Ann Surg Treat Res.
2017 Dec;93(6):305-309. 10.4174/astr.2017.93.6.305.
Laparoscopic reinforcement suture on staple-line of duodenal stump using barbed suture during laparoscopic gastrectomy for gastric cancer
- Affiliations
-
- 1Department of Surgery, Dong-A University College of Medicine, Busan, Korea. mckim@donga.ac.kr
- 2Department of Surgery, Dongnam Institute of Radiological and Medical Sciences, Cancer Center, Busan, Korea.
- KMID: 2396871
- DOI: http://doi.org/10.4174/astr.2017.93.6.305
Abstract
- PURPOSE
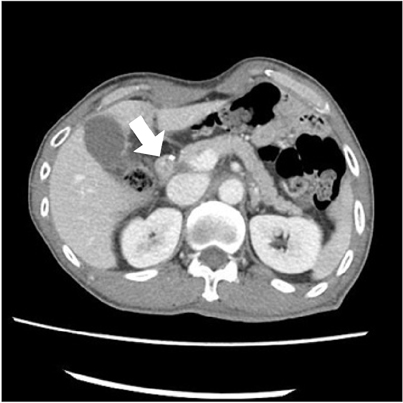
Duodenal stump fistula (DSF) is a serious complication after gastrectomy for gastric cancer. Although risk evaluation and management of DSF were presented by some investigators, there was no technical attempt has been made to prevent DSF during laparoscopic gastrectomy until now.
METHODS
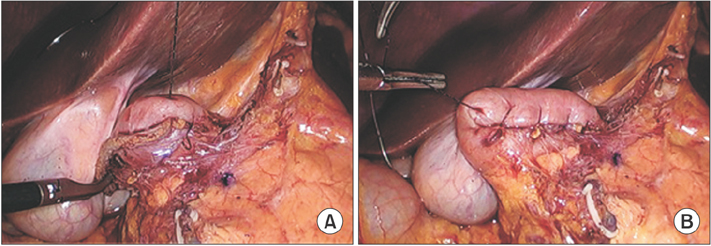
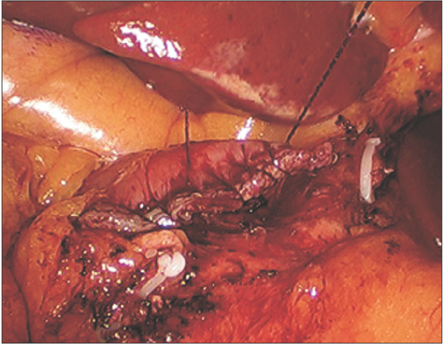
Consecutive 99 patients were enrolled from April 2014 to February 2016 in 2 institutes. All patients were performed laparoscopic gastrectomy for gastric cancer. After cutting of duodenal stump, laparoscopic reinforcement suture (LARS) commenced with continuous invagination method or interrupted method by barbed suture. Clinicopathologic features and postoperative outcomes were analyzed.
RESULTS
Fifty-six patients had comorbidity including 5 patients with duodenal ulcer. Most patients were performed distal gastrectomy with B-II, and 10 patients total gastrectomy with Roux en Y esophagojejunostomy. Although there were 2 esophagojejunostomy leakage and 1 artificial lesser curvature leakage, DSF did not occurred at all in this study. Mean operation time was 3 hours and mean LARS procedure time was 8 minutes.
CONCLUSION
LARS of duodenal stump can be considered as one of prevention methods of DSF during laparoscopic gastrectomy for gastric cancer. So this new technique will be necessary to appropriately evaluate by prospective randomized controlled trial in the future.
Keyword
MeSH Terms
Figure
Reference
-
1. Cozzaglio L, Giovenzana M, Biffi R, Cobianchi L, Coniglio A, Framarini M, et al. Surgical management of duodenal stump fistula after elective gastrectomy for malignancy: an Italian retrospective multicenter study. Gastric Cancer. 2016; 19:273–279.2. Paik HJ, Lee SH, Choi CI, Kim DH, Jeon TY, Kim DH, et al. Duodenal stump fistula after gastrectomy for gastric cancer: risk factors, prevention, and management. Ann Surg Treat Res. 2016; 90:157–163.3. Cornejo Mde L, Priego P, Ramos D, Coll M, Ballestero A, Galindo J, et al. Duodenal fistula after gastrectomy: retrospective study of 13 new cases. Rev Esp Enferm Dig. 2016; 108:20–26.4. Aurello P, Sirimarco D, Magistri P, Petrucciani N, Berardi G, Amato S, et al. Management of duodenal stump fistula after gastrectomy for gastric cancer: systematic review. World J Gastroenterol. 2015; 21:7571–7576.5. Orsenigo E, Bissolati M, Socci C, Chiari D, Muffatti F, Nifosi J, et al. Duodenal stump fistula after gastric surgery for malignancies: a retrospective analysis of risk factors in a single centre experience. Gastric Cancer. 2014; 17:733–744.6. Kim KH, Kim MC, Jung GJ. Risk factors for duodenal stump leakage after gastrectomy for gastric cancer and management technique of stump leakage. Hepatogastroenterology. 2014; 61:1446–1453.7. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Longterm results of laparoscopic gastrectomy for gastric cancer: a largescale casecontrol and case-matched Korean multicenter study. J Clin Oncol. 2014; 32:627–633.8. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010; 251:417–420.9. Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased Morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: shortterm outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016; 263:28–35.10. Etoh T, Inomata M, Shiraishi N, Kitano S. Minimally invasive approaches for gastric cancerJapanese experiences. J Surg Oncol. 2013; 107:282–288.11. Lu W, Gao J, Yang J, Zhang Y, Lv W, Mu J, et al. Longterm clinical outcomes of laparoscopyassisted distal gastrectomy versus open distal gastrectomy for early gastric cancer: a comprehensive systematic review and meta-analysis of randomized control trials. Medicine (Baltimore). 2016; 95:e3986.12. Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a largescale korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700.13. Kim MC, Choi HJ, Jung GJ, Kim HH. Techniques and complications of laparoscopyassisted distal gastrectomy (LADG) for gastric cancer. Eur J Surg Oncol. 2007; 33:700–705.14. Yakoub D, Athanasiou T, Tekkis P, Hanna GB. Laparoscopic assisted distal gastrectomy for early gastric cancer: is it an alternative to the open approach? Surg Oncol. 2009; 18:322–333.15. Chen K, Wu D, Pan Y, Cai JQ, Yan JF, Chen DW, et al. Totally laparoscopic gastrectomy using intracorporeally stapler or handsewn anastomosis for gastric cancer: a singlecenter experience of 478 consecutive cases and outcomes. World J Surg Oncol. 2016; 14:115.16. Kim EY, Choi HJ, Cho JB, Lee J. Totally laparoscopic total gastrectomy versus laparoscopically assisted total gastrectomy for gastric cancer. Anticancer Res. 2016; 36:1999–2003.17. Han G, Park JY, Kim YJ. Comparison of shortterm postoperative outcomes in totally laparoscopic distal gastrectomy versus laparoscopy-assisted distal gastrectomy. J Gastric Cancer. 2014; 14:105–110.18. Carandina S, Tabbara M, Bossi M, Valenti A, Polliand C, Genser L, et al. Staple line reinforcement during laparoscopic sleeve gastrectomy: absorbable monofilament, barbed suture, fibrin glue, or nothing? Results of a prospective randomized study. J Gastrointest Surg. 2016; 20:361–366.19. Gagner M, Buchwald JN. Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis. 2014; 10:713–723.20. Al Hajj GN, Haddad J. Prevent ing staple-line leak in sleeve gastrectomy: reinforcement with bovine pericardium vs. oversewing. Obes Surg. 2013; 23:1915–1921.21. Rogula T, Khorgami Z, Bazan M, Mamolea C, Acquafresca P, ElShazly O, et al. Comparison of reinforcement techniques using suture on staple-line in sleeve gastrectomy. Obes Surg. 2015; 25:2219–2224.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Reinforcement Suture (LARS) on Staple Line of Duodenal Stump Using Barbed Suture in Laparoscopic Gastrectomy for Gastric Cancer: a Prospective Single Arm Phase II Study
- Postoperative mechanical small bowel obstruction induced by V-Loc barbed absorbable suture after laparoscopic distal gastrectomy
- Laparoscopic Billroth-II Gastrectomy for Benign Gastric Disease
- Recurrent Gastric Cancer at the Duodenal Stump after Billroth II Subtotal Gastrectomy
- Totally Laparoscopic Distal Gastrectomy with ROUX-EN-Y Reconstruction for Treatment of Duodenal Ulcer Obstruction