J Korean Acad Nurs.
2018 Feb;48(1):26-37. 10.4040/jkan.2018.48.1.26.
Effects of Active Mandibular Exercise for Mouth Opening Limitation Patients after Maxillomandibular Fixation Release: A Non-Randomized Controlled Trial
- Affiliations
-
- 1Department of Nursing, Pusan National University, Yangsan, Korea. myung@pusan.ac.kr
- 2(Bio)Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2405467
- DOI: http://doi.org/10.4040/jkan.2018.48.1.26
Abstract
- PURPOSE
The aim of this study was to evaluate the effects of active mandibular exercise (AME) in patients with limited mouth opening after maxillomandibular fixation (MMF) release.
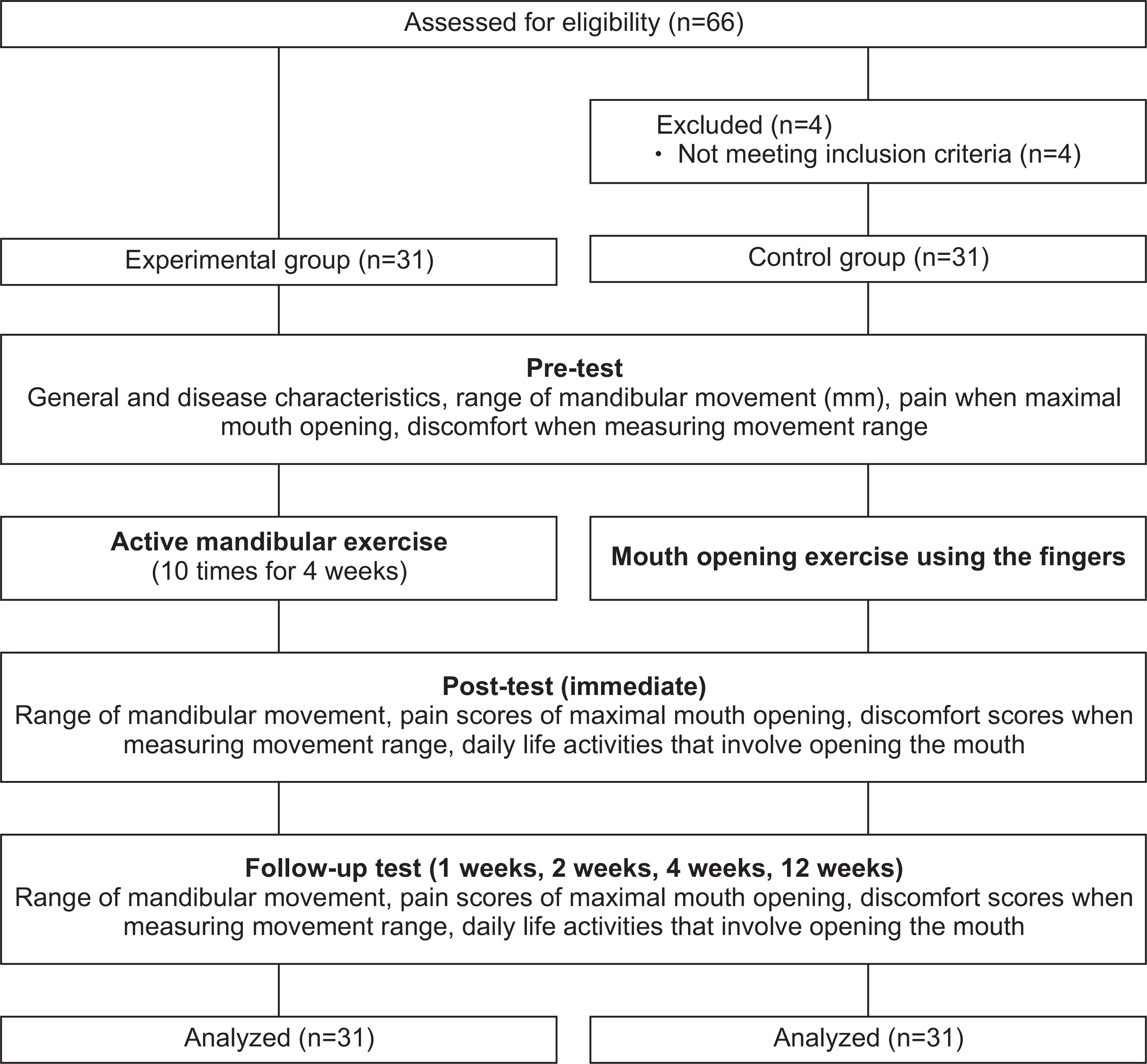
METHODS
The study used a quasi-experimental, nonequivalent control group and a pre test-post test design. Sixty-two patients with Maxillomandibular Fixation Release were assigned to the experimental (n=31) or control group (n=31). The AME was performed in the experimental group for 4 weeks. The exercise AME consisted of maximal mouth opening, lateral excursion and protrusive movement. These movements were repeated ten times a day. After the final exercise of the day, the number of tongue blades used for mouth opening was noted. The effect of AME was evaluated after MMF release at different time intervals: a) immediately, b) after 1 week, c) after 2 weeks, d) after 4 weeks, and e) after 12 weeks. The exercise was assessed using the following criteria: a) mandibular movements, b) pain scores associated with maximal mouth opening, c) discomfort scores associated with range of movement, and d) daily life activities that involve opening the mouth.
RESULTS
The experimental group showed significant improvement regarding the range of mandibular movements (maximal mouth opening (F=23.60, p < .001), lateral excursion to the right side (F=5.25, p=.002), lateral excursion to the left side (F=5.97, p=.001), protrusive movement (F=5.51, p=.001)), pain score (F=39.59, p < .001), discomfort score (F=9.38, p < .001). Daily life activities that involve opening the mouth were more favorable compared to those in the control group.
CONCLUSION
The AME in patients after MMF release is helpful for increasing mandibular movement range, decreasing pain and discomfort, and improving day life activities that involve opening the mouth. Therefore, AME is highly recommended as an effective nursing intervention.
Keyword
MeSH Terms
Figure
Reference
-
References
1. King RE, Scianna JM, Petruzzelli GJ. Mandible fracture pat- terns: A suburban trauma center experience. American Journal of Otolaryngology. 2004; 25(5):301–307. https://doi.org/10.1016/j.amjoto.2004.03.001.2. Yoon SY, Song JM, Kim YD, Chung IK, Shin SH. Pusan Korea Pusan National University. Clinical changes of TMD and condyle stability after two jaw surgery with and without preceding TMD treatments in class III patients. Maxillofacial Plastic and Reconstructive Surgery. 2015; 37(1):9. https://doi.org/10.1186/s40902-015-0008-2.
Article3. Lee CH, Kim CH. Open reduction of mandibular fracture without maxillomandibular fixation: Retrospective study. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2011; 37(4):255–263. https://doi.org/10.5125/jkaoms.2011.37.4.255.
Article4. Moon CW, Kim SG, Oh JS. Correlation between mandibular condylar process fracture and temporomandibular joint. Maxillofacial Plastic Reconstructive Surgery. 2010; 32(5):488–492.5. Jones JK, Van Sickels JE. A preliminary report of arthroscopic findings following acute condylar trauma. Journal of Oral and Maxillofacial Surgery. 1991; 49(1):55–60. https://doi.org/10.1016/0278-2391(91)90266-O.
Article6. Palmieri C, Ellis E 3rd, Throckmorton G. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. Journal of Oral and Maxillofacial Surgery. 1999; 57(7):764–775. discussion 775-776.https://doi.org/10.1016/S0278-2391(99)90810-8.
Article7. Blanchet PJ, Rompré PH, Lavigne GJ, Lamarche C. Oral dyskinesia: A clinical overview. International Journal of Prosthodontics. 2005; 18(1):10–19.8. Korean Association of Oral and Maxillofacial Surgery. Textbook of oral and maxillofacial surgery. 3rd ed. Seoul: Medical & Dental Publishing Co.;2013. p. 241–254. 447, 505.9. Lee JK, Kim KW, Lee JH. An experimental study of effect of intermaxillary fixation and occusal splint on pulmonary function. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2002; 28(3):175–181.10. Kim SN, Lee DG, Bae JO, Woo SC. Effect of Therabite jaw motion rehabilitation systemTM for treatment of limited mouth opening. Journal of Wonkwang Biomaterial Implant. 1996; 4(3):1–19.11. Jung W, Lee KE, Sun SA, Suh BJ. Opening exercise therapy with locking-free appliance (LA): Preliminary study. Journal of Oral Medicine and Pain. 2013; 38(1):29–34.12. Ohba S, Tasaki H, Tobita T, Minamizato T, Kawasaki T, Motooka N, et al. Assessment of skeletal stability of intraoral vertical ramus osteotomy with one-day maxillary-mandibular fixation followed by early jaw exercise. Journal of Cranio-Maxillofacial Surgery. 2013; 41(7):586–592. https://doi.org/10.1016/j.jcms.2012.11.032.
Article13. Jang SY, Kim SH, Choi JK. A case report on abnormal jaw movements associated with brain injury. Journal of Oral Medicine and Pain. 1998; 23(4):447–454.14. Kim HJ, Kim BJ. Effects of temporal muscle exercise on mastication after craniotomy. Korean Journal of Adult Nursing. 2012; 24(2):130–138. https://doi.org/10.7475/kjan.2012.24.2.138.
Article15. Teng TT, Ko EW, Huang CS, Chen YR. The effect of early physiotherapy on the recovery of mandibular function after orthognathic surgery for Class III correction: Part I–jaw-motion analysis. Journal of Cranio-Maxillofacial Surgery. 2015; 43(1):131–137. https://doi.org/10.1016/j.jcms.2014.10.025.
Article16. Han TR, Bang MS, Jung SG, Kang YK, Ko MH, Ko YJ, et al. Rehabilitation medicine. 5th ed. Seoul: Koonja Publishing;2014. p. 252–254.17. Conn VS, Hafdahl AR, Mehr DR. Interventions to increase physical activity among healthy adults: Meta-analysis of outcomes. American Journal of Public Health. 2011; 101(4):751–758. https://doi.org/10.2105/AJPH.2010.194381.
Article18. Cunningham SJ, Gilthorpe MS, Hunt NP. Are orthognathic patients different? European Journal of Orthodontics. 2000; 22(2):195–202. https://doi.org/10.1093/ejo/22.2.195.
Article19. Bock JJ, Odemar F, Fuhrmann RA. Assessment of quality of life in patients undergoing orthognathic surgery. Journal of Orofacial Orthopedics. 2009; 70(5):407–419. https://doi.org/10.1007/s00056-009-9903-4.
Article20. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates;1988. p. 1–400.21. McLachlan E. Pain and suffering. Recognizing pain. The American Journal of Nursing. 1974; 74(3):496–497.22. Seo HJ. The effects of relaxation technique on anxiety and distress of patients with gastrofibroscopy [master’s thesis]. Seoul: Ewha Womans University;1990. p. 1–73.23. Lee SK, Choi YK, Hwang DY, Kim KW. The occlusal force and EMG change after BSSRO. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2008; 34(5):537–542.24. Ju YY, Liu YC, Cheng HY, Chang YJ. Rapid repetitive passive movement improves knee proprioception. Clinical Biomechanics (Bristol, Avon). 2011; 26(2):188–193. https://doi.org/10.1016/j.clinbiomech.2010.09.015.
Article25. Shin JH, Kim GS, Lee JH, Oh SJ. The effects of periodic reminding interventions on medication adherence, self-efficacy, and pain for home-based lung cancer patients. Journal of Korean Clinical Nursing Research. 2013; 19(3):443–454.26. Lee BN, Lee GE. Effects of pain control education on pain control barrier, postoperative pain and pain control satisfaction in gynecological patients. Journal of Korean Academy of Nursing. 2006; 36(6):968–975. https://doi.org/10.4040/jkan.2006.36.6.968.
Article27. Maloney GE, Mehta N, Forgione AG, Zawawi KH, Al-Badawi EA, Driscoll SE. Effect of a passive jaw motion device on pain and range of motion in TMD patients not responding to flat plane intraoral appliances. Journal of Craniomandibular & Sleep Practice. 2002; 20(1):55–66. https://doi.org/10.1080/08869634.2002.11746191.
Article28. Kim IS, Kim HS, Lee MH. Effects of music therapy on anxiety and distress in patients taking thoracentesis. Journal of East-West Nursing Research. 2011; 17(2):103–109.29. Wang J, Chen W, Ni Z, Zheng M, Liang X, Zheng Y, et al. Tim- ing of orthognathic surgery on the changes of oral health-related quality of life in Chinese orthognathic surgery. American Journal of Orthodontics and Dentofacial Orthopedics. 2017; 151(3):565–571. https://doi.org/10.1016/j.ajodo.2016.06.050.30. Hwang JH, Kim SY. The influence of unloading taping method using non-elastic tape on the pain, opening mouth, functional level, quality of life in patients with temporomandibular joint disorder. Physical Therapy Korea. 2016; 23(3):29–39. https://doi.org/10.12674/ptk.2016.23.3.029.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Use Of Bone Reduction Forceps For Reduction And Fixation Of Mandibular Angle Fractures
- The effect of early removal of the fixation plates and active mouth opening exercise on the temporomandibular dysfunction after mandibular setback surgery
- Microplate Fixation without Maxillomandibular Fixation in Double Mandibular Fractures
- Mandibular Ramus Osteochondroma-A Rare Cause of Chronic Mouth Opening Limitation: A Case Report
- Difficult Endotracheal Intubation Due to Unrecognized Dysfunction of Temporomandibular Joint: A case report