J Dent Anesth Pain Med.
2017 Dec;17(4):297-305. 10.17245/jdapm.2017.17.4.297.
Learning fiberoptic intubation for awake nasotracheal intubation
- Affiliations
-
- 1Department of Dental Anesthesiology, School of Dentistry, Seoul National University, Seoul, Korea. stone90@snu.ac.kr
- 2Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea.
- KMID: 2399800
- DOI: http://doi.org/10.17245/jdapm.2017.17.4.297
Abstract
- BACKGROUND
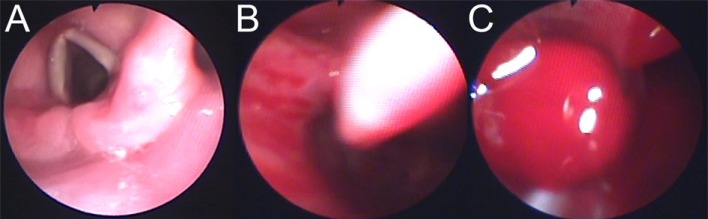
Fiberoptic nasotracheal intubation (FNI) is performed if it is difficult to open the mouth or if intubation using laryngoscope is expected to be difficult. However, training is necessary because intubation performed by inexperienced operators leads to complications.
METHODS
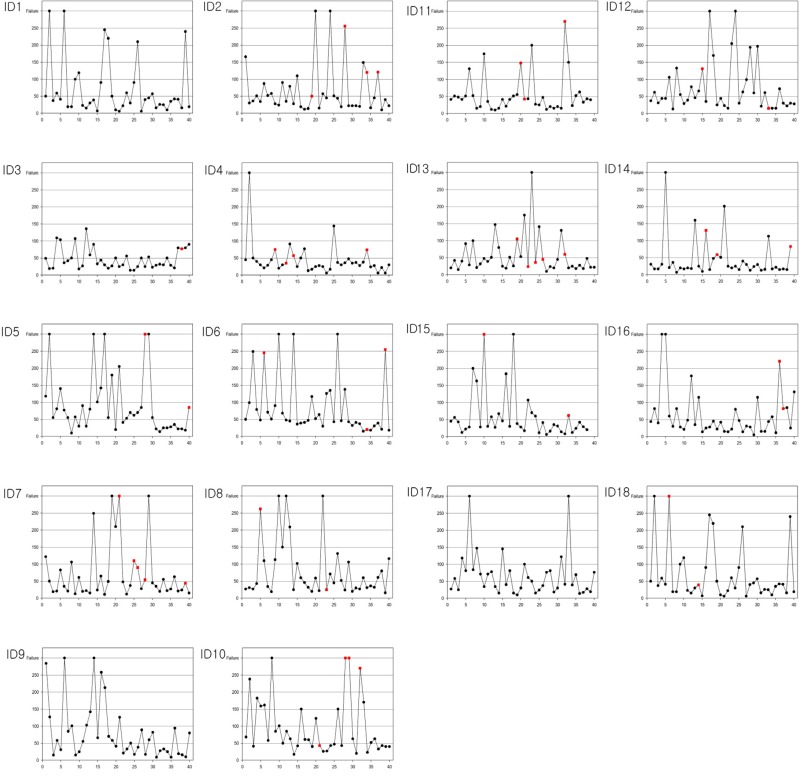
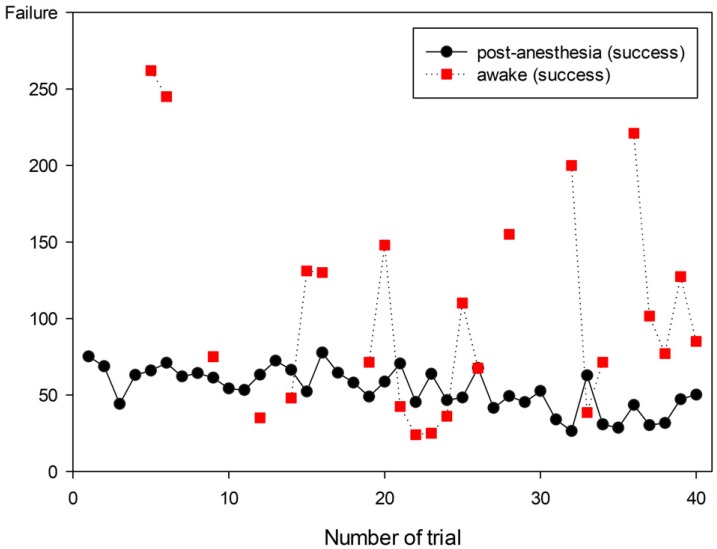
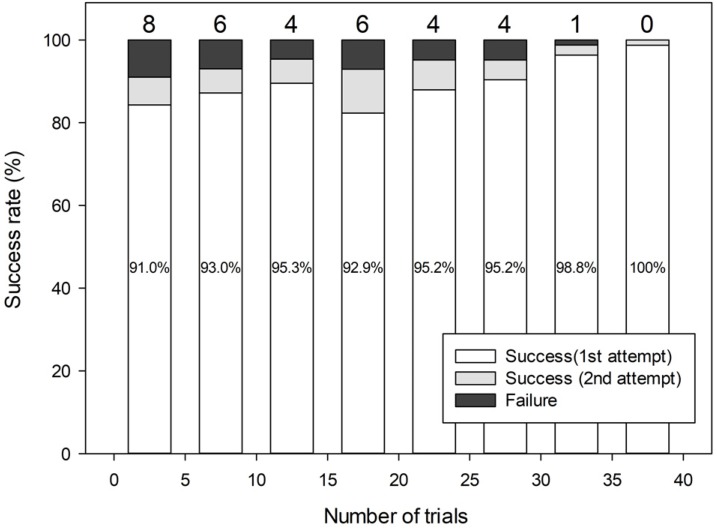
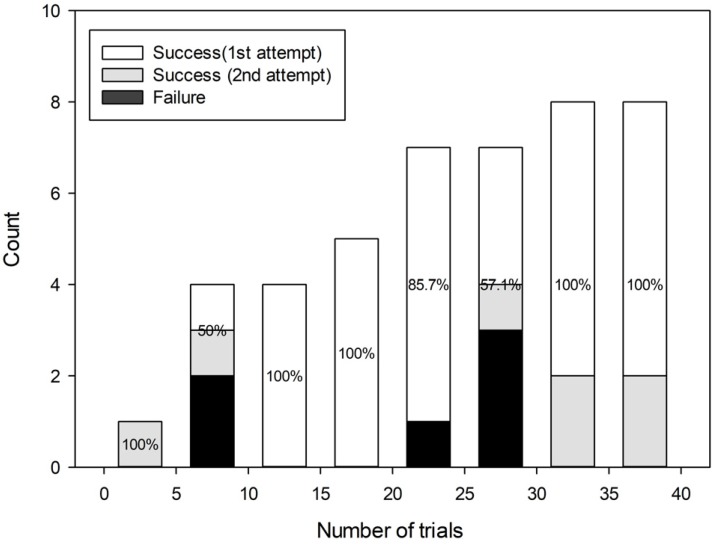
Every resident performed intubation in 40 patients. Success of FNI was evaluated as the time of FNI. First intubation time was restricted to 2 min 30 s. If the second attempt was unsuccessful, it was considered a failed case, and a specialist performed nasotracheal intubation. If the general method of intubation was expected to be difficult, awake intubation was performed. The degree of nasal bleeding during intubation was also evaluated.
RESULTS
The mean age of the operators (11 men, 7 women) was 27.8 years. FNI was performed in a total of 716 patients. The success rate was 88.3% for the first attempt and 94.6% for the second attempt. The failure rate of intubation in anesthetized patients was 4.9%, and 13.6% in awake patients. When intubation was performed in anesthetized patients, the failure rate from the first to fifth trial was 9.6%, which decreased to 0.7% when the number of trials increased to > 30 times. In terms of awake intubation, there was no failed attempt when the resident had performed the FNI > 30 times. The number of FNIs performed and nasal bleeding were important factors influencing the failure rate.
CONCLUSION
The success rate of FNI increased as the number of FNI performed by residents increased despite the nasal bleeding.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Orotracheal intubation in a patient with difficult airway by using fiberoptic nasotracheal intubation: A case report
Hye Joo Yun, Eunsun So, Myong-Hwan Karm, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2018;18(2):125-128. doi: 10.17245/jdapm.2018.18.2.125.
Reference
-
1. Mahmood S, Lowe T. Management of epistaxis in the oral and maxillofacial surgery setting: An update on current practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:23–29. PMID: 12539023.
Article2. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the american society of anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013; 118:251–270. PMID: 23364566.3. Delaney KA, Hessler R. Emergency flexible fiberoptic nasotracheal intubation: A report of 60 cases. Ann Emerg Med. 1988; 17:919–926. PMID: 3415064.
Article4. Ovassapian A, Yelich SJ, Dykes MH, Brunner EE. Fiberoptic nasotracheal intubation--incidence and causes of failure. Anesth Analg. 1983; 62:692–695. PMID: 6859572.
Article5. Smith JE, Jackson AP, Hurdley J, Clifton PJ. Learning curves for fibreoptic nasotracheal intubation when using the endoscopic video camera. Anaesthesia. 1997; 52:101–106. PMID: 9059089.
Article6. Ovassapian A, Yelich SJ, Dykes MH, Golman ME. Learning fibreoptic intubation: Use of simulators v. Traditional teaching. Br J Anaesth. 1988; 61:217–220. PMID: 3415894.7. Dalal PG, Dalal GB, Pott L, Bezinover D, Prozesky J, Bosseau Murray W. Learning curves of novice anesthesiology residents performing simulated fibreoptic upper airway endoscopy. Can J Anaesth. 2011; 58:802–809. PMID: 21710368.
Article8. Johnson C, Roberts JT. Clinical competence in the performance of fiberoptic laryngoscopy and endotracheal intubation: A study of resident instruction. J Clin Anesth. 1989; 1:344–349. PMID: 2627408.9. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990; 72:828–833. PMID: 2339799.
Article10. Bailie R, Posner KL. New trends in adverse respiratory events. ASA Newsl. 2011; 75:28–29.11. Huitink JM, Lie PP, Heideman I, Jansma P, Greif R, Schagen Nv, et al. A prospective, cohort evaluation of major and minor airway management complications during routine anaesthetic care at an academic medical centre. Anaesthesia. 2017; 72:42–48. PMID: 27665740.
Article12. Buis ML, Maissan IM, Hoeks SE, Klimek M, Stolker RJ. Defining the learning curve for endotracheal intubation using direct laryngoscopy: A systematic review. Resuscitation. 2016; 99:63–71. PMID: 26711127.
Article13. Ovassapian A. Fiberoptic tracheal intubation. Fiberoptic Airway Endoscopy in Anesthesia and Critical Care. New York: Raven Press;1990. p. 57–79.14. Korttila K, Tarkkanen J, Tarkkanen L. Comparison of laryngotracheal and ultrasonic nebulizer administration of lidocaine in local anaesthesia for bronchoscopy. Acta Anaesthesiol Scand. 1981; 25:161–165. PMID: 7324824.
Article15. Somerson SJ, Sicilia MR. AANA journal course: update for nurse anesthetists--beyond the laryngoscope: advanced techniques for difficult airway management. AANA J. 1993; 61:64–71. PMID: 8368059.16. Machata AM, Gonano C, Holzer A, Andel D, Spiss CK, Zimpfer M, et al. Awake nasotracheal fiberoptic intubation: Patient comfort, intubating conditions, and hemodynamic stability during conscious sedation with remifentanil. Anesth Analg. 2003; 97:904–908. PMID: 12933427.
Article17. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39:1105–1111. PMID: 6507827.
Article18. Collins SR, Blank RS. Fiberoptic intubation: An overview and update. Respir Care. 2014; 59:865–878. PMID: 24891196.
Article19. K Nasa V, Kamath SS. Risk factors assessment of the difficult intubation using intubation difficulty scale (IDS). J Clin Diagn Res. 2014; 8:GC01–GC03.20. Kim HW, Seo KS, Shin TJ, Kim HJ. The effect of laryngeal view grade and intraoral bleeding on intubation difficulty during fiberoptic nasotracheal intubation. J Korean Dent Soc Anesthesiol. 2009; 9:91–97.
Article21. Sanuki T, Hirokane M, Kotani J. Epistaxis during intubation: A comparison of nostril sides. J Oral Maxillofac Surg. 2010; 68:618–621. PMID: 19931965.22. Lai HC, Chang YH, Huang RC, Hung NK, Lu CH, Chen JH, et al. Efficacy of sevoflurane as an adjuvant to propofol-based total intravenous anesthesia for attenuating secretions in ocular surgery. Medicine. 2017; 96:e6729. PMID: 28445291.
Article23. O'Connell JE, Stevenson DS, Stokes MA. Pathological changes associated with short-term nasal intubation. Anaesthesia. 1996; 51:347–350. PMID: 8686823.24. Morimoto Y, Sugimura M, Hirose Y, Taki K, Niwa H. Nasotracheal intubation under curve-tipped suction catheter guidance reduces epistaxis. Can J Anaesth. 2006; 53:295–298. PMID: 16527796.
Article25. Elwood T, Stillions DM, Woo DW, Bradford HM, Ramamoorthy C. Nasotracheal intubation: A randomized trial of two methods. Anesthesiology. 2002; 96:51–53. PMID: 11753001.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blind Intubation Using Fiberoptic Bronchoscope in Epistaxis
- Effective removal of epistaxis during nasotracheal intubation utilizing a fiberoptic scope in a difficult airway: A case report
- Use of the Airtraq(R) optical laryngoscope as a rescue airway device following failed awake flexible fiberoptic nasotracheal intubation of a patient with severe microsomia: A case report
- The Chanages of Blood Pressure , Heart Rate and Cardiac Output During Awake Fiberoptic Nasotracheal and Orotracheal Intubation
- Atelectasis Due to Epistaxis Aspiration during Awake Fiberoptic Nasotracheal Intubation