Ann Dermatol.
2017 Apr;29(2):143-148. 10.5021/ad.2017.29.2.143.
Urticarial Dermatitis: Clinical Characteristics of Itch and Therapeutic Response to Cyclosporine
- Affiliations
-
- 1Department of Dermatology, Pusan National University School of Medicine, Busan, Korea. dockbs@pusan.ac.kr
- 2Depeartment of Nursing Science, Choonhae College of Health Sciences, Ulsan, Korea.
- 3Bio-Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2394836
- DOI: http://doi.org/10.5021/ad.2017.29.2.143
Abstract
- BACKGROUND
Urticarial dermatitis, which is characterised by persistent wheals with eczematous papules and plaques, is frequently misdiagnosed and difficult to treat. Patients commonly experience intolerable pruritus which may greatly affect their quality of life.
OBJECTIVE
The objective of this study is to characterize the clinical patterns of pruritus in patients with urticarial dermatitis and to determine the effectiveness of cyclosporine treatment.
METHODS
This prospective study included 50 histopathologically confirmed patients with urticarial dermatitis. A face-to-face structured questionnaire was given to all patients, and they were treated with low-dose cyclosporine (1~3 mg/kg/d) for at least 2 weeks.
RESULTS
The majority of patients (80.0%) had moderate to severe pruritus. Most patients experienced exacerbation of the itch in the evening (74.0%), with the extremities (upper, 86.0%; lower, 94.0%) being the most commonly involved sites. Due to severe pruritus, patients complained about reduced social contact, quality of life and difficulties in falling asleep et al. Cyclosporine significantly reduced the mean itch score and extent of erythema, and improved interference with daily activities and sleep.
CONCLUSION
Our study highlights the detailed description and characteristics of pruritus in patients with urticarial dermatitis. And we recommend alternative and effective therapeutic option of low-dose cyclosporine.
Keyword
MeSH Terms
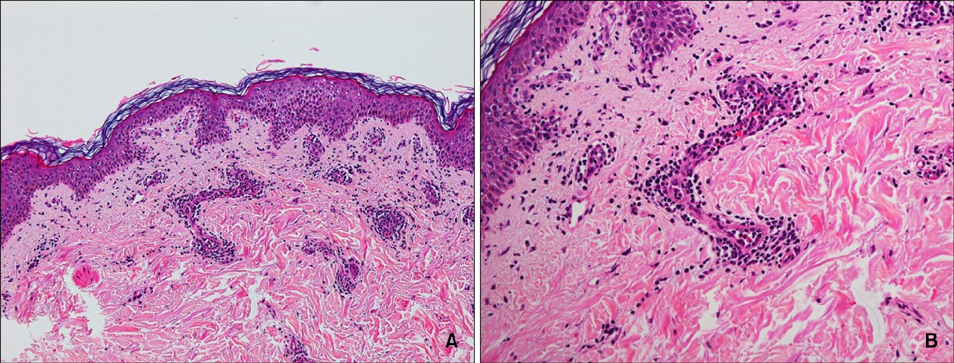
Figure
Reference
-
1. Hannon GR, Wetter DA, Gibson LE. Urticarial dermatitis: clinical features, diagnostic evaluation, and etiologic associations in a series of 146 patients at Mayo Clinic (2006~2012). J Am Acad Dermatol. 2014; 70:263–268.
Article2. Kossard S, Hamann I, Wilkinson B. Defining urticarial dermatitis: a subset of dermal hypersensitivity reaction pattern. Arch Dermatol. 2006; 142:29–34.3. Lee JS, Loh TH, Seow SC, Tan SH. Prolonged urticaria with purpura: the spectrum of clinical and histopathologic features in a prospective series of 22 patients exhibiting the clinical features of urticarial vasculitis. J Am Acad Dermatol. 2007; 56:994–1005.
Article4. Peroni A, Colato C, Zanoni G, Girolomoni G. Urticarial lesions: if not urticaria, what else? The differential diagnosis of urticaria: part II. Systemic diseases. J Am Acad Dermatol. 2010; 62:557–570.
Article5. Kazmierowski JA, Chusid MJ, Parrillo JE, Fauci AS, Wolff SM. Dermatologic manifestations of the hypereosinophilic syndrome. Arch Dermatol. 1978; 114:531–535.
Article6. Erturk IE, Arican O, Omurlu IK, Sut N. Effect of the pruritus on the quality of life: a preliminary study. Ann Dermatol. 2012; 24:406–412.
Article7. Patel T, Ishiuji Y, Yosipovitch G. Nocturnal itch: why do we itch at night? Acta Derm Venereol. 2007; 87:295–298.
Article8. Haest C, Casaer MP, Daems A, De Vos B, Vermeersch E, Morren MA, et al. Measurement of itching: validation of the Leuven Itch Scale. Burns. 2011; 37:939–950.
Article9. Chaptini C, Sidhu S. Mycophenolate mofetil as a treatment for urticarial dermatitis. Australas J Dermatol. 2014; 55:275–278.
Article10. Asero R. Oral cyclophosphamide in a case of cyclosporin and steroid-resistant chronic urticaria showing autoreactivity on autologous serum skin testing. Clin Exp Dermatol. 2005; 30:582–583.
Article11. Tedeschi A, Airaghi L, Lorini M, Asero R. Chronic urticaria: a role for newer immunomodulatory drugs? Am J Clin Dermatol. 2003; 4:297–305.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Itch in atopic dermatitis: from pathogenesis to treatment
- Clinical Character istics of Itch in Patients with Adult and Childhood Atopic Dermatitis
- A Clinical Study of Urticarial Dermatitis
- Clinical Study of Itch in Korean Patients with Chronic Idiopathic Urticaria
- Systemic Treatment of Cyclosporin in Severe Atopic Dermatitis