J Korean Ophthalmol Soc.
2017 Nov;58(11):1301-1306. 10.3341/jkos.2017.58.11.1301.
An Unusual Case of Endogenous Klebsiella Pneumonia Endophthalmitis
- Affiliations
-
- 1Department of Ophthalmology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. Kimdk89@empas.com
- KMID: 2395874
- DOI: http://doi.org/10.3341/jkos.2017.58.11.1301
Abstract
- PURPOSE
To report an unusual case of endogenous endophthalmitis in a patient with Klebsiella pneumoniae primary liver abscess.
CASE SUMMARY
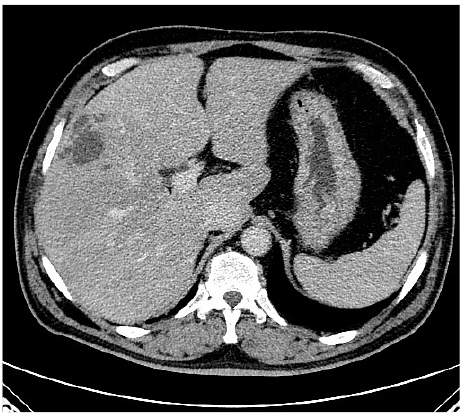
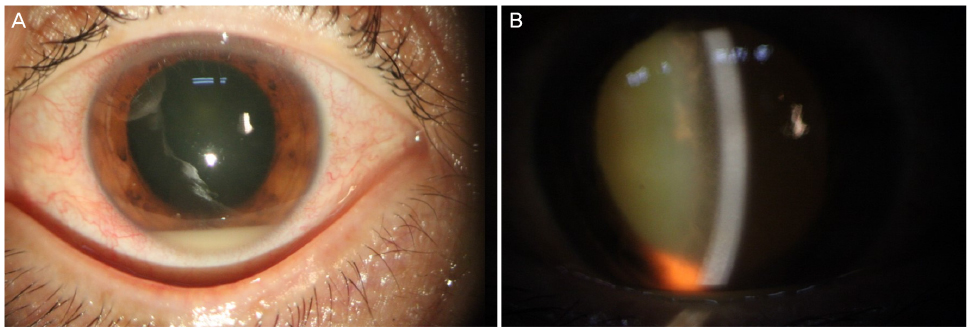
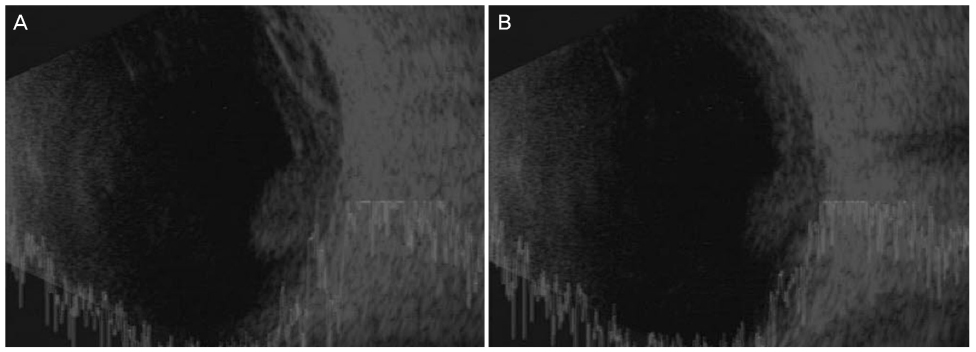
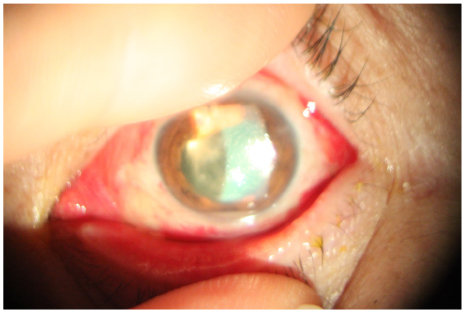
A-54-year-old man with diabetes mellitus and liver abscess was referred to us for consultation of visual loss in his left eye for 2 days. On the first examination, the patient's left visual acuity was hand motion and the left intraocular pressure was 13 mmHg. Vitreous opacity and inflammatory membrane were detected with increased echogenicity using ultrasonography. Vitectomy and intravitreous antibiotic injection were performed under the impression of endogenous endophthalmitis caused by liver abscess on the day of the first visit. Culture revealed Klebsiella pneumoniae from blood and liver abscess. After vitrectomy, the patient showed improvement. However, on the 20th and 40th postoperative days, the patient complained of blurred vision, and inflammation and hypopyon were observed in the anterior chamber. An intracameral antibiotic injection and anterior chamber washing were performed. The patient has not complained of any other symptoms to date.
CONCLUSIONS
In this patient with endophthalmitis, inflammation and hypopyon in the anterior chamber were evident three times after vitrectomy. Ultimately, the inflammation was effectively controlled by intracameral antibiotic injection and anterior chamber washes.
MeSH Terms
Figure
Reference
-
1. Okada AA, Johnson RP, Liles WC, et al. Endogenous bacterial endophthalmitis. Report of a ten-year retrospective study. Ophthalmology. 1994; 101:832–838.2. Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol. 2003; 48:403–423.3. Kim HW, Kim SY, Chung IY, et al. Emergence of Enterococcus species in the infectious microorganisms cultured from patients with endophthalmitis in South Korea. Infection. 2014; 42:113–118.4. Han JM, Kim NJ. Two Cases of bilateral endogenous Klebsiella pneumoniae endophthalmitis in primary Klebsiella pneumoniae liver abscess patients. J Korean Ophthalmol Soc. 2009; 50:1590–1594.5. Chang FY, Chou MY. Comparison of pyogenic liver abscesses caused by Klebsiella pneumoniae and non-K. pneumoniae pathogens. J Formos Med Assoc. 1995; 94:232–237.6. Sng CC, Jap A, Chan YH, Chee SP. Risk factors for endogenous Klebsiella endophthalmitis in patients with Klebsiella bacteraemia: a case-control study. Br J Ophthalmol. 2008; 92:673–677.7. Sheu SJ, Kung YH, Wu TT, et al. Risk factors for endogenous endophthalmitis secondary to klebsiella pneumoniae liver abscess: 20-year experience in Southern Taiwan. Retina. 2011; 31:2026–2031.8. Lee SS, Chen YS, Tsai HC, et al. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 2008; 47:642–650.9. La TY, Kim CW, Lee JS. A case of endogenous endophthalmitis accompanying orbital cellulitis caused by klebsiella pneumoniae from liver abscess. J Korean Ophthalmol Soc. 2000; 41:1000–1005.10. Tae KS, Kim TH, Moon YS, Chin HS. A case of Klebsiella endogenous endophthalmitis accompanied by necrotizing scleral perforation. J Korean Ophthalmol Soc. 2003; 44:2680–2686.11. Lee YH, Choi SJ, Kim IC, Chung YT. A case of the bilateral metastatic endophthalmitis. J Korean Ophthalmol Soc. 1995; 36:2048–2053.12. Shim HS, Lee SS, Park JM, Song JK. Three cases of the metastatic endophthalmitis. J Korean Ophthalmol Soc. 1994; 35:349–355.13. Byun YC, Lee H, Lee EK, Lee KW. A case of metastatic endophthalmitis originated from bacterial endocardits. J Korean Ophthalmol Soc. 1994; 35:122–127.14. Yang CS, Tsai HY, Sung CS, et al. Endogenous Klebsiella endophthalmitis associated with pyogenic liver abscess. Ophthalmology. 2007; 114:876–880.15. Yoon YH, Lee SU, Sohn JH, Lee SE. Result of early vitrectomy for endogenous Klebsiella pneumoniae endophthalmitis. Retina. 2003; 23:366–370.16. Ang M, Jap A, Chee SP. Prognostic factors and outcomes in endogenous Klebsiella pneumoniae endophthalmitis. Am J Ophthalmol. 2011; 151:338–344.e2.17. Suh DS, Roh JH, Kim SD. Surgical management of infectious endophthalmitis: Early vitrectomy vs late vitrectomy. J Korean Ophthalmol Soc. 1998; 39:2418–2425.18. Zhang YQ, Wang WJ. Treatment outcomes after pars plana vitrectomy for endogenous endophthalmitis. Retina. 2005; 25:746–750.19. Doft BH, Kelsey SF, Wisniewski S, et al. Treatment of endophthalmitis after cataract extraction. Retina. 1994; 14:297–304.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of the Bilateral Metastatic Endophthalmitis
- Klebsiella pneumoniae Brain Abscess and Endophthalmitis after Acute Epiglottitis
- Two Cases of Endogenous Endophthalmitis
- A Case of Endogenous endophthalmitis Caused by Klebsiella Pneumoniae from Emphysematous Pyelonephritis
- A Case of Endogenous Endophthalmitis Accompanying Orbital Cellulitis Caused by Klebsiella Pneumoniae from Liver Abscess