Korean J Clin Neurophysiol.
2015 Dec;17(2):76-79. 10.14253/kjcn.2015.17.2.76.
Recurrent Myelopathy in a Patient with Klippel-Trenaunay Syndrome
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Suwon, Korea. isjoo@ajou.ac.kr
- KMID: 2403243
- DOI: http://doi.org/10.14253/kjcn.2015.17.2.76
Abstract
- Klippel-Trenaunay syndrome (KTS) is a rare congenital malformation syndrome involving blood and lymph vessels, which is characterized by triad of cutaneous hemangioma, venous varicosities, and overgrowth of the affected limbs. Because vascular malformation in KTS can be located anywhere except the face and brain, the clinical presentation could be extremely variable. But there are only rare case reports that KTS is associated with spinal cord lesion. We report a case of recurrent myelopathy in a patient with KTS.
MeSH Terms
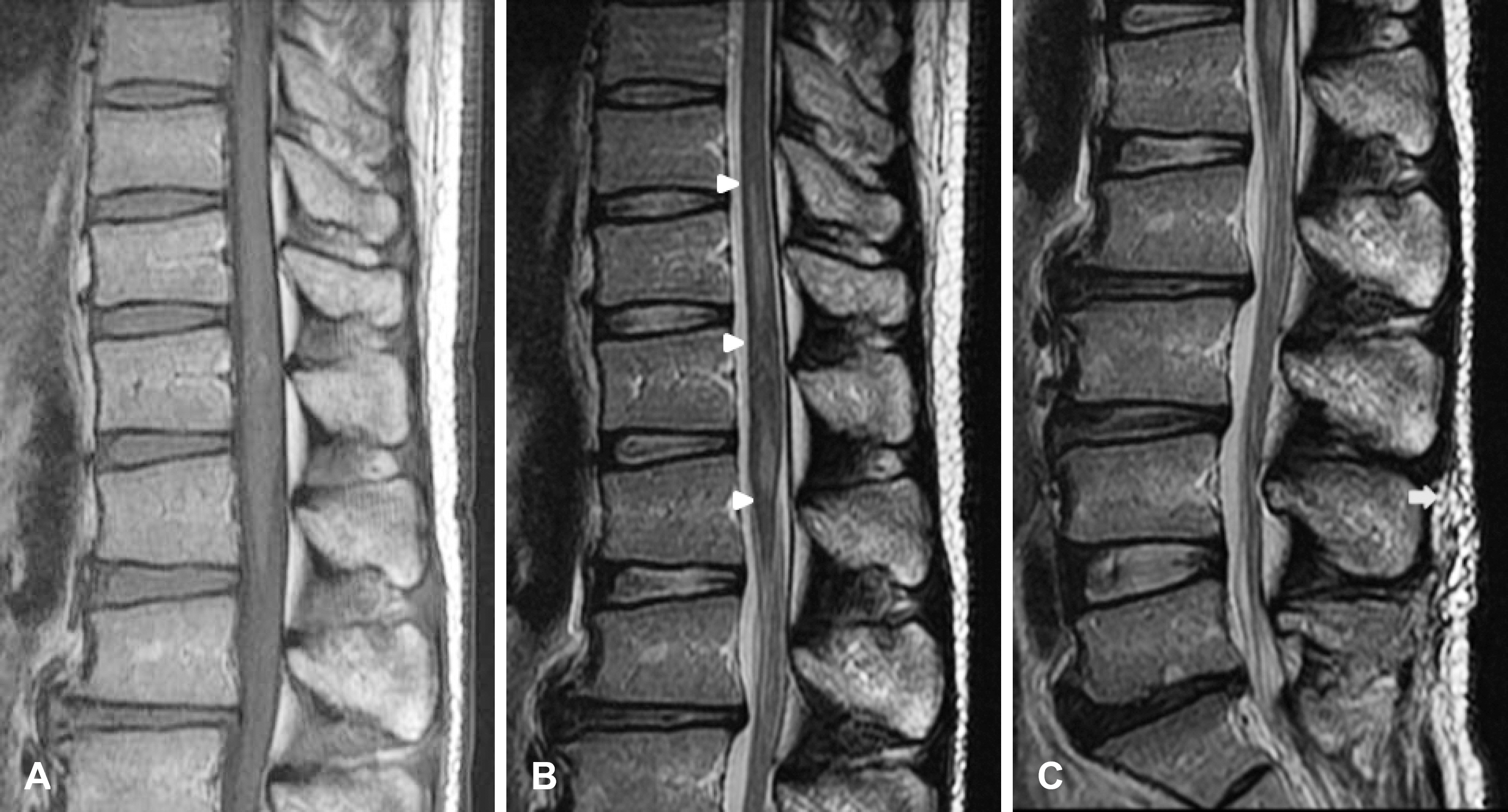
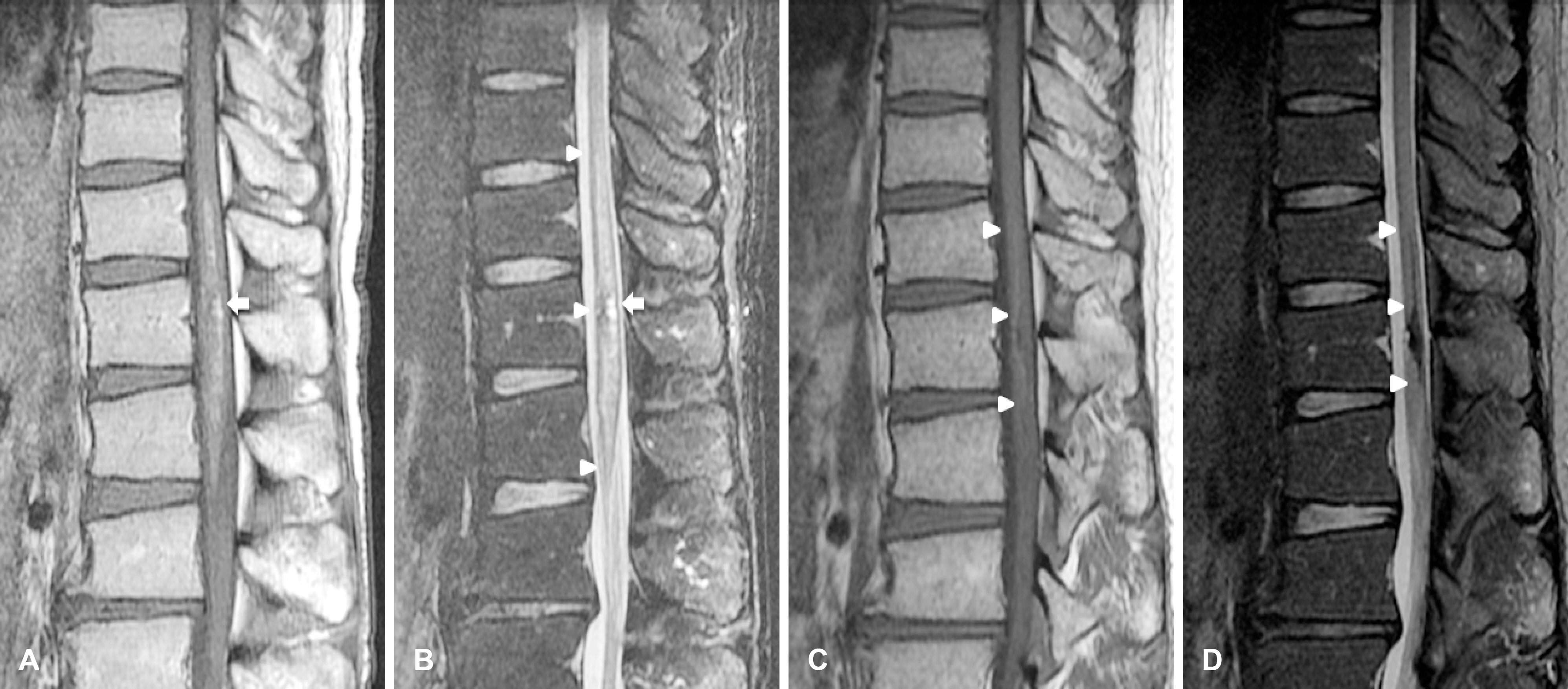
Figure
Reference
-
1.Jacob AG., Driscoll DJ., Shaughnessy WJ., Stanson AW., Clay RP., Gloviczki P. Klippel-Trenaunay syndrome: spectrum and management. Mayo Clin Proc. 1998. 73:28–36.
Article2.Jeun KH., Kim YP. A case report of the Klippel-Trenaunay syndrome. Korea J Dermatol. 1971. 9:15–22.3.Alomari AI., Orbach DB., Mulliken JB., Bisdorff A., Fishman SJ., Norbash A, et al. Klippel-Trenaunay syndrome and spinal arteriovenous malformations: an erroneous association. AJNR Am J Neuroradiol. 2010. 31:1608–1612.
Article4.Kojima Y., Kuwana N., Sato M., Ikeda Y. Klippel- Trenaunay-Weber syndrome with spinal arteriovenous malformation-case report. Neurol Med Chir. 1989. 29:235–240.5.Servelle M., Bastin R., Loygue J., Montagnani A., Bacour F., Soulie J, et al. Hematuria and rectal bleeding in the child with Klippel and Trenaunay syndrome. Ann Surg. 1976. 183:418–428.
Article6.Parsa CF. Focal venous hypertension as a pathophysiologic mechanism for tissue hypertrophy, port-wine stains, the Sturge-Weber syndrome, and relateddisorders: proof of concept with novel hypothesis for underlying etiological cause (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2013. 111:180–215.7.Cohen MM Jr. Vasculogenesis, angiogenesis, hemangiomas, and vascular malformations. Am J Med Genet. 2002. 108:265–274.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Klippel-Trenaunay Syndrome, 2 Cases
- Klippel-trenaunay-weber syndrome
- A Case of Klippel-Trenaunay-Weber Syndrome Diagnosed by Antenatal Ultrasonography
- Bladder Hemangioma Associated with Klippel-Trenaunay Syndrome: Case Report
- A Case of Klippel-Trenaunay Syndrome with Microcystic Lymphatic Malformation on Anus