Ann Hepatobiliary Pancreat Surg.
2017 Nov;21(4):223-227. 10.14701/ahbps.2017.21.4.223.
ALPPS in a patient with periductal infiltrating intrahepatic cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Multi Organ Transplant Center, King Fahad Specialist University Hospital, Dammam, Saudi Arabia.
- KMID: 2397803
- DOI: http://doi.org/10.14701/ahbps.2017.21.4.223
Abstract
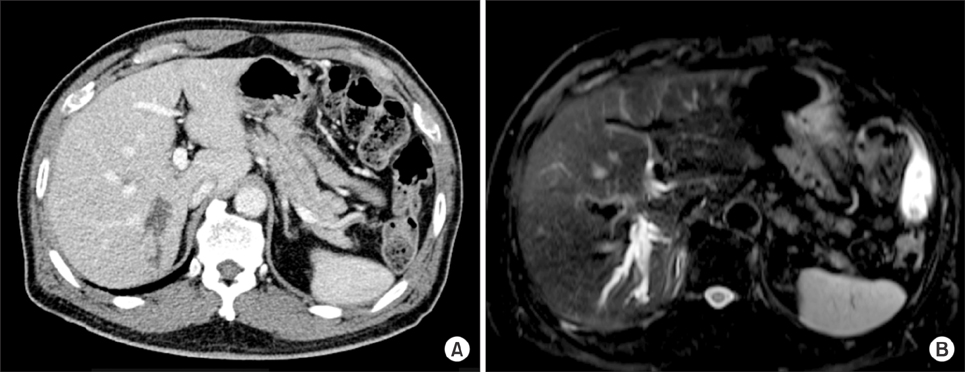
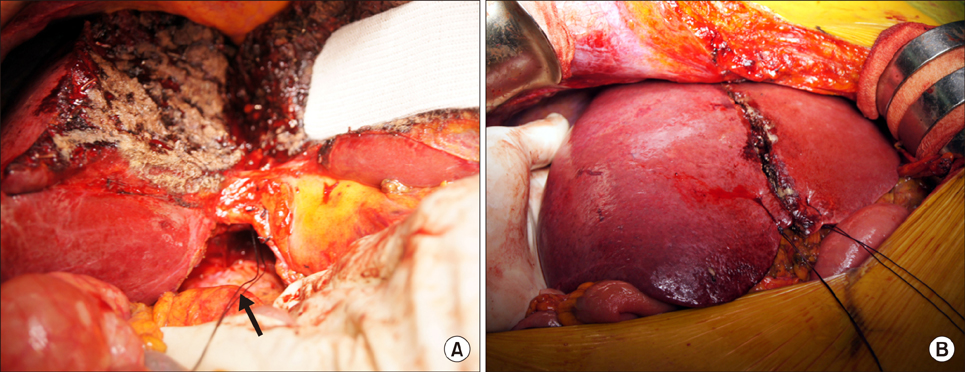
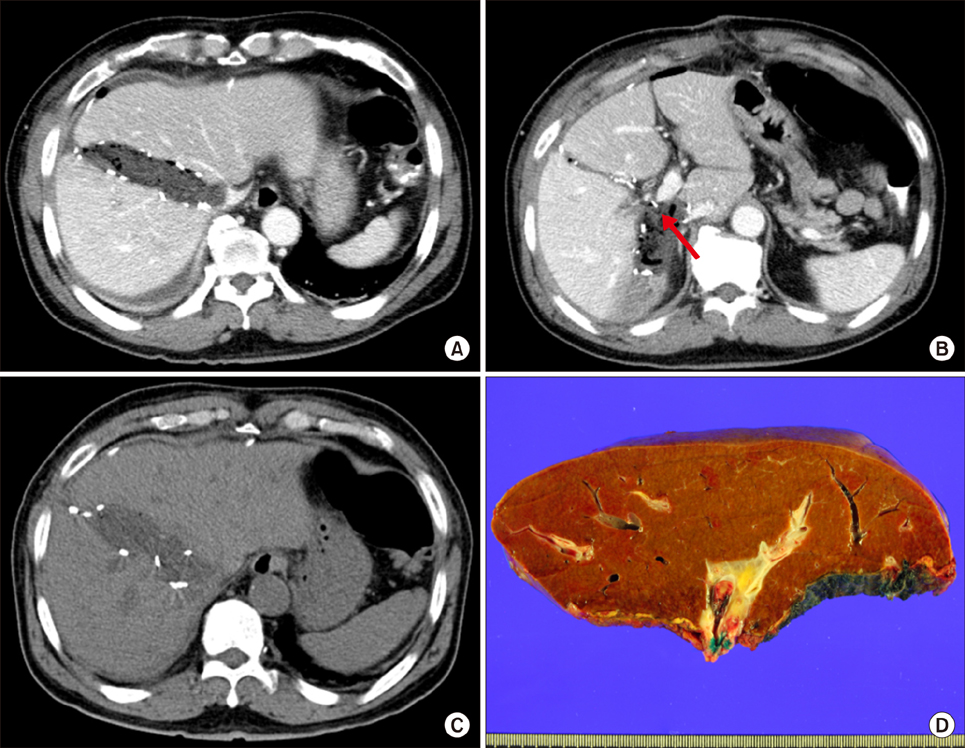
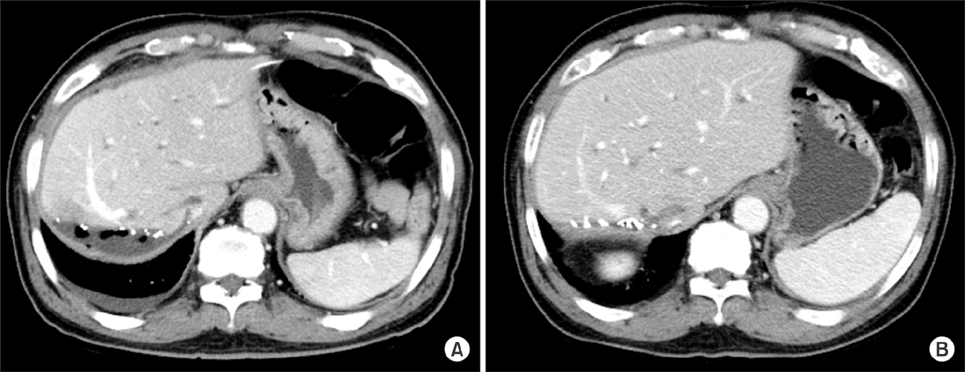
- Associating Liver Partition and Portal vein ligation for Staged hepatectomy (ALPPS) is a novel method to prevent post-hepatectomy hepatic failure. We present a case of periductal infiltrating intrahepatic cholangiocarcinoma undergone ALPPS, that was conducted as intraoperative choice instead of conducting preoperative portal vein embolization (PVE). A 65-year-old male patient was to undergo extended right posterior sectionectomy, but the operation plan was changed to conduct right hepatectomy with/without bile duct resection due to invasion of the right hepatic duct. After deciding to conduct ALPPS, we stopped further perihilar dissection and liver was transected. The right portal vein was ligated and Surgicel was densely packed between the transected hemilivers. There was rapid regeneration of the left liver on computed tomography follow-up, thus the second-stage right hepatectomy was conducted 10 days after the first-stage operation. Bile duct resection (BDR) was not performed due to heavy perihilar adhesion and inflammation, but fortunately tumor-negative bile duct resection margin was achieved after meticulous dissection. This patient recovered uneventfully and discharged nine days after the second-stage right hepatectomy. Thereafter he underwent concurrent chemoradiation therapy. He is doing well so far without evidence of tumor recurrence for 20 months after operation. In conclusion, this case suggests that ALPPS may be applied to an unexpected situation requiring PVE, but ALPPS is not recommend for treatment of perihilar malignancy requiring BDR.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Monosegment ALPPS for bilateral colorectal liver metastasis - One is enough
Klaus Steinbrück, Reinaldo Fernandes, Gustavo Stoduto, Thomas Auel
Ann Hepatobiliary Pancreat Surg. 2020;24(4):522-525. doi: 10.14701/ahbps.2020.24.4.522.
Reference
-
1. Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007; 356:1545–1559.2. Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, et al. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990; 107:521–527.3. Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P. A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg. 2004; 240:1037–1049.4. Kianmanesh R, Farges O, Abdalla EK, Sauvanet A, Ruszniewski P, Belghiti J. Right portal vein ligation: a new planned two-step all-surgical approach for complete resection of primary gastrointestinal tumors with multiple bilateral liver metastases. J Am Coll Surg. 2003; 197:164–170.5. Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012; 255:405–414.6. Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 2014; 260:829–836. discussion 836-838.7. de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg. 2012; 36:125–128.8. Lau WY, Lai EC, Lau SH. Associating liver partition and portal vein ligation for staged hepatectomy: the current role and development. Hepatobiliary Pancreat Dis Int. 2017; 16:17–26.9. Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N, et al. ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg. 2014; 38:1510–1519.10. de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg. 2012; 255:415–417.11. Olthof PB, Coelen RJS, Wiggers JK, Groot Koerkamp B, Malago M, Hernandez-Alejandro R, et al. High mortality after ALPPS for perihilar cholangiocarcinoma: case-control analysis including the first series from the international ALPPS registry. HPB (Oxford). 2017; 19:381–387.12. Lang H, de Santibanes E, Clavien PA. Outcome of ALPPS for perihilar cholangiocarcinoma: case-control analysis including the first series from the international ALPPS registry. HPB (Oxford). 2017; 19:379–380.13. Hwang S, Ha TY, Ko GY, Kwon DI, Song GW, Jung DH, et al. Preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy. World J Surg. 2015; 39:2990–2998.14. Ahn JH, Kim HD, Abuzar SM, Lee JY, Jin SE, Kim EK, et al. Intracorneal melatonin delivery using 2-hydroxypropyl-β-cyclodextrin ophthalmic solution for granular corneal dystrophy type 2. Int J Pharm. 2017; 529:608–616.15. Guiu B, Chevallier P, Denys A, Delhom E, Pierredon-Foulongne MA, Rouanet P, et al. Simultaneous trans-hepatic portal and hepatic vein embolization before major hepatectomy: the liver venous deprivation technique. Eur Radiol. 2016; 26:4259–4267.16. am Esch JS, Schmelzle M, Fürst G, Robson SC, Krieg A, Duhme C, et al. Infusion of CD133+ bone marrow-derived stem cells after selective portal vein embolization enhances functional hepatic reserves after extended right hepatectomy: a retrospective single-center study. Ann Surg. 2012; 255:79–85.17. Ludvík J, Duras P, Třeška V, Matoušková T, Brůha J, Fichtl J, et al. Portal vein embolization with contralateral application of stem cells facilitates increase of future liver remnant volume in patients with liver metastases. Cardiovasc Intervent Radiol. 2017; 40:690–696.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features of Intrahepatic Cholangiocarcinoma according to Gross Morphology
- Intrahepatic Cholangiocarcinoma: Gross Appearance and Corresponding Pathologic and Radiologic Features
- Associated Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Registry: What Have We Learned?
- CT Findings of Intrahepatic Cholangiocarcinoma Associated with Hepatolithiasis
- Surgical Treatment for Intrahepatic Cholangiocarcinoma