J Korean Orthop Assoc.
2018 Feb;53(1):19-28. 10.4055/jkoa.2018.53.1.19.
Etiology and Management of Nonunion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyungpook National University School of Medicine, Daegu, Korea. cwoh@knu.ac.kr
- KMID: 2405395
- DOI: http://doi.org/10.4055/jkoa.2018.53.1.19
Abstract
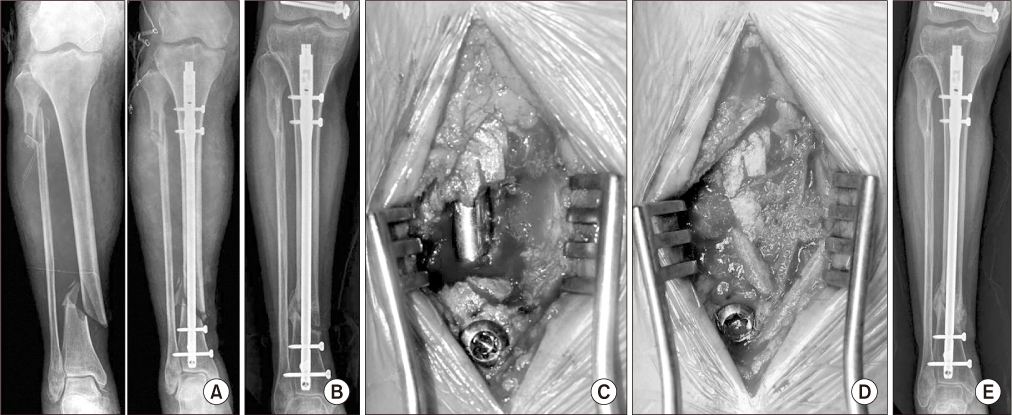
- Nonunion is caused by various factors related to fracture characteristics, patient characteristics, treatment, and infection. Aseptic nonunion, is divided into three categories in accordance with the biological activity of the fracture: atrophic nonunion, oligotrophic nonunion, and hypertrophic nonunion. Treatment of nonunion depends on the cause and classification. Here, we report our experiences and review the various causes of nonunion and treatment methods available.
Keyword
MeSH Terms
Figure
Reference
-
1. McKee MD, DiPasquale DJ, Wild LM, Stephen DJ, Kreder HJ, Schemitsch EH. The effect of smoking on clinical outcome and complication rates following Ilizarov reconstruction. J Orthop Trauma. 2003; 17:663–667.
Article2. Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM. LEAP Study Group. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005; 19:151–157.
Article3. Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br. 2000; 82:655–658.4. Hak DJ. Management of aseptic tibial nonunion. J Am Acad Orthop Surg. 2011; 19:563–573.
Article5. Park J, Kim SG, Yoon HK, Yang KH. The treatment of nonisthmal femoral shaft nonunions with im nail exchange versus augmentation plating. J Orthop Trauma. 2010; 24:89–94.
Article6. Brinker MR, O'Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007; 89:177–188.
Article7. Oh JK, Bae JH, Oh CW, Biswal S, Hur CR. Treatment of femoral and tibial diaphyseal nonunions using reamed intramedullary nailing without bone graft. Injury. 2008; 39:952–959.
Article8. Yang KH, Kim JR, Park J. Nonisthmal femoral shaft nonunion as a risk factor for exchange nailing failure. J Trauma Acute Care Surg. 2012; 72:E60–E64.
Article9. Eom TW, Kim JJ, Oh HK, Kim JW. Challenge to treat hypertrophic nonunion of the femoral shaft: the Poller screw augmentation technique. Eur J Orthop Surg Traumatol. 2016; 26:559–563.
Article10. Litrenta J, Tornetta P 3rd, Vallier H, et al. Dynamizations and exchanges: success rates and indications. J Orthop Trauma. 2015; 29:569–573.11. Oh CW, Apivatthakakul T, Oh JK, et al. Bone transport with an external fixator and a locking plate for segmental tibial defects. Bone Joint J. 2013; 95:1667–1672.
Article12. Oh CW, Song HR, Roh JY, et al. Bone transport over an intramedullary nail for reconstruction of long bone defects in tibia. Arch Orthop Trauma Surg. 2008; 128:801–808.
Article13. Ziran BH, Smith WR, Morgan SJ. Use of calcium-based demineralized bone matrix/allograft for nonunions and posttraumatic reconstruction of the appendicular skeleton: preliminary results and complications. J Trauma. 2007; 63:1324–1328.
Article14. Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000; 45:346–353.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associated Factors of Nonunion Following Conservative Management of Distal Clavicle Fractures
- Relationship of Tibial Nonunion with Fibular Nonunion in the Tibio-fibular Shaft Fracture
- Surgical Treatment of Malunion and Nonunion after Pelvic Bone Fracture
- The Use of Poller Screws in Nonunion of Femoral Shaft Following Intramedullary Nailing of Femoral Shaft Fracture: A Case Report
- A Clinical Study on Nonunion of the Forearm Fracture