Ann Rehabil Med.
2017 Dec;41(6):935-943. 10.5535/arm.2017.41.6.935.
Effects of Overactive Bladder Symptoms in Stroke Patients' Health Related Quality of Life and Their Performance Scale
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, National Rehabilitation Center, Seoul, Korea. silverzookim@gmail.com
- 2Department of Urology, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2400277
- DOI: http://doi.org/10.5535/arm.2017.41.6.935
Abstract
OBJECTIVE
To identify the effects of overactive bladder (OAB) symptoms on the health-related quality of life (HRQOL) in stroke patients since OAB symptoms are common in such patients, but their effects on stroke rehabilitation over time are unclear.
METHODS
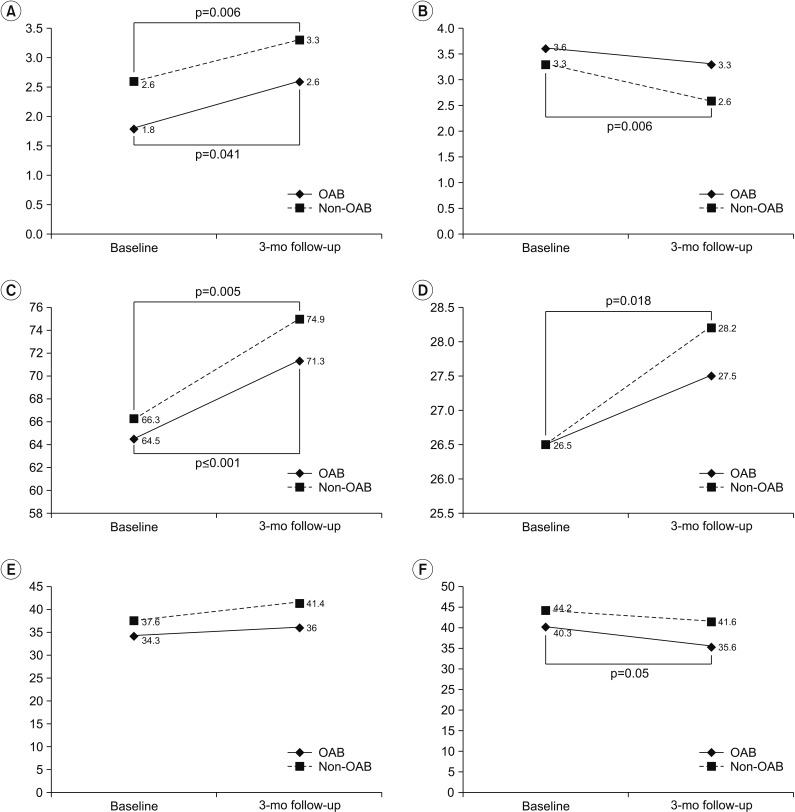
This study included 30 post-acute stroke patients who had been admitted for rehabilitation treatments. All participants completed a questionnaire evaluating urinary symptoms, including the Overactive Bladder Symptom Score (OABSS) and general HRQOL with a Short-Form 36 (SF-36) health survey. We assessed their performance in terms of the Function Ambulation Category, Modified Rankin Scale (MRS), Modified Barthel Index, and Mini-Mental State Examination (MMSE). All assessments were carried out twice at baseline and at 3 months. We divided patients into an OAB and non-OAB group with OABSS. A correlation analysis and multivariate regression were then performed.
RESULTS
All performance scales showed an improvement over 3 months in the non-OAB group (n=18; p < 0.02), but, MRS and MMSE scores did not improve significantly in the OAB group (n=12) (p=0.15 and p=0.20, respectively). In the OAB group, the vitality and mental health scores significantly decreased over 3 months (p=0.011 and p=0,041, respectively), and the mental component summary (MCS) score showed a marginal decrease over 3 months (p=0.05). A multivariate regression analysis revealed that OAB symptoms were negatively correlated with the 3 months MCS score (B=−8.15, p=0.034).
CONCLUSION
These results indicated that OAB symptoms could have negative effects on HRQOL and performance in patients suffering from a stroke.
Keyword
MeSH Terms
Figure
Reference
-
1. Brittain KR, Peet SM, Castleden CM. Stroke and incontinence. Stroke. 1998; 29:524–528. PMID: 9472900.
Article2. Brittain KR, Perry SI, Peet SM, Shaw C, Dallosso H, Assassa RP, et al. Prevalence and impact of urinary symptoms among community-dwelling stroke survivors. Stroke. 2000; 31:886–891. PMID: 10753993.
Article3. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.
Article4. Liberman JN, Hunt TL, Stewart WF, Wein A, Zhou Z, Herzog AR, et al. Health-related quality of life among adults with symptoms of overactive bladder: results from a U.S. community-based survey. Urology. 2001; 57:1044–1050. PMID: 11377301.
Article5. Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001; 87:760–766. PMID: 11412210.
Article6. Jo JK, Lee S, Kim YT, Choi HY, Kim SA, Choi BY, et al. Analysis of the risk factors for overactive bladder on the basis of a survey in the community. Korean J Urol. 2012; 53:541–546. PMID: 22949998.
Article7. Sexton CC, Coyne KS, Thompson C, Bavendam T, Chen CI, Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older Americans: results from the epidemiology of lower urinary tract symptoms study. J Am Geriatr Soc. 2011; 59:1465–1470. PMID: 21718275.
Article8. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003; 20:327–336. PMID: 12811491.
Article9. Wein AJ, Rovner ES. Definition and epidemiology of overactive bladder. Urology. 2002; 60(5 Suppl 1):7–12.
Article10. Itoh Y, Yamada S, Konoeda F, Koizumi K, Nagata H, Oya M, et al. Burden of overactive bladder symptom on quality of life in stroke patients. Neurourol Urodyn. 2013; 32:428–434. PMID: 23129306.
Article11. Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003; 82:327–338. PMID: 14499979.
Article12. Stoffel JT, Peterson AC, Sandhu JS, Suskind AM, Wei JT, Lightner DJ, et al. AUA white paper on nonneurogenic chronic urinary retention: consensus definition, treatment, algorithm, and outcome endpoints. J Urol. 2017; 198:153–160. PMID: 28163030.13. Yamaguchi O, Nishizawa O, Takeda M, Yokoyama O, Homma Y, Kakizaki H, et al. Clinical guidelines for overactive bladder. Int J Urol. 2009; 16:126–142. PMID: 19228224.
Article14. Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome: overactive bladder symptom score. Urology. 2006; 68:318–323. PMID: 16904444.15. Jeong SJ, Homma Y, Oh SJ. Korean version of the overactive bladder symptom score questionnaire: translation and linguistic validation. Int Neurourol J. 2011; 15:135–142. PMID: 22087422.
Article16. Gandek B, Sinclair SJ, Kosinski M, Ware JE Jr. Psychometric evaluation of the SF-36 health survey in Medicare managed care. Health Care Financ Rev. 2004; 25:5–25.17. Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history and effects on 2-year outcomes of urinary incontinence after stroke. Stroke. 2001; 32:122–127. PMID: 11136926.
Article18. Tibaek S, Gard G, Klarskov P, Iversen HK, Dehlendorff C, Jensen R. Prevalence of lower urinary tract symptoms (LUTS) in stroke patients: a cross-sectional, clinical survey. Neurourol Urodyn. 2008; 27:763–771. PMID: 18551565.
Article19. Williams MP, Srikanth V, Bird M, Thrift AG. Urinary symptoms and natural history of urinary continence after first-ever stroke: a longitudinal populationbased study. Age Ageing. 2012; 41:371–376. PMID: 22321907.20. Willis-Gray MG, Dieter AA, Geller EJ. Evaluation and management of overactive bladder: strategies for optimizing care. Res Rep Urol. 2016; 8:113–122. PMID: 27556018.21. Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am. 2016; 43:289–297. PMID: 27476122.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relating Factor and Quality of Life of Overactive Bladder in Adults
- Antimuscarinic Agent Treatment Affecting Patient-Reported Outcomes in Overactive Bladder Syndrome With Depressive Symptoms
- The Prevalence and Quality of Life of Overactive Bladder and Urinary Incontinence in Young Women
- Review of the Anticholinergics for the Treatment of Overactive Bladder: 2009 Update
- The Impact of Overactive Bladder on Health-Related Quality of Life, Sexual Life and Psychological Health in Korea