Imaging Sci Dent.
2017 Dec;47(4):255-259. 10.5624/isd.2017.47.4.255.
CT evaluation of underlying bone sclerosis in patients with oral squamous cell carcinoma: A preliminary retrospective study
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea. future3@snu.ac.kr
- KMID: 2397840
- DOI: http://doi.org/10.5624/isd.2017.47.4.255
Abstract
- PURPOSE
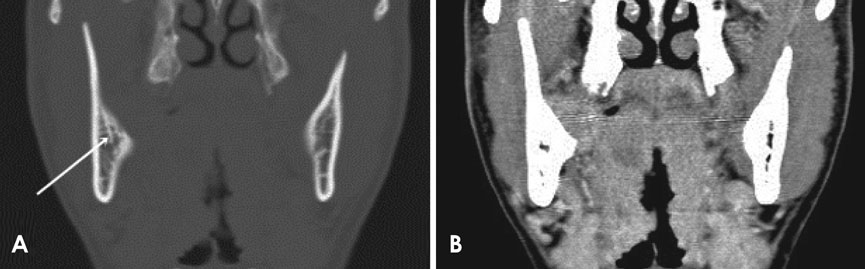
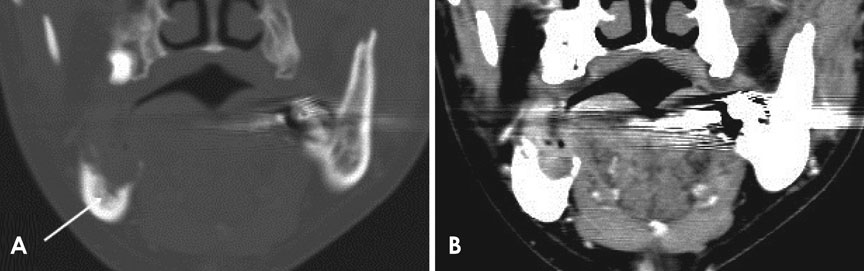
Underlying bone sclerosis is frequently observed in clinical settings when oral squamous cell carcinoma (OSCC) invades the jaw bone. The aim of this study was to assess the prevalence and characteristics of underlying bone sclerosis in patients with OSCC.
MATERIALS AND METHODS
We retrospectively reviewed the computed tomographic (CT) images of 131 patients who underwent mandibulectomy between January 2012 and December 2015 to treat OSCC. The presence, degree, and extent of underlying bone sclerosis were assessed on CT images and correlated with the following imaging patterns of bone invasion: cortical invasion, medullary invasion with a smooth margin, and medullary invasion with an irregular margin. The chi-square test was used to determine the relationships between the variables.
RESULTS
The prevalence of underlying bone sclerosis on CT images was 70.1% (47 of 67). The prevalence was 85.7% (42 of 49) in patients with medullary invasion, but it was 27.8% (5 of 18) in patients with only cortical invasion, indicating a significant increase in the prevalence of underlying bone sclerosis in patients with medullary invasion (P < .05). Aggressive patterns of bone invasion were associated with increases in the degree and extent of the underlying bone sclerosis (P < .05).
CONCLUSION
More than two-thirds of OSCC cases with bone invasion showed underlying bone sclerosis. On CT images, reactive sclerosis in the remaining margin of the alveolar bone should not be used as the primary means to differentiate periodontal inflammatory lesions from those resulting from OSCC.
MeSH Terms
Figure
Reference
-
1. Hoffmannová J, Foltán R, Vlk M, Sipos M, Horká E, Pavliková G, et al. Hemimandibulectomy and therapeutic neck dissection with radiotherapy in the treatment of oral squamous cell carcinoma involving mandible: a critical review of treatment protocol in the years 1994-2004. Int J Oral Maxillofac Surg. 2010; 39:561–567.
Article2. Lubek J, El-Hakim M, Salama AR, Liu X, Ord RA. Gingival carcinoma: retrospective analysis of 72 patients and indications for elective neck dissection. Br J Oral Maxillofac Surg. 2011; 49:182–185.
Article3. Chen YL, Kuo SW, Fang KH, Hao SP. Prognostic impact of marginal mandibulectomy in the presence of superficial bone invasion and the nononcologic outcome. Head Neck. 2011; 33:708–713.
Article4. Uribe S, Rojas LA, Rosas CF. Accuracy of imaging methods for detection of bone tissue invasion in patients with oral squamous cell carcinoma. Dentomaxillofac Radiol. 2013; 42:20120346.
Article5. Koenig LJ. Diagnostic imaging. Oral and maxillofacial. Salt Lake City: Amirsys Pub;2012. p. 2–28.6. Shatzkes DR, Meltzer DE, Lee JA, Babb JS, Sanfilippo NJ, Holliday RA. Sclerosis of the pterygoid process in untreated patients with nasopharyngeal carcinoma. Radiology. 2006; 239:181–186.
Article7. Munoz A, Ramos A, Ferrando J, Gomez B, Escudero L, Relea F, et al. Laryngeal cacinoma: sclerotic apperance of the cricoid and arytenoid cartilage-CT-pathologic correlation. Radilogy. 1993; 189:433–437.8. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011; 144:646–674.
Article9. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St. Louis: Elsevier;2014. p. 430.10. Nakayama E, Yoshiura K, Yuasa K, Kanda S, Saitoh M, Kage W, et al. A study of the association between the prognosis of carcinoma of the mandibular gingiva and the pattern of bone destruction on computed tomography. Dentomaxillofac Radiol. 2000; 29:163–169.
Article11. Jimi E, Furuta H, Matsuo K, Tominaga K, Takahashi T, Nakanishi O. The cellular and molecular mechanisms of bone invasion by oral squamous cell carcinoma. Oral Dis. 2011; 17:462–468.
Article12. Guise TA, Mundy GR. Cancer and bone. Endocr Rev. 1998; 19:18–54.
Article13. Partridge M, Kiguwa S, Luqmani Y, Langdon JD. Expression of bFGF, KGF and FGF receptors on normal oral mucosa and SCC. Eur J Cancer B Oral Oncol. 1996; 32B:76–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic problem of squamous papilloma and oral mucosa malignancy
- Squamous Cell Carcinoma of Temporal Bone: Four Case Reports
- The Dental Factors in Oral Squamous Cell Carcinoma
- Spindle Cell Carcinoma in Larynx: A case showing bone formation
- A clinical study on squamous cell carcinoma of the oral cavity ofKorean