J Korean Soc Radiol.
2017 Dec;77(6):353-366. 10.3348/jksr.2017.77.6.353.
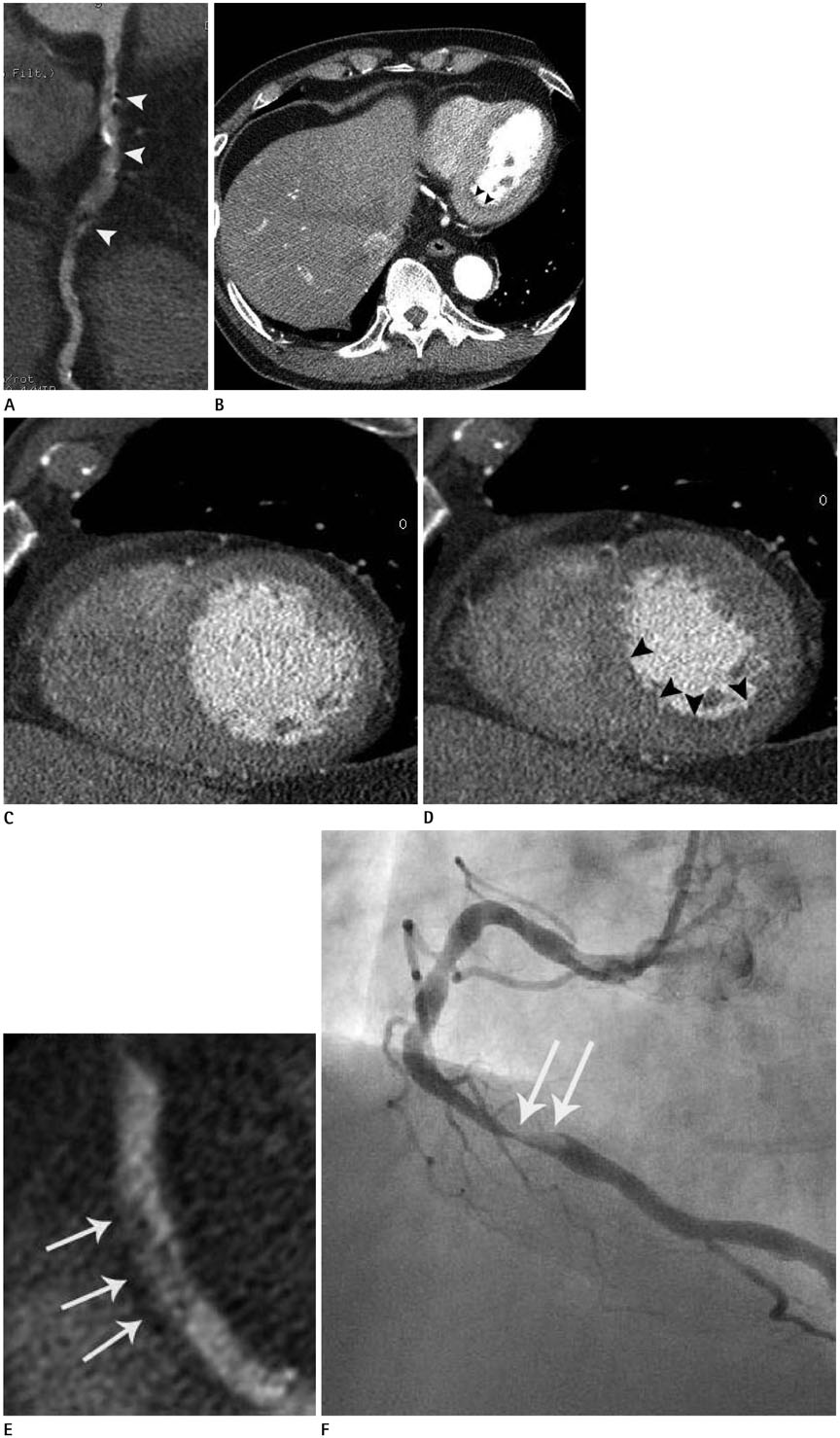
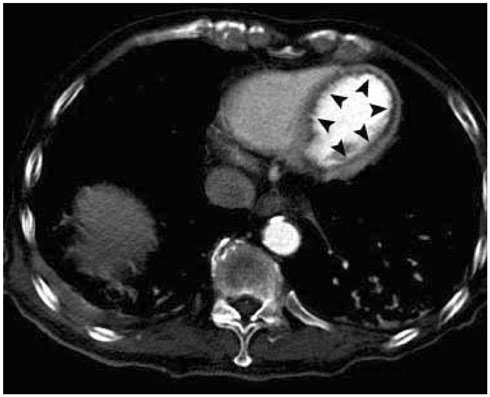
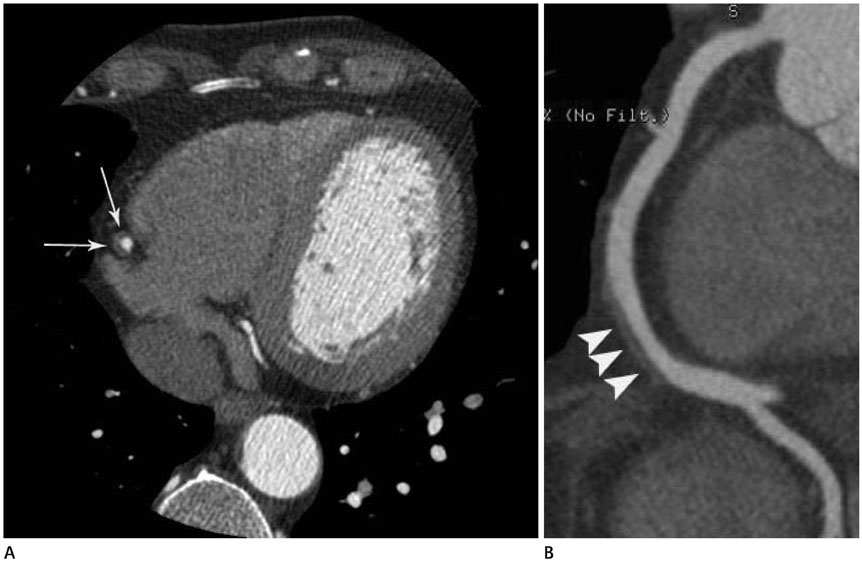
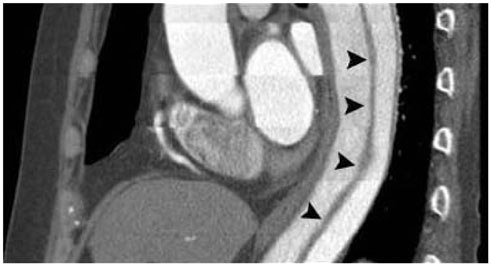
The Expanding Role of Computed Tomography Angiography in the Evaluation of Atherosclerotic Coronary Artery Disease
- Affiliations
-
- 1Department of Radiology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 2Smile Radiologic Clinic, Seoul, Korea.
- 3Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 6Department of Radiology, University of Maryland School of Medicine, Baltimore, MD, USA. cwhite@umm.edu
- KMID: 2396493
- DOI: http://doi.org/10.3348/jksr.2017.77.6.353
Abstract
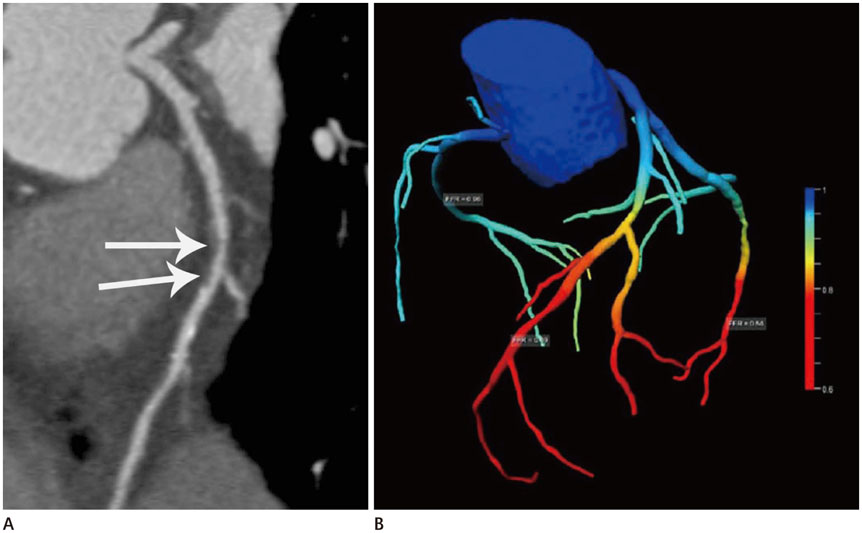
- Atherosclerotic coronary artery disease (CAD) is a leading cause of morbidity and mortality globally. Because of its remarkable technological advances, a coronary computed tomography angiography (CTA) is now a crucial imaging tool in the evaluation of patients with nonspecific acute and stable chest pain. This review article provides an overview of atherosclerotic CAD, the pros and cons of CTAs as compared to competing imaging modalities, and the potential remedies to overcome drawbacks of CTAs.
MeSH Terms
Figure
Reference
-
1. Lee J. Coronary artery calcium scoring and its impact on the clinical practice in the era of multidetector CT. Int J Cardiovasc Imaging. 2011; 27:Suppl 1. 9–25.2. Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007; 49:1860–1870.3. Hoffmann U, Brady TJ, Muller J. Cardiology patient page. Use of new imaging techniques to screen for coronary artery disease. Circulation. 2003; 108:e50–e53.4. Lee HY, Song IS, Yoo SM, Rho JY, Moon JY, White CS. Can the extent of epicardial adipose tissue thickness or the presence of descending thoracic aortic calcification predict significant coronary artery stenosis in patients with a zero coronary calcium score on multi-detector CT? Atherosclerosis. 2010; 212:495–500.5. Budoff MJ, Gul KM. Expert review on coronary calcium. Vasc Health Risk Manag. 2008; 4:315–324.6. American College of Cardiology Foundation Appropriate Use Criteria Task Force. Society of Cardiovascular Computed Tomography. American College of Radiology. American Heart Association. American Society of Echocardiography. American Society of Nuclear Cardiology. North American Society for Cardiovascular Imaging. Society for Cardiovascular Angiography and Interventions. Society for Cardiovascular Magnetic Resonance. Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010; 56:1864–1894.7. Wong ND, Budoff MJ, Pio J, Detrano RC. Coronary calcium and cardiovascular event risk: evaluation by age- and sex-specific quartiles. Am Heart J. 2002; 143:456–459.8. Yoo SM, Lee HY, White CS. Screening coronary CT angiography: possibilities and pitfalls. Int J Cardiovasc Imaging. 2014; 30:1599–1601.9. Korean Society of Radiology. Korean Society of Cardiology. Kim YJ, Yong HS, Kim SM, Kim JA, Yang DH, Hong YJ. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015; 16:251–285.10. Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013; 368:2004–2013.11. Wake R, Iida H, Ogata H, Takeshita H, Kusuyama T, Kohno H, et al. Cardiac computed tomography for the diagnosis of coronary artery atherosclerosis. Int J Clin Med. 2013; 4:183–189.12. Chang HJ, Chung N. Clinical perspective of coronary computed tomographic angiography in diagnosis of coronary artery disease. Circ J. 2011; 75:246–252.13. Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol. 2011; 57:1237–1247.14. Kim HR, Yoo SM, Rho JY, Lee HY, White CS. MDCT evaluation of atherosclerotic coronary artery disease: what should radiologists know? Int J Cardiovasc Imaging. 2014; 30:Suppl 1. 1–11.15. Yoo SM, Chun EJ, Lee HY, Min D, White CS. Computed tomography diagnosis of nonspecific acute chest pain in the emergency department: from typical acute coronary syndrome to various unusual mimics. J Thorac Imaging. 2017; 32:26–35.16. Staniak HL, Bittencourt MS, Pickett C, Cahill M, Kassop D, Slim A, et al. Coronary CT angiography for acute chest pain in the emergency department. J Cardiovasc Comput Tomogr. 2014; 8:359–367.17. Chandarana H, Srichai MB. Evaluation of myocardial abnormalities and ischemia. Radiol Clin North Am. 2010; 48:771–782.18. Seneviratne SK, Truong QA, Bamberg F, Rogers IS, Shapiro MD, Schlett CL, et al. Incremental diagnostic value of regional left ventricular function over coronary assessment by cardiac computed tomography for the detection of acute coronary syndrome in patients with acute chest pain: from the ROMICAT trial. Circ Cardiovasc Imaging. 2010; 3:375–383.19. Motoyama S, Kondo T, Sarai M, Sugiura A, Harigaya H, Sato T, et al. Multislice computed tomographic characteristics of coronary lesions in acute coronary syndromes. J Am Coll Cardiol. 2007; 50:319–326.20. Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009; 54:49–57.21. Otsuka K, Fukuda S, Tanaka A, Nakanishi K, Taguchi H, Yoshikawa J, et al. Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome. JACC Cardiovasc Imaging. 2013; 6:448–457.22. Maurovich-Horvat P, Schlett CL, Alkadhi H, Nakano M, Otsuka F, Stolzmann P, et al. The napkin-ring sign indicates advanced atherosclerotic lesions in coronary CT angiography. JACC Cardiovasc Imaging. 2012; 5:1243–1252.23. Hwang IC, Jeon JY, Kim Y, Kim HM, Yoon YE, Lee SP, et al. Statin therapy is associated with lower all-cause mortality in patients with non-obstructive coronary artery disease. Atherosclerosis. 2015; 239:335–342.24. Hecht HS. A paradigm shift: coronary computed tomographic angiography before stress testing. Am J Cardiol. 2009; 104:613–618.25. Lee HY, Yoo SM, White CS. Coronary CT angiography in emergency department patients with acute chest pain: triple rule-out protocol versus dedicated coronary CT angiography. Int J Cardiovasc Imaging. 2009; 25:319–326.26. Yoo SM, Rho JY, Lee HY, Song IS, Moon JY, White CS. Current concepts in cardiac CT angiography for patients with acute chest pain. Korean Circ J. 2010; 40:543–549.27. Yoo SM, Lee HY, White CS. MDCT evaluation of acute aortic syndrome. Radiol Clin North Am. 2010; 48:67–83.28. Lee HY, Song IS, Yoo SM, Rho JY, Moon JY, Kim IJ, et al. Rarity of isolated pulmonary embolism and acute aortic syndrome occurring outside of the field of view of dedicated coronary CT angiography. Acta Radiol. 2011; 52:378–384.29. Meijs MF, Meijboom WB, Prokop M, Mollet NR, van Mieghem CA, Doevendans PA, et al. Is there a role for CT coronary angiography in patients with symptomatic angina? Effect of coronary calcium score on identification of stenosis. Int J Cardiovasc Imaging. 2009; 25:847–854.30. Techasith T, Cury RC. Stress myocardial CT perfusion: an update and future perspective. JACC Cardiovasc Imaging. 2011; 4:905–916.31. Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol. 2014; 63:1145–1155.32. Pijls NH, Tanaka N, Fearon WF. Functional assessment of coronary stenoses: can we live without it. Eur Heart J. 2013; 34:1335–1344.33. COURAGE Trial Research Group. Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007; 356:1503–1516.34. FAME Study Investigators. Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van't Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.35. FAME 2 Trial Investigators. De Bruyne B, Fearon WF, Pijls NH, Barbato E, Tonino P, Piroth Z, et al. Fractional flow reserveguided PCI for stable coronary artery disease. N Engl J Med. 2014; 371:1208–1217.36. King SB 3rd. Is it form or function?: the “COURAGE” to ask. JACC Cardiovasc Interv. 2014; 7:202–220.37. American College of Cardiology Foundation. American Heart Association Task Force on Practice Guidelines. American College of Physicians. American Association for Thoracic Surgery. Preventive Cardiovascular Nurses Association. Society for Cardiovascular Angiography and Interventions. Society of Thoracic Surgeons. Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012; 60:e44–e164.38. Yunaga H, Ohta Y, Kaetsu Y, Kitao S, Watanabe T, Furuse Y, et al. Diagnostic performance of calcification-suppressed coronary CT angiography using rapid kilovolt-switching dual-energy CT. Eur Radiol. 2017; 27:2794–2801.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Atherosclerotic Plaque in Non-invasive Coronary Imaging
- Evaluation of Myocardial Ischemia Using Coronary Computed Tomography Angiography in Patients with Stable Angina
- CT Imaging Findings in Non-Atherosclerotic Coronary Artery Disease
- Assessment of Coronary Stenosis Using Coronary CT Angiography in Patients with High Calcium Scores: Current Limitations and Future Perspectives
- Coronary CT Angiography