Neuroradiol J. 2014; 27:213–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multivessel spontaneous coronary artery dissection presenting as acute myocardial infarction
- Acute Myocardial Infarction in Patient with Spontaneous Coronary
- Spontaneous Renal Artery Dissection in a Patient with Protein C and S Deficiency
- Total Arch Replacement for Chronic Aortic Aneurysmal Dissection Patient with Aberrant Subclavian Artery
- Complication of Transradial Coronary Catheterization in Aberrant Insertion of the Right Subclavian Artery