A prospective randomized study comparing radiofrequency ablation and hepatic resection for hepatocellular carcinoma
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. kssuh@snu.ac.kr
- 2Department of Surgery, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 5Liver Cancer Center, National Cancer Center, Goyang, Korea.
- KMID: 2402849
- DOI: http://doi.org/10.4174/astr.2018.94.2.74
Abstract
- PURPOSE
Although there are several prospective clinical studies comparing radiofrequency ablation (RFA) and hepatic resection (HR) for the treatment of hepatocellular carcinoma, there are few trials that have been performed in strictly homogeneous patients.
METHODS
Patients who were newly diagnosed with a solitary hepatocellular carcinoma were randomized to the HR or RFA group. Inclusion criteria were as follows: age ≥ 20 years but ≤ 70 years, Child-Pugh class A, maximal diameter of the tumor ≥ 2 cm but ≤ 4 cm, no previous treatment history, and platelet count > 80,000/mm3.
RESULTS
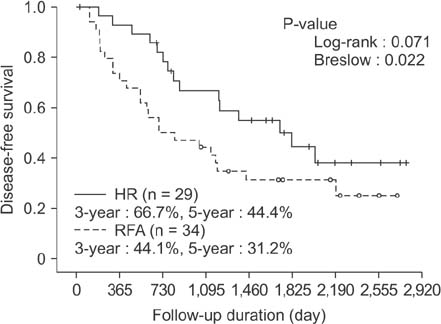
Although the study was early terminated, 29 and 34 patients were enrolled in the HR and RFA groups, respectively, and prospectively followed on an intention-to-treat basis. The 5-year overall survival rates were 83.4% and 86.2% in the HR and RFA groups, respectively, which were not significantly different (P = 0.812 by log-rank, P = 0.990 by Breslow). The 3- and 5-year disease-free survival rates in the HR group were significantly superior to those in the RFA group (66.7%, 44.4% vs. 44.1%, 31.2%, P = 0.071 by log-rank, P = 0.023 by Breslow). Intrahepatic local recurrence tended to develop more frequently in the RFA group (P = 0.042), while the frequency of intrahepatic distant and extrahepatic recurrence was similar bet ween the 2 groups. There were no significant differences in the frequency and severity of complications between the 2 groups.
CONCLUSION
HR was significantly superior to RFA in terms of disease-free survival; however, the overall survival was excellent in both groups.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
2018 Korean Liver Cancer Association–National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
,
Korean J Radiol. 2019;20(7):1042-1113. doi: 10.3348/kjr.2019.0140.2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
J Liver Cancer. 2023;23(1):1-120. doi: 10.17998/jlc.2022.11.07.Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study
Kazuya Kariyama, Kazuhiro Nouso, Atsushi Hiraoka, Hidenori Toyoda, Toshifumi Tada, Kunihiko Tsuji, Toru Ishikawa, Takeshi Hatanaka, Ei Itobayashi, Koichi Takaguchi, Akemi Tsutsui, Atsushi Naganuma, Satoshi Yasuda, Satoru Kakizaki, Akiko Wakuta, Shohei Shiota, Masatoshi Kudo, Takashi Kumada
J Liver Cancer. 2024;24(1):71-80. doi: 10.17998/jlc.2023.09.11.
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108.
Article2. Taylor-Robinson SD, Foster GR, Arora S, Hargreaves S, Thomas HC. Increase in primary liver cancer in the UK, 1979-94. Lancet. 1997; 350:1142–1143.
Article3. El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999; 340:745–750.
Article4. Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol. 2008; 48:Suppl 1. S20–S37.
Article5. Huang J, Yan L, Cheng Z, Wu H, Du L, Wang J, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg. 2010; 252:903–912.
Article6. Lai EC, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Hepatic resection for hepatocellular carcinoma. An audit of 343 patients. Ann Surg. 1995; 221:291–298.
Article7. Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg. 2006; 243:321–328.
Article8. Lau WY, Leung TW, Yu SC, Ho SK. Percutaneous local ablative therapy for hepatocellular carcinoma: a review and look into the future. Ann Surg. 2003; 237:171–179.9. Rossi S, Buscarini E, Garbagnati F, Di Stasi M, Quaretti P, Rago M, et al. Percutaneous treat ment of small hepatic tumors by an expandable RF needle electrode. AJR Am J Roentgenol. 1998; 170:1015–1022.10. Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000; 232:381–391.
Article11. Wood TF, Rose DM, Chung M, Allegra DP, Foshag LJ, Bilchik AJ. Radiofrequency ablation of 231 unresectable hepatic tumors: indications, limitations, and complications. Ann Surg Oncol. 2000; 7:593–600.
Article12. Buscarini L, Buscarini E, Di Stasi M, Vallisa D, Quaretti P, Rocca A. Percutaneous radiofrequency ablation of small hepatocellular carcinoma: long-term results. Eur Radiol. 2001; 11:914–921.
Article13. Clavien PA, Camargo CA Jr, Croxford R, Langer B, Levy GA, Greig PD. Definition and classification of negative outcomes in solid organ transplantation. Application in liver transplantation. Ann Surg. 1994; 220:109–120.
Article14. Montorsi M, Santambrogio R, Bianchi P, Donadon M, Moroni E, Spinelli A, et al. Survival and recurrences after hepatic resection or radiofrequency for hepatocellular carcinoma in cirrhotic patients: a multivariate analysis. J Gastrointest Surg. 2005; 9:62–67.
Article15. Vivarelli M, Guglielmi A, Ruzzenente A, Cucchetti A, Bellusci R, Cordiano C, et al. Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Ann Surg. 2004; 240:102–107.
Article16. Lau WY. Management of hepatocellular carcinoma. J R Coll Surg Edinb. 2002; 47:389–399.17. Hong SN, Lee SY, Choi MS, Lee JH, Koh KC, Paik SW, et al. Comparing the outcomes of radiofrequency ablation and surgery in patients with a single small hepatocellular carcinoma and well-preserved hepatic function. J Clin Gastroenterol. 2005; 39:247–252.
Article18. Ni JY, Xu LF, Sun HL, Zhou JX, Chen YT, Luo JH. Percutaneous ablation therapy versus surgical resection in the treatment for early-stage hepatocellular carcinoma: a meta-analysis of 21,494 patients. J Cancer Res Clin Oncol. 2013; 139:2021–2033.
Article19. Wang Y, Luo Q, Li Y, Deng S, Wei S, Li X. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinomas: a meta-analysis of randomized and nonrandomized controlled trials. PLoS One. 2014; 9:e84484.
Article20. Xu Q, Kobayashi S, Ye X, Meng X. Comparison of hepatic resection and radiofrequency ablation for small hepatocellular carcinoma: a meta-analysis of 16,103 patients. Sci Rep. 2014; 4:7252.
Article21. Hasegawa K, Kokudo N, Imamura H, Matsuyama Y, Aoki T, Minagawa M, et al. Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg. 2005; 242:252–259.
Article22. Regimbeau JM, Kianmanesh R, Farges O, Dondero F, Sauvanet A, Belghiti J. Extent of liver resection influences the outcome in patients with cirrhosis and small hepatocellular carcinoma. Surgery. 2002; 131:311–317.
Article23. Sasaki A, Kai S, Iwashita Y, Hirano S, Ohta M, Kitano S. Microsatellite distribution and indication for locoregional therapy in small hepatocellular carcinoma. Cancer. 2005; 103:299–306.
Article24. Shi M, Zhang CQ, Zhang YQ, Liang XM, Li JQ. Micrometastases of solitary hepatocellular carcinoma and appropriate resection margin. World J Surg. 2004; 28:376–381.
Article25. Shi M, Guo RP, Lin XJ, Zhang YQ, Chen MS, Zhang CQ, et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann Surg. 2007; 245:36–43.26. Hoffman AL, Wu SS, Obaid AK, French SW, Lois J, McMonigle M, et al. Histologic evaluation and treatment outcome after sequential radiofrequency ablation and hepatic resection for primary and metastatic tumors. Am Surg. 2002; 68:1038–1043.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Thermal Ablation of Hepatocellular Carcinomas
- Radiofrequency Ablation of Hepatic Cysts: Case Report
- Microwave thermosphere versus radiofrequency ablation for hepatocellular carcinoma: Are we approaching the time to end the debate?
- Current status and future of radiofrequency ablation for hepatocellular carcinoma
- Chemoembolization combined with radiofrequency ablation is the best option for the local treatment of early hepatocellular carcinoma?