J Korean Fract Soc.
2011 Jul;24(3):230-236.
Anatomically Percutaneous Wiring Reduction in Minimally Invasive Plate Osteosynthesis for Distal Tibial Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. -chan-@hanmail.net
Abstract
- PURPOSE
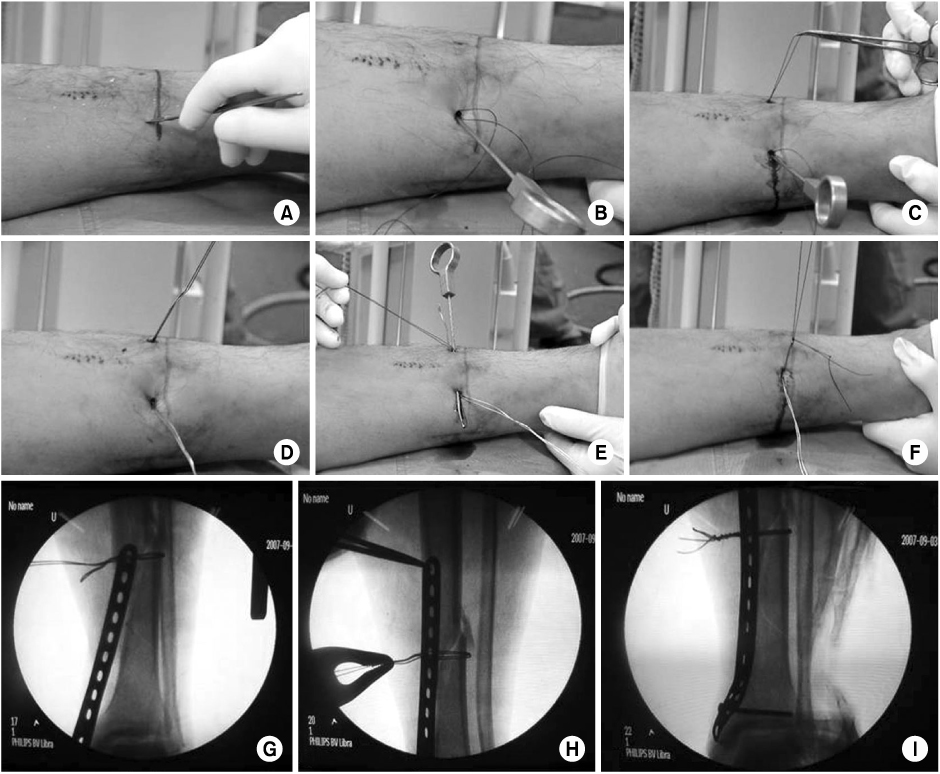
To report the method of anatomical reduction and its maintenance by percutaneous wiring reduction in minimally invasive plate osteosynthesis for distal tibial fractures.
MATERIALS AND METHODS
17 cases that were diagnosed oblique, spiral or transverse fracture of distal tibia from August 2007 to February 2010 and were able to anatomically reduce by the method of percutanous wiring reduction in minimally invasive plate osteosynthesis were included in this study. Mean age was 50, and mean follow up period was 18 months. We investigated the period until bone union was achieved, degree of angulation angle, and complications. For postoperative evaluation, Olerud and Molander ankle score and VAS pain score in daily living were checked.
RESULTS
The mean varus/valgus angulation after bone union on AP radiograph was 0.9 degrees and the mean anterior/posterior angulation on lateral radiograph was 2.0 degrees The mean Olerud and Molander ankle score was 89.4, and mean pain score due to walk adjacent to metal plate was 0 points.
CONCLUSION
By the method of percutaneous wiring reduction in distal tibial fracture, anatomical reduction is easily acquired, and only by wire itself, reduction could be maintained, so that without additional manual reduction, plate could be easily fixed.
Figure
Reference
-
1. Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999. 13:92–97.
Article2. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury. 1998. 29:3 Suppl. C3–C6.
Article3. Bolhofner BR, Carmen B, Clifford P. The results of open reduction and internal fixation of distal femur fractures using a biological (indirect) reduction technique. J Orthop Trauma. 1996. 10:372–377.
Article4. Borg T, Larsson S, Lindsjö U. Minimally-invasive plating of distal tibia fractures. Preliminary results in 21 patients. Injury. 2004. 35:608–614.5. Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002. 16:691–695.
Article6. Bradley GW, Mckenna GB, Dunn HK, Daniels AU, Statton WO. Effects of flexural rigidity of plates on bone healing. J Bone Joint Surg Am. 1979. 61:866–872.
Article7. Brumback RJ, McGarvey WC. Fractures of the tibial plafond. Evolving treatment concepts for the pilon fracture. Orthop Clin North Am. 1995. 26:273–285.8. Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010. 24:24–29.
Article9. Ghera S, Santori FS, Calderaro M, Giorgini TL. Minimally invasive plate osteosynthesis in distal tibial fractures: pitfalls and surgical guidelines. Orthopedics. 2004. 27:903–905.
Article10. Hahn D, Bradbury N, Hartley R, Radford PJ. Intramedullary nail breakage in distal fractures of the tibia. Injury. 1996. 27:323–327.
Article11. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007. 38:365–370.
Article12. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997. 28:1 Suppl. A42–A47.
Article13. Holbrook JL, Swiontkowski MF, Sanders R. Treatment of open fractures of the tibial shaft: ender nailing versus external fixation. A randomized, prospective comparison. J Bone Joint Surg Am. 1989. 71:1231–1238.14. Kim YM, Shin HD, Yang JY, Yang JH, Lee HJ, Kim KC. Percutaneous temporal wiring method for minimally invasive plate osteosynthesis of a distal tibial fracture. Orthopedics. 2009. 32:177.15. Kim YM, Yang JH, Kim DK. Minimally invasive percutaneous plate osteosynthesis using periarticular plate for distal tibial fractures. J Korean Fract Soc. 2007. 20:315–322.
Article16. Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005. 125:87–94.
Article17. Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these ankles function over time? J Bone Joint Surg Am. 2003. 85:287–295.18. McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992. 6:195–200.
Article19. Mckibbin B. The biology of fracture healing in long bones. J Bone Joint Surg Br. 1978. 60:150–162.
Article20. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003. 408:286–291.
Article21. Olerud C, Molander H. A scoring scale for symptoms evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984. 103:190–194.22. Pai V, Coulter G, Pai V. Minimally invasive plate fixation of the tibia. Int Orthop. 2007. 31:491–496.
Article23. Puno RM, Teynor JT, Nagano J, Gustilo RB. Critical analysis of result of 201 tibial shaft fractures. Clin Orthop Relat Res. 1986. 212:113–121.24. Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br. 1995. 77:781–787.
Article25. Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979. 138:105–110.
Article26. Shon OJ, Kim DS. Minimally invasive percutaneous plate osteosynthesis using a lateral plate in distal tibial fracture. J Korean Fract Soc. 2010. 23:42–49.
Article27. Toms AD, McMurtie A, Maffulli N. Percutaneous plating of the distal tibia. J Foot Ankle Surg. 2004. 43:199–203.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Minimally Invasive Percutaneous Plate Osteosynthesis Using a Lateral Plate in Distal Tibial Fracture
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures
- Minimally Invasive Plate Osteosynthesis for Periarticular Tibial Fractures
- Bone Union Time of Simple Distal Femur Fractures in the Elderly according to Fracture Gap after Treated with Minimally Invasive Plate Osteosynthesis