Ann Dermatol.
2018 Feb;30(1):29-35. 10.5021/ad.2018.30.1.29.
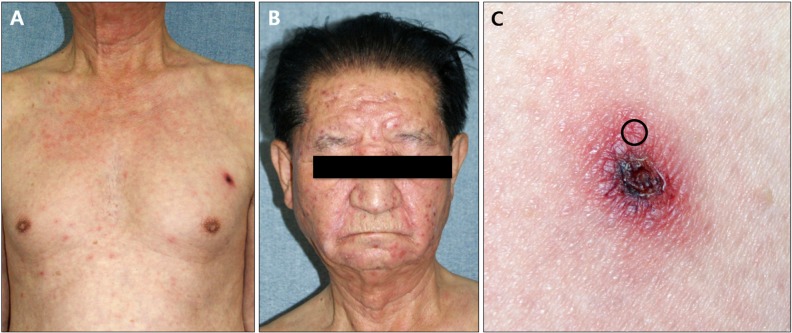
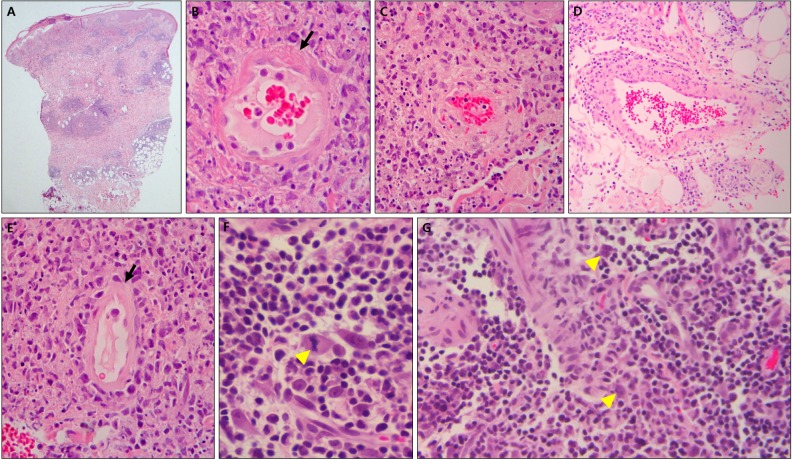
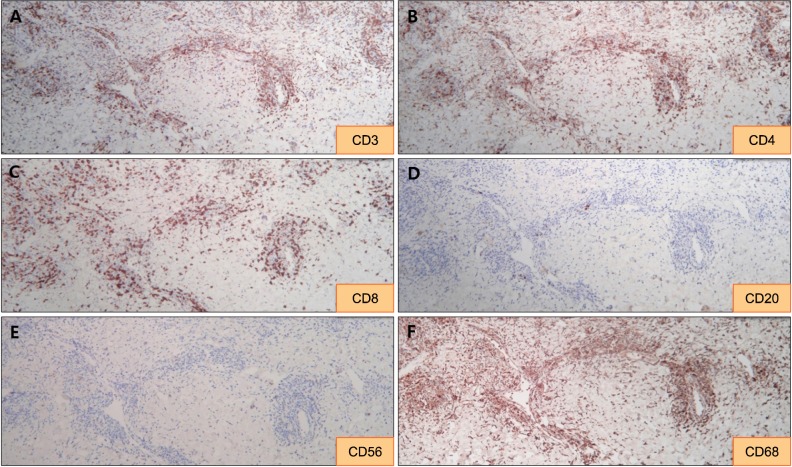
Histopathologic Finding of Perieschar Lesions in Tsutsugamushi Disease Shows Lymphocytic Vasculitis Mimicking Angiocentric Lymphoma
- Affiliations
-
- 1Department of Dermatology, Kosin University College of Medicine, Busan, Korea. ksderm98@unitel.co.kr
- 2Department of Dermatology, Maryknoll Medical Center, Busan, Korea.
- KMID: 2399751
- DOI: http://doi.org/10.5021/ad.2018.30.1.29
Abstract
- BACKGROUND
Tsutsugamushi disease is an acute, febrile, infectious disease caused by Orientia tsutsugamushi. Several studies investigating the histopathologic findings of eschars in tsutsugamushi disease reported leukocytoclastic vasculitis and neutrophil infiltration as the major findings. However, these findings may result from secondary changes following tissue necrosis. The histopathologic findings of perieschar lesions may be important to understand the primary changes associated with tsutsugamushi disease.
OBJECTIVE
To investigate characteristic histopathologic features of perieschar lesions and suppose the mechanism of vascular pathophysiological changes associated with tsutsugamushi disease.
METHODS
We analyzed histopathological slides of perieschar lesions in 12 patients diagnosed with tsutsugamushi disease.
RESULTS
In the epidermis, exocytosis of mononuclear cells (75.0%) and basal vacuolar changes (66.7%) were frequent. In the dermis, perivascular, interstitial, and perineural mononuclear cell infiltration (100.0%, 83.3%, and 83.3%, respectively), as well as thrombosis (83.3%), atypical lymphocyte infiltration (91.7%), and mitotic figures (83.3%) were commonly seen. Lymphocytic vasculitis and mononuclear cell infiltration around eccrine glands were found in all cases, but eosinophil infiltration was only found in one patient (8.3%). However, the characteristic findings of eschar lesions, such as leukocytoclastic vasculitis and neutrophil infiltration, were not found in perieschar lesions.
CONCLUSION
The major histopathologic findings in the perieschar lesions of tsutsugamushi disease were lymphocytic vasculitis and atypical lymphocytic infiltration, mimicking lymphoma. Therefore, we suggest that this lesion should be added to the list of pseudolymphomas. To observe these characteristic histopathologic features, we also recommend that skin biopsies should be performed on perieschar lesions, not eschar lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Ogawa M, Hagiwara T, Kishimoto T, Shiga S, Yoshida Y, Furuya Y, et al. Scrub typhus in Japan: epidemiology and clinical features of cases reported in 1998. Am J Trop Med Hyg. 2002; 67:162–165. PMID: 12389941.
Article2. Chaudhary N, Lee JS, Wu JY, Tharin S. Evidence for use of teriparatide in spinal fusion surgery in osteoporotic patients. World Neurosurg. 2017; 100:551–556. PMID: 27923758.
Article3. Hu ML, Liu JW, Wu KL, Lu SN, Chiou SS, Kuo CH, et al. Short report: abnormal liver function in scrub typhus. Am J Trop Med Hyg. 2005; 73:667–668. PMID: 16222006.4. Allen AC, Spitz S. A comparative study of the pathology of scrub typhus (tsutsugamushi disease) and other rickettsial diseases. Am J Pathol. 1945; 21:603–681. PMID: 19970829.5. Seong SY, Choi MS, Kim IS. Orientia tsutsugamushi infection: overview and immune responses. Microbes Infect. 2001; 3:11–21. PMID: 11226850.6. Soter NA. Cutaneous necrotizing venulitis. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw Hill;2012. p. 2003–2008.7. Mekkes JR, Loots MA, van der Wal AC, Bos JD. Increased incidence of hypercoagulability in patients with leg ulcers caused by leukocytoclastic vasculitis. J Am Acad Dermatol. 2004; 50:104–107. PMID: 14699376.
Article8. Barksdale SK, Scumpia P, Wang JY, Xu X, Barnhill RL. Vascular disease. In : Elder DE, Elinitsas R, Rosenbach M, Murphy GF, Rubin AI, Xu X, editors. Lever's histopathology of the skin. 11th ed. Philadelphia: Lippincott William & Wilkins;2015. p. 240–275.9. Massa MC, Su WP. Lymphocytic vasculitis: is it a specific clinicopathologic entity? J Cutan Pathol. 1984; 11:132–139. PMID: 6736395.
Article10. Kossard S. Defining lymphocytic vasculitis. Australas J Dermatol. 2000; 41:149–155. PMID: 10954985.
Article11. Paris DH, Phetsouvanh R, Tanganuchitcharnchai A, Jones M, Jenjaroen K, Vongsouvath M, et al. Orientia tsutsugamushi in human scrub typhus eschars shows tropism for dendritic cells and monocytes rather than endothelium. PLoS Negl Trop Dis. 2012; 6:e1466. PMID: 22253938.
Article12. Chi DH, Huh JR, Sung KJ, Koh JK. Epstein-Barr virus associated cutaneous angiocetric immunoproliferative lesion showing histologic features of classical lymphomatoid granulomatosis. Ann Dermatol. 1996; 8:110–113.13. Cerroni L. Other cutaneous B-cell lymphomas. In : Cerroni L, editor. Skin lymphoma: the illustrated guide. 4th ed. Oxford: Wiley-Blackwell;2014. p. 253–256.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Angiocentric Lymphoma Mimicking Behcet's Disease
- Angiocentric T - cell Lymphoma: Clinical and Histopathologic Features of Four Patients
- Angiocentric T cell Lymphoma associated with Epstein-Barr Virus
- A Case of Angiocentic T-Cell Lymphoma Achieving Initial Complete Remission with CVP Chemotherapy
- Subcutaneous Panniculitic Angiocentric T/NK-Cell Lymphoma