J Gastric Cancer.
2017 Dec;17(4):354-362. 10.5230/jgc.2017.17.e40.
Laparoscopic Reinforcement Suture (LARS) on Staple Line of Duodenal Stump Using Barbed Suture in Laparoscopic Gastrectomy for Gastric Cancer: a Prospective Single Arm Phase II Study
- Affiliations
-
- 1Department of Surgery, Dong-A University College of Medicine, Busan, Korea. d002045@dau.ac.kr
- KMID: 2398801
- DOI: http://doi.org/10.5230/jgc.2017.17.e40
Abstract
- PURPOSE
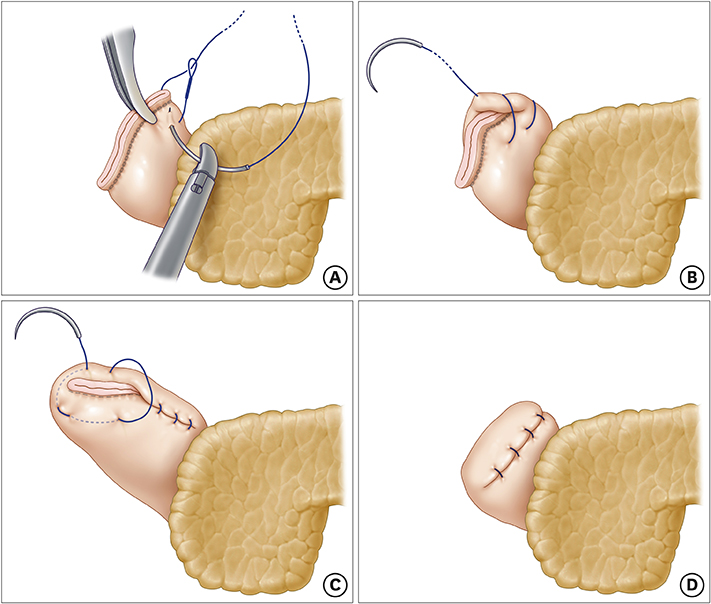
Laparoscopic gastrectomy is accepted as a standard treatment for patients with early gastric cancer in Korea, Japan, and China. However, duodenal stump leakage remains a fatal complication after gastrectomy. We conducted a prospective phase II study to evaluate the safety of the new technique of laparoscopic reinforcement suture (LARS) on the duodenal stump.
MATERIALS AND METHODS
The estimated number of patients required for this study was 100 for a period of 18 months. Inclusion criteria were histologically proven gastric adenocarcinoma treated with laparoscopic distal or total gastrectomy and Billroth II or Roux-en-Y reconstruction. The primary endpoint was the incidence of duodenal stump leakage within the first 30 postoperative days. The secondary endpoints were early postoperative outcomes until discharge.
RESULTS
One hundred patients were enrolled between February 2016 and March 2017. The study groups consisted of 65 male and 35 female patients with a mean age (years) of 62.3. Of these, 63 (63%) patients had comorbidities. The mean number of retrieved lymph nodes was 38. The mean operation time was 145 minutes including 7.8 minutes of mean LARS time. There was no occurrence of duodenal stump leakage. Thirteen complications occurred, with one case of reoperation for splenic artery rupture and one case of mortality.
CONCLUSIONS
Based on the results of this prospective phase II study, LARS can be safely performed in a short operation period without development of duodenal stump leakage. A future randomized prospective controlled trial is required to confirm the surgical benefit of LARS compared to non-LARS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors for Duodenal Stump Leakage after Laparoscopic Gastrectomy for Gastric Cancer
Lihu Gu, Kang Zhang, Zefeng Shen, Xianfa Wang, Hepan Zhu, Junhai Pan, Xin Zhong, Parikshit Asutosh Khadaroo, Ping Chen
J Gastric Cancer. 2020;20(1):81-94. doi: 10.5230/jgc.2020.20.e4.
Reference
-
1. Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016; 263:28–35.2. Hiki N, Katai H, Mizusawa J, Nakamura K, Nakamori M, Yoshikawa T, et al. Long-term outcomes of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG0703). [In print]. Gastric Cancer. 2017; DOI: 10.1007/s10120-016-0687-0.3. Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, et al. Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol. 2016; 34:1350–1357.4. Hur H, Lee HY, Lee HJ, Kim MC, Hyung WJ, Park YK, et al. Efficacy of laparoscopic subtotal gastrectomy with D2 lymphadenectomy for locally advanced gastric cancer: the protocol of the KLASS-02 multicenter randomized controlled clinical trial. BMC Cancer. 2015; 15:355.5. Park JY, Kim YW, Ryu KW, Nam BH, Lee YJ, Jeong SH, et al. Assessment of laparoscopic stomach preserving surgery with sentinel basin dissection versus standard gastrectomy with lymphadenectomy in early gastric cancer-a multicenter randomized phase III clinical trial (SENORITA trial) protocol. BMC Cancer. 2016; 16:340.6. Kim KH, Kim SH, Kim MC. How much progress has been made in minimally invasive surgery for gastric cancer in Korea?: a viewpoint from Korean prospective clinical trials. Medicine (Baltimore). 2014; 93:e233.7. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008; 49:409–415.8. Aurello P, Sirimarco D, Magistri P, Petrucciani N, Berardi G, Amato S, et al. Management of duodenal stump fistula after gastrectomy for gastric cancer: systematic review. World J Gastroenterol. 2015; 21:7571–7576.9. Cozzaglio L, Giovenzana M, Biffi R, Cobianchi L, Coniglio A, Framarini M, et al. Surgical management of duodenal stump fistula after elective gastrectomy for malignancy: an Italian retrospective multicenter study. Gastric Cancer. 2016; 19:273–279.10. Kim MC. Laparoscopic reinforcement suture of duodenal stump using barbed suture during laparoscopic gastrectomy for gastric cancer: preliminary results in consecutive 62 patients. Ann Laparosc Endosc Surg. 2017; 2:28.11. Kim KH, Kim MC, Jung GJ. Risk factors for duodenal stump leakage after gastrectomy for gastric cancer and management technique of stump leakage. Hepatogastroenterology. 2014; 61:1446–1453.12. Kim MC, Choi HJ, Jung GJ, Kim HH. Techniques and complications of laparoscopy-assisted distal gastrectomy (LADG) for gastric cancer. Eur J Surg Oncol. 2007; 33:700–705.13. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994; 4:146–148.14. Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale Korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700.15. Song KY, Hyung WJ, Kim HH, Han SU, Cho GS, Ryu SW, et al. Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol. 2008; 98:6–10.16. Cho GS, Kim W, Kim HH, Ryu SW, Kim MC, Ryu SY. Multicentre study of the safety of laparoscopic subtotal gastrectomy for gastric cancer in the elderly. Br J Surg. 2009; 96:1437–1442.17. Lee HJ, Kim HH, Kim MC, Ryu SY, Kim W, Song KY, et al. The impact of a high body mass index on laparoscopy assisted gastrectomy for gastric cancer. Surg Endosc. 2009; 23:2473–2479.18. Song J, Lee HJ, Cho GS, Han SU, Kim MC, Ryu SW, et al. Recurrence following laparoscopy-assisted gastrectomy for gastric cancer: a multicenter retrospective analysis of 1,417 patients. Ann Surg Oncol. 2010; 17:1777–1786.19. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014; 32:627–633.20. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010; 251:417–420.21. Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999; 340:908–914.22. Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, et al. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Br J Cancer. 1999; 79:1522–1530.23. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007; 245:68–72.24. Pugliese R, Maggioni D, Sansonna F, Scandroglio I, Ferrari GC, Di Lernia S, et al. Total and subtotal laparoscopic gastrectomy for adenocarcinoma. Surg Endosc. 2007; 21:21–27.25. Strong VE, Devaud N, Allen PJ, Gonen M, Brennan MF, Coit D. Laparoscopic versus open subtotal gastrectomy for adenocarcinoma: a case-control study. Ann Surg Oncol. 2009; 16:1507–1513.26. Allieta R, Nardi M Jr, Brachet-Contul R, Millo P, Fabozzi M, Cornaglia S, et al. Laparoscopic gastrectomy for treatment of advanced gastric cancer: preliminary experience on 38 cases. Minerva Chir. 2009; 64:445–456.27. Gagner M, Buchwald JN. Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis. 2014; 10:713–723.28. Ali BI, Park CH, Song KY. Outcomes of non-operative treatment for duodenal stump leakage after gastrectomy in patients with gastric cancer. J Gastric Cancer. 2016; 16:28–33.29. Kim KH, Lee HB, Kim SH, Kim MC, Jung GJ. Role of percutaneous transhepatic biliary drainage in patients with complications after gastrectomy. Int Surg. 2015; 101:78–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic reinforcement suture on staple-line of duodenal stump using barbed suture during laparoscopic gastrectomy for gastric cancer
- Postoperative mechanical small bowel obstruction induced by V-Loc barbed absorbable suture after laparoscopic distal gastrectomy
- Recurrent Gastric Cancer at the Duodenal Stump after Billroth II Subtotal Gastrectomy
- Laparoscopic Billroth-II Gastrectomy for Benign Gastric Disease
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case