Korean J Radiol.
2018 Apr;19(2):311-319. 10.3348/kjr.2018.19.2.311.
Clinical Feasibility of Synthetic Magnetic Resonance Imaging in the Diagnosis of Internal Derangements of the Knee
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, YUHS-KRIBB Medical Convergence Research Institute, and Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul 03722, Korea. radiologie@gmail.com
- KMID: 2404928
- DOI: http://doi.org/10.3348/kjr.2018.19.2.311
Abstract
OBJECTIVE
To evaluate the feasibility of synthetic magnetic resonance imaging (MRI) compared to conventional MRI for the diagnosis of internal derangements of the knee at 3T.
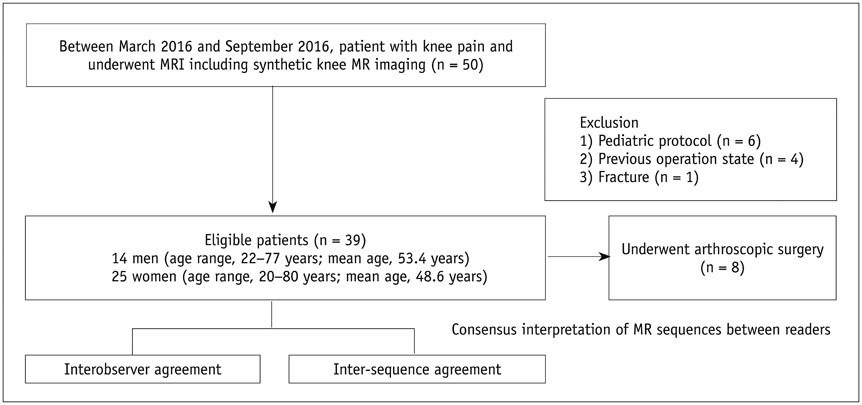
MATERIALS AND METHODS
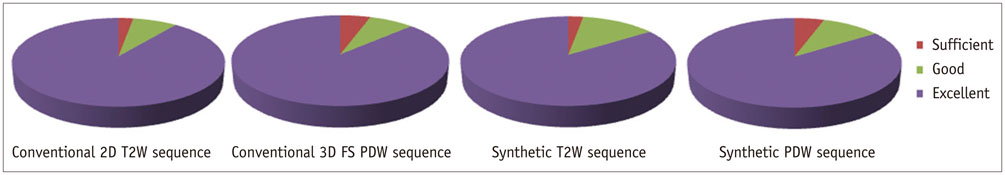
Following Institutional Review Board approval, image sets of conventional and synthetic MRI in 39 patients were included. Two musculoskeletal radiologists compared the image sets and qualitatively analyzed the images. Subjective image quality was assessed using a four-grade scale. Interobserver agreement and intersequence agreement between conventional and synthetic images for cartilage lesions, tears of the cruciate ligament, and tears of the meniscus were independently assessed using Kappa statistics. In patients who underwent arthroscopy (n = 8), the sensitivity, specificity, and accuracy for evaluated internal structures were calculated using arthroscopic findings as the gold standard.
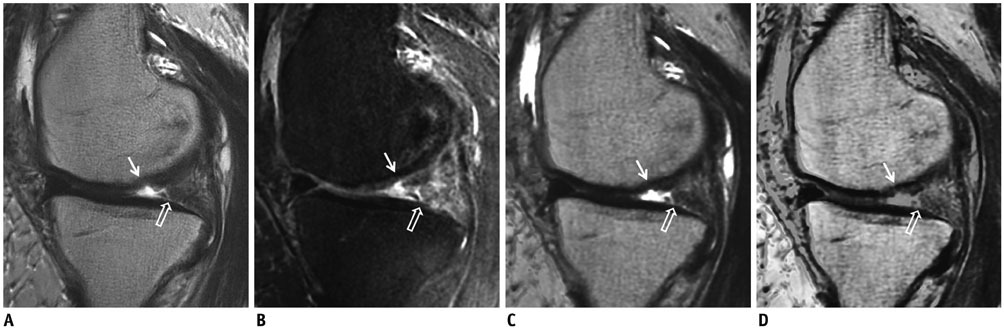
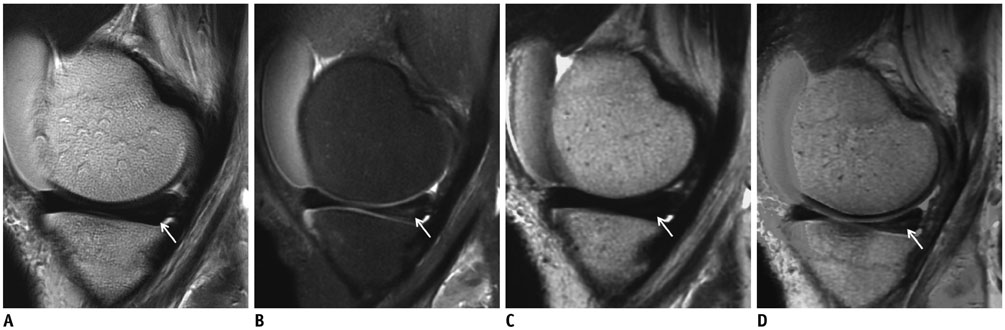
RESULTS
There was no statistically significant difference in image quality (p = 0.90). Interobserver agreement (κ = 0.649- 0.981) and intersequence agreement (κ = 0.794-0.938) were nearly perfect for all evaluated structures. The sensitivity, specificity, and accuracy for detecting cartilage lesions (sensitivity, 63.6% vs. 54.6-63.6%; specificity, 91.9% vs. 91.9%; accuracy, 83.3-85.4% vs. 83.3-85.4%) and tears of the cruciate ligament (sensitivity, specificity, accuracy, 100% vs. 100%) and meniscus (sensitivity, 50.0-62.5% vs. 62.5%; specificity, 100% vs. 87.5-100%; accuracy, 83.3-85.4% vs. 83.3-85.4%) were similar between the two MRI methods.
CONCLUSION
Conventional and synthetic MRI showed substantial to almost perfect degree of agreement for the assessment of internal derangement of knee joints. Synthetic MRI may be feasible in the diagnosis of internal derangements of the knee.
Keyword
MeSH Terms
Figure
Reference
-
1. Fritz RC. MR imaging of meniscal and cruciate ligament injuries. Magn Reson Imaging Clin N Am. 2003; 11:283–293.
Article2. Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F, et al. Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radiographics. 2011; 31:37–61.
Article3. Stoller DW. Magnetic resonance imaging in orthopaedics and sports medicine, Volume 1. 3rd ed. Ambler, PA: Lippincott Williams & Wilkins;2007. p. 307.4. Duc SR, Zanetti M, Kramer J, Käch KP, Zollikofer CL, Wentz KU. Magnetic resonance imaging of anterior cruciate ligament tears: evaluation of standard orthogonal and tailored paracoronal images. Acta Radiol. 2005; 46:729–733.
Article5. Roberts CC, Towers JD, Spangehl MJ, Carrino JA, Morrison WB. Advanced MR imaging of the cruciate ligaments. Radiol Clin North Am. 2007; 45:1003–1016. vi-vii.
Article6. Kim HS, Yoon YC, Park KJ, Wang JH, Choe BK. Interposition of the posterior cruciate ligament into the medial compartment of the knee joint on coronal magnetic resonance imaging. Korean J Radiol. 2016; 17:239–244.
Article7. Fitzgerald SW, Remer EM, Friedman H, Rogers LF, Hendrix RW, Schafer MF. MR evaluation of the anterior cruciate ligament: value of supplementing sagittal images with coronal and axial images. AJR Am J Roentgenol. 1993; 160:1233–1237.
Article8. Peterfy CG, Gold G, Eckstein F, Cicuttini F, Dardzinski B, Stevens R. MRI protocols for whole-organ assessment of the knee in osteoarthritis. Osteoarthritis Cartilage. 2006; 14:Suppl A. A95–A111.
Article9. Betts AM, Leach JL, Jones BV, Zhang B, Serai S. Brain imaging with synthetic MR in children: clinical quality assessment. Neuroradiology. 2016; 58:1017–1026.
Article10. Blystad I, Warntjes JB, Smedby O, Landtblom AM, Lundberg P, Larsson EM. Synthetic MRI of the brain in a clinical setting. Acta Radiol. 2012; 53:1158–1163.
Article11. Hasan KM, Walimuni IS, Abid H, Wolinsky JS, Narayana PA. Multi-modal quantitative MRI investigation of brain tissue neurodegeneration in multiple sclerosis. J Magn Reson Imaging. 2012; 35:1300–1311.
Article12. West J, Warntjes JB, Lundberg P. Novel whole brain segmentation and volume estimation using quantitative MRI. Eur Radiol. 2012; 22:998–1007.
Article13. Bonnier G, Roche A, Romascano D, Simioni S, Meskaldji D, Rotzinger D, et al. Advanced MRI unravels the nature of tissue alterations in early multiple sclerosis. Ann Clin Transl Neurol. 2014; 1:423–432.
Article14. Granberg T, Uppman M, Hashim F, Cananau C, Nordin LE, Shams S, et al. Clinical feasibility of synthetic MRI in multiple sclerosis: a diagnostic and volumetric validation study. AJNR Am J Neuroradiol. 2016; 37:1023–1029.
Article15. Masi JN, Sell CA, Phan C, Han E, Newitt D, Steinbach L, et al. Cartilage MR imaging at 3.0 versus that at 1.5 T: preliminary results in a porcine model. Radiology. 2005; 236:140–150.
Article16. Barnett MJ. MR diagnosis of internal derangements of the knee: effect of field strength on efficacy. AJR Am J Roentgenol. 1993; 161:115–118.
Article17. Mink JH, Levy T, Crues JV 3rd. Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988; 167:769–774.
Article18. Robertson PL, Schweitzer ME, Bartolozzi AR, Ugoni A. Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology. 1994; 193:829–834.
Article19. De Smet AA, Norris MA, Yandow DR, Quintana FA, Graf BK, Keene JS. MR diagnosis of meniscal tears of the knee: importance of high signal in the meniscus that extends to the surface. AJR Am J Roentgenol. 1993; 161:101–107.
Article20. Noyes FR, Stabler CL. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989; 17:505–513.
Article21. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article22. Barth M, Breuer F, Koopmans PJ, Norris DG, Poser BA. Simultaneous multislice (SMS) imaging techniques. Magn Reson Med. 2016; 75:63–81.
Article23. Zahneisen B, Ernst T, Poser BA. SENSE and simultaneous multislice imaging. Magn Reson Med. 2015; 74:1356–1362.
Article24. Zhang T, Chowdhury S, Lustig M, Barth RA, Alley MT, Grafendorfer T, et al. Clinical performance of contrast enhanced abdominal pediatric MRI with fast combined parallel imaging compressed sensing reconstruction. J Magn Reson Imaging. 2014; 40:13–25.
Article25. Warntjes JB, Dahlqvist O, Lundberg P. Novel method for rapid, simultaneous T1, T2*, and proton density quantification. Magn Reson Med. 2007; 57:528–537.26. Nozaki T, Kaneko Y, Yu HJ, Kaneshiro K, Schwarzkopf R, Yoshioka H. Comparison of T1rho imaging between spoiled gradient echo (SPGR) and balanced steady state free precession (b-FFE) sequence of knee cartilage at 3T MRI. Eur J Radiol. 2015; 84:1299–1305.
Article27. Kijowski R, Blankenbaker DG, Munoz Del, Baer GS, Graf BK. Evaluation of the articular cartilage of the knee joint: value of adding a T2 mapping sequence to a routine MR imaging protocol. Radiology. 2013; 267:503–513.
Article28. Yoon MA, Hong SJ, Im AL, Kang CH, Kim BH, Kim IS. Comparison of T1rho and T2 mapping of knee articular cartilage in an asymptomatic population. Korean J Radiol. 2016; 17:912–918.
Article29. Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003; 226:837–848.
Article30. Jung JY, Yoon YC, Kwon JW, Ahn JH, Choe BK. Diagnosis of internal derangement of the knee at 3.0-T MR imaging: 3D isotropic intermediate-weighted versus 2D sequences. Radiology. 2009; 253:780–787.
Article31. Jung JY, Yoon YC, Kim HR, Choe BK, Wang JH, Jung JY. Knee derangements: comparison of isotropic 3D fast spin-echo, isotropic 3D balanced fast field-echo, and conventional 2D fast spin-echo MR imaging. Radiology. 2013; 268:802–813.
Article32. Kijowski R, Davis KW, Woods MA, Lindstrom MJ, De Smet AA, Gold GE, et al. Knee joint: comprehensive assessment with 3D isotropic resolution fast spin-echo MR imaging--diagnostic performance compared with that of conventional MR imaging at 3.0 T. Radiology. 2009; 252:486–495.
Article33. Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging-based diagnosis and classification of meniscal tears. Radiographics. 2014; 34:981–999.
Article34. Pipe JG. Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med. 1999; 42:963–969.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of diagnoses from magnetic resonance imaging of the knee
- Magnetic resonance imaging in the knee joint
- The clinical value of magnetic resonance imaging in the evaluation of internal derangement of the knee
- Clinical value of magnetic resonance imaging compared with arthroscopic findings in internal derangement of the knee
- A Case of Pedunculated Localized Nodular Synovitis of the Knee: MR Imaging Findings