Int J Stem Cells.
2017 Nov;10(2):154-159. 10.15283/ijsc17033.
Mesenchymal Stem Cell Differentiation into Adipocytes Is Equally Induced by Insulin and Proinsulin In Vitro
- Affiliations
-
- 1Pfützner Science & Health Institute, Mainz, Germany. Andreas.pfuetzner@pfuetzner-mainz.com
- 2Technical University of Applied Sciences, Bingen, Germany.
- 3Bonn-Rhein-Sieg University of Applied Sciences, Rheinbach, Germany.
- KMID: 2400869
- DOI: http://doi.org/10.15283/ijsc17033
Abstract
- BACKGROUND AND OBJECTIVES
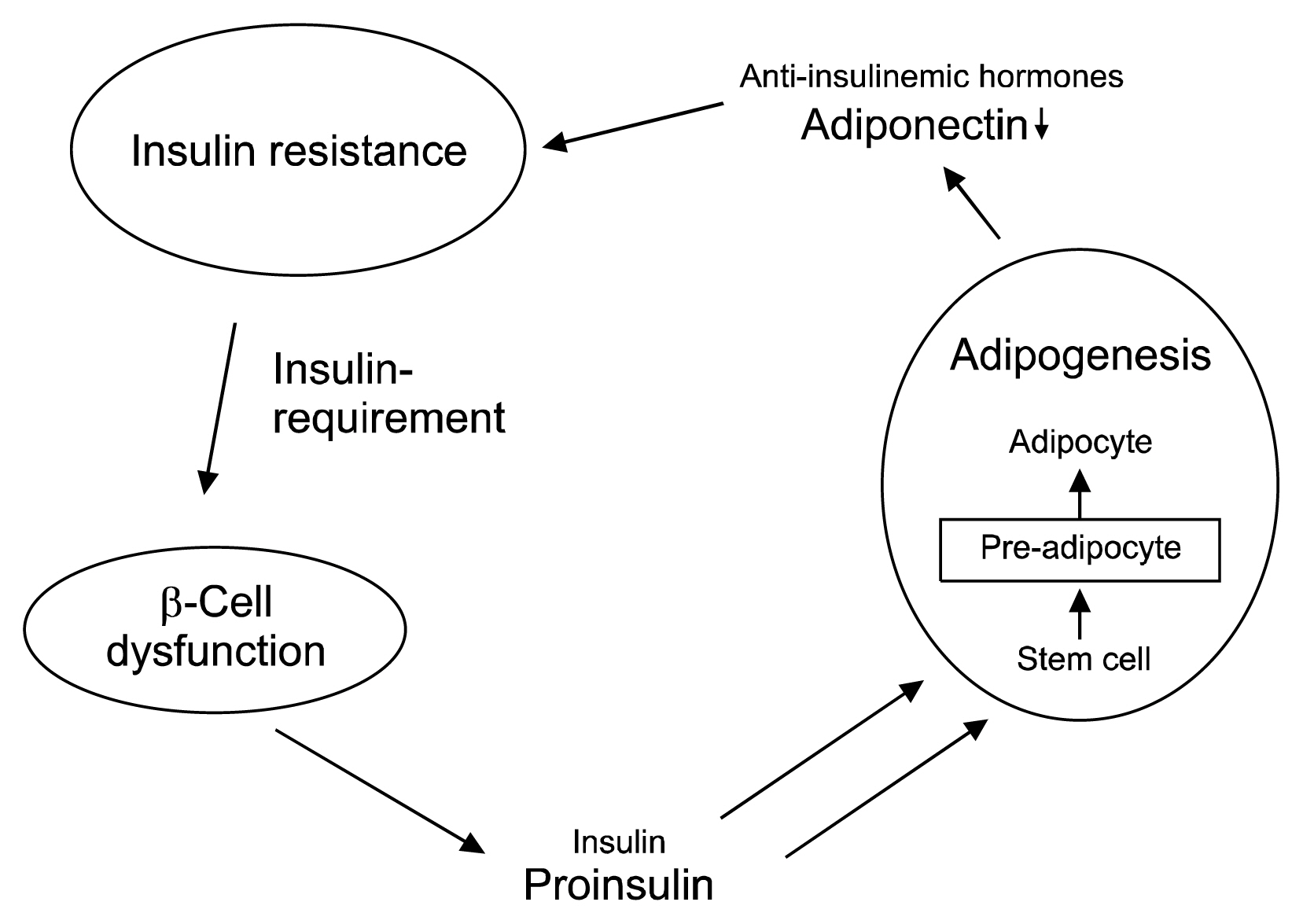
In advanced β-cell dysfunction, proinsulin is increasingly replacing insulin as major component of the secretion product. It has been speculated that proinsulin has at least the same adipogenic potency than insulin, leading to an increased tendency of lipid tissue formation in patients with late stage β-cell dysfunction.
METHODS AND RESULTS
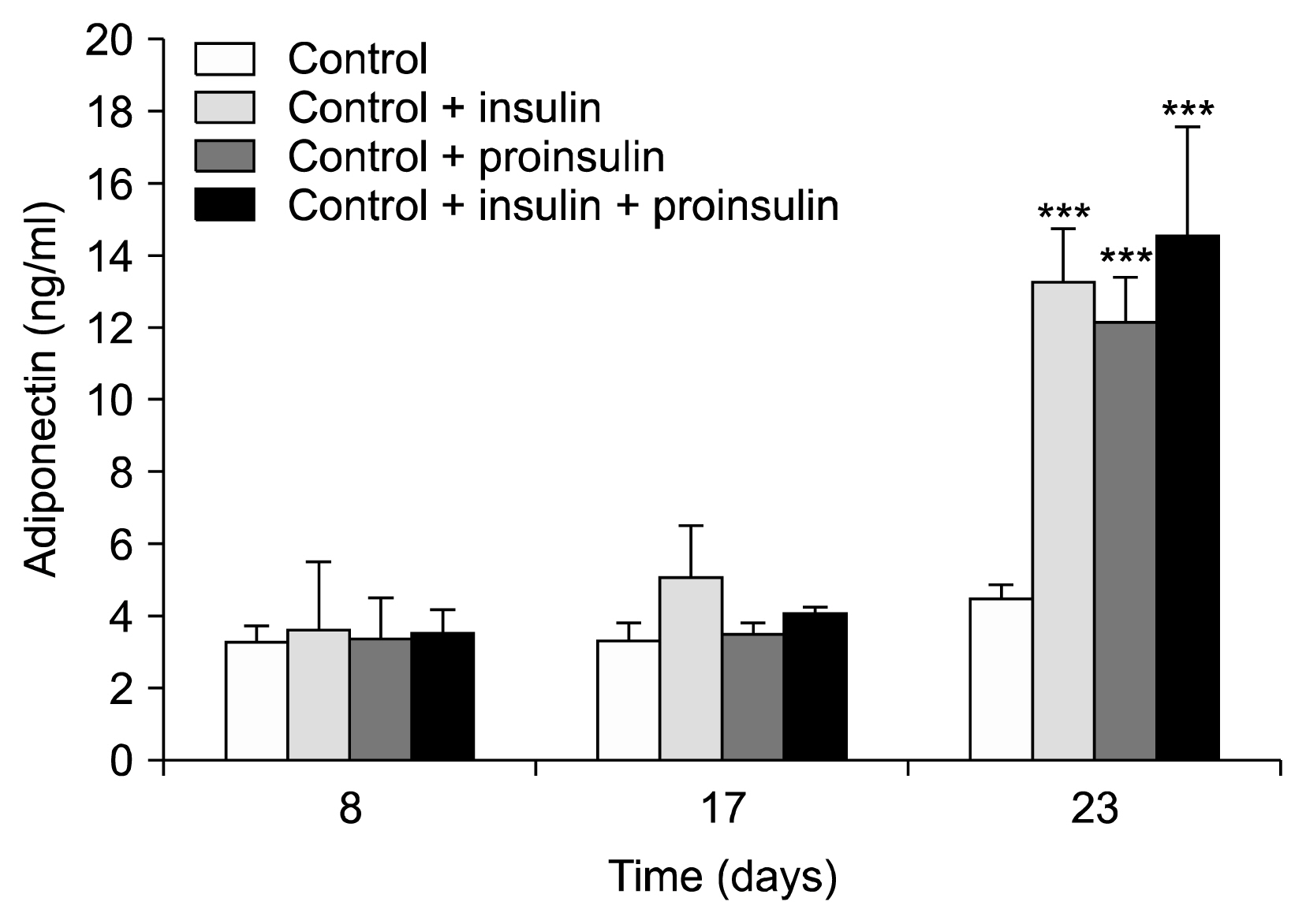
Mesenchymal stem cells obtained from liposuction material were grown in differentiation media containing insulin (0.01 μmol), proinsulin (0.01 μmol) or insulin+proinsulin (each 0.005 μmol). Cell culture supernatants were taken from these experiments and an untreated control at weeks 1, 2, and 3, and were stored at −80°C until analysis. Cell differentiation was microscopically supervised and adiponectin concentrations were measured as marker for differentiation into mature lipid cells. This experiment was repeated three times. No growth of lipid cells and no change in adiponectin values was observed in the negative control group (after 7/14/12 days: 3.2±0.5/3.3±0.1/4.4±0.5 ng/ml/12 h). A continuous differentiation into mature adipocytes (also confirmed by Red-Oil-staining) and a corresponding increase in adiponectin values was observed in the experiments with insulin (3.6±1.9/5.1±1.4/13.3±1.5 ng/ml/12 h; p < 0.05 week 1 vs. week 3) and proinsulin (3.3±1.2/3.5±0.3/12.2±1.2 ng/ml/12 h; p < 0.05). Comparable effects were seen with the insulin/proinsulin combination.
CONCLUSIONS
Proinsulin has the same adipogenic potential than insulin in vitro. Proinsulin has only 10~20% of the glucose-lowering effect of insulin. It can be speculated that the adipogenic potential of proinsulin may be a large contributor to the increased body weight problems in patients with type 2 diabetes and advanced β-cell dysfunction.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005; 115:1111–1119. DOI: 10.1172/JCI25102. PMID: 15864338. PMCID: 1087185.
Article2. Pfützner A, Weber MM, Forst T. A biomarker concept for assessment of insulin resistance, beta-cell function and chronic systemic inflammation in type 2 diabetes mellitus. Clin Lab. 2008; 54:485–490.3. Pfützner A, Kunt T, Hohberg C, Mondok A, Pahler S, Konrad T, Lübben G, Forst T. Fasting intact proinsulin is a highly specific predictor of insulin resistance in type 2 diabetes. Diabetes Care. 2004; 27:682–687. DOI: 10.2337/diacare.27.3.682. PMID: 14988285.
Article4. Pfützner A, Pfützner AH, Larbig M, Forst T. Role of intact proinsulin in diagnosis and treatment of type 2 diabetes mellitus. Diabetes Technol Ther. 2004; 6:405–412. DOI: 10.1089/152091504774198124. PMID: 15198846.
Article5. Glauber HS, Henry RR, Wallace P, Frank BH, Galloway JA, Cohen RM, Olefsky JM. The effects of biosynthetic human proinsulin on carbohydrate metabolism in non-insulin-dependent diabetes mellitus. N Engl J Med. 1987; 316:443–449. DOI: 10.1056/NEJM198702193160805. PMID: 3543679.
Article6. Galloway JA, Hooper SA, Spradlin CT, Howey DC, Frank BH, Bowsher RR, Anderson JH. Biosynthetic human proinsulin. Review of chemistry, in vitro and in vivo receptor binding, animal and human pharmacology studies, and clinical trial experience. Diabetes Care. 1992; 15:666–692. DOI: 10.2337/diacare.15.5.666. PMID: 1516487.
Article7. American Diabetes Association. Standards in diabetes care 2017. Diabetes Care. 2017; 40(Suppl 1):S1–S135.8. Ivy JL. Role of exercise training in the prevention and treatment of insulin resistance and non-insulin-dependent diabetes mellitus. Sports Med. 1997; 24:321–336. DOI: 10.2165/00007256-199724050-00004. PMID: 9368278.
Article9. Wallberg-Henriksson H, Rincon J, Zierath JR. Exercise in the management of non-insulin-dependent diabetes mellitus. Sports Med. 1998; 25:25–35. DOI: 10.2165/00007256-199825010-00003. PMID: 9458525.
Article10. Janderová L, McNeil M, Murrell AN, Mynatt RL, Smith SR. Human mesenchymal stem cells as an in vitro model for human adipogenesis. Obes Res. 2003; 11:65–74. DOI: 10.1038/oby.2003.11. PMID: 12529487.
Article11. Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001; 7:211–228. DOI: 10.1089/107632701300062859. PMID: 11304456.
Article12. Zhu M, Heydarkhan-Hagvall S, Hedrick M, Benhaim P, Zuk P. Manual isolation of adipose-derived stem cells from human lipoaspirates. J Vis Exp. 2013; (79):e50585. PMID: 24121366. PMCID: 3935774.
Article13. Pansky A, Roitzheim B, Tobiasch E. Differentiation potential of adult human mesenchymal stem cells. Clin Lab. 2007; 53:81–84. PMID: 17323830.14. Nagahara K, Dobashi K, Ishikawa T, Nakano Y, Abe Y, Tanaka D, Itabashi K. AICAR attenuates TNFα-induced inappropriate secretion of monocyte chemoattractant protein-1 and adiponectin in 3T3-L1 adipocytes. J Atheroscler Thromb. 2016; 23:1345–1354. DOI: 10.5551/jat.34835. PMID: 27170207. PMCID: 5221497.
Article15. Huypens P, Quartier E, Pipeleers D, Van de Casteele M. Metformin reduces adiponectin protein expression and release in 3T3-L1 adipocytes involving activation of AMP activated protein kinase. Eur J Pharmacol. 2005; 518:90–95. DOI: 10.1016/j.ejphar.2005.06.016. PMID: 16039647.
Article16. Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999; 284:143–147. DOI: 10.1126/science.284.5411.143. PMID: 10102814.
Article17. Contador D, Ezquer F, Espinosa M, Arango-Rodriguez M, Puebla C, Sobrevia L, Conget P. Dexamethasone and rosiglitazone are sufficient and necessary for producing functional adipocytes from mesenchymal stem cells. Exp Biol Med (Maywood). 2015; 240:1235–1246. DOI: 10.1177/1535370214566565.
Article18. Pfützner A, Hermanns I, Ramljak S, Demircik F, Pfützner AH, Kann PH, Weber MM. Elevated intact proinsulin levels during an oral glucose challenge indicate progressive β-cell dysfunction and may be predictive for development of type 2 diabetes. J Diabetes Sci Technol. 2015; 9:1307–1312. DOI: 10.1177/1932296815607862.
Article19. Vangipurapu J, Stančáková A, Kuulasmaa T, Kuusisto J, Laakso M. Both fasting and glucose-stimulated proinsulin levels predict hyperglycemia and incident type 2 diabetes: a population-based study of 9,396 Finnish men. PLoS One. 2015; 10:e0124028. DOI: 10.1371/journal.pone.0124028. PMID: 25853252. PMCID: 4390238.
Article20. Zethelius B, Byberg L, Hales CN, Lithell H, Berne C. Proinsulin and acute insulin response independently predict Type 2 diabetes mellitus in men--report from 27 years of follow-up study. Diabetologia. 2003; 46:20–26. DOI: 10.1007/s00125-002-0995-2. PMID: 12637978.
Article21. Nijpels G, Popp-Snijders C, Kostense PJ, Bouter LM, Heine RJ. Fasting proinsulin and 2-h post-load glucose levels predict the conversion to NIDDM in subjects with impaired glucose tolerance: the Hoorn Study. Diabetologia. 1996; 39:113–118. PMID: 8720611.
Article22. Kahn SE, Leonetti DL, Prigeon RL, Boyko EJ, Bergstrom RW, Fujimoto WY. Proinsulin as a marker for the development of NIDDM in Japanese-American men. Diabetes. 1995; 44:173–179. DOI: 10.2337/diab.44.2.173. PMID: 7859937.
Article23. Zethelius B, Byberg L, Hales CN, Lithell H, Berne C. Proinsulin is an independent predictor of coronary heart disease: Report from a 27-year follow-up study. Circulation. 2002; 105:2153–2158. DOI: 10.1161/01.CIR.0000015855.04844.E7. PMID: 11994248.
Article24. Lindahl B, Dinesen B, Eliasson M, Røder M, Hallmans G, Stegmayr B. High proinsulin levels precede first-ever stroke in a nondiabetic population. Stroke. 2000; 31:2936–2941. DOI: 10.1161/01.STR.31.12.2936. PMID: 11108752.
Article25. Lindahl B, Dinesen B, Eliasson M, Røder M, Jansson JH, Huhtasaari F, Hallmans G. High proinsulin concentration precedes acute myocardial infarction in a nondiabetic population. Metabolism. 1999; 48:1197–1202. DOI: 10.1016/S0026-0495(99)90138-5. PMID: 10484064.
Article26. Kuryszko J, Sławuta P, Sapikowski G. Secretory function of adipose tissue. Pol J Vet Sci. 2016; 19:441–446. PMID: 27487522.
Article27. Nordt TK, Bode C, Sobel BE. Stimulation in vivo of expression of intra-abdominal adipose tissue plasminogen activator inhibitor Type I by proinsulin. Diabetologia. 2001; 44:1121–1124. DOI: 10.1007/s001250100618. PMID: 11596666.
Article28. Frühbeck G. Overview of adipose tissue and its role in obesity and metabolic disorders. Methods Mol Biol. 2008; 456:1–22. DOI: 10.1007/978-1-59745-245-8_1. PMID: 18516549.
Article29. Schöndorf T, Maiworm A, Emmison N, Forst T, Pfützner A. Biological background and role of adiponectin as marker for insulin resistance and cardiovascular risk. Clin Lab. 2005; 51:489–494. PMID: 16285470.30. Galic S, Oakhill JS, Steinberg GR. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010; 316:129–139. DOI: 10.1016/j.mce.2009.08.018.
Article31. Ghanim H, Aljada A, Hofmeyer D, Syed T, Mohanty P, Dandona P. Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation. 2004; 110:1564–1571. DOI: 10.1161/01.CIR.0000142055.53122.FA. PMID: 15364812.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Histone Acetylation in Mesenchymal Stem Cell Differentiation
- Serum insulin, proinsulin, and proinsulin/insulin ratio in type 2 diabetic patients
- Adult Mesenchymal Stem Cells for Cell Therapy in Clinical Application
- Serum Insulin, Proinsulin and Proinsulin/Insulin Ratio in Type 2 Diabetic Patients: As an Index of beta-Cell Function or Insulin Resistance
- Plasma Proinsulin Levels among the Control, Impaired Glucose Tolerance and Type 2 Diabetes Mellitus during Oral Glucose Tolerance Test