J Korean Acad Prosthodont.
2017 Oct;55(4):389-393. 10.4047/jkap.2017.55.4.389.
Flexibility of resin splint systems for traumatized teeth
- Affiliations
-
- 1Institute for Clinical Dental Research, Korea University Medical Center, Korea University, Seoul, Korea. wddc@korea.ac.kr
- KMID: 2393910
- DOI: http://doi.org/10.4047/jkap.2017.55.4.389
Abstract
- PURPOSE
The aim of this study is to evaluate the flexural strength of flexible resins and the flexibility of different resin splint (RS) systems in comparison with resin wire splint (RWS) system.
MATERIALS AND METHODS
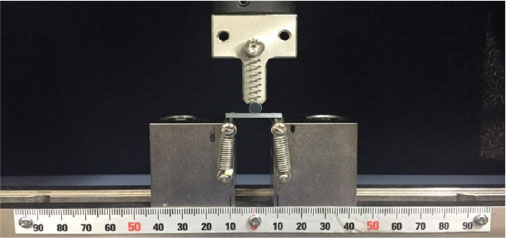
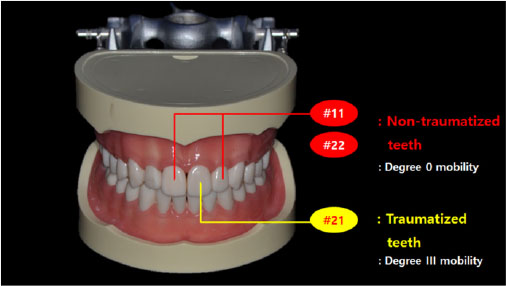
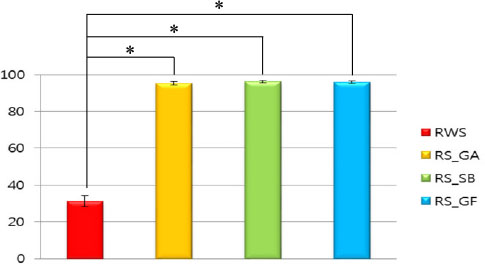
Three different resin materials (G-aenial flo, GA, GC; Superbond, SB, Sun medical; G-fix, GF, GC) were tested flexural strength test in accordance with ISO-4049:2000. For the flexibility test of splint systems, a artificial model with resin teeth was used to evaluate three types of resin splint systems (GA, SB, and GF) and one resin wire splint system. The left central incisor was simulated "˜injured teeth' with third degree mobility. Three consecutively repeated measurements of periotest value were taken in horizontal direction, before and after splinting to access tooth mobility. The splinting effect was calculated through the periotest value. Differences were evaluated through One-way Anova and Tukey HDS post-hoc tests for pair-wise comparison (α= .05).
RESULTS
Although GA group showed significant higher flexural strength than SB and GF groups, all of three different resin splint systems produced a significantly higher and rigid splinting effect compared with 016" resin-wire splint system (P < .05).
CONCLUSION
Within the limits of an in vitro study, it can be stated that resin splint systems are too rigid and may not be acceptable to treat tooth avulsion.
Keyword
MeSH Terms
Figure
Reference
-
1. Andreasen JO, Andreasen FM. Textbook and colour atlas of traumatic injuries to the teeth. 3rd ed. Copenhagen: Munksgaard;1994. p. 155. p. 383. p. 425. .2. Soares AJ, Gomes BP, Zaia AA, Ferraz CC, de Souza-Filho FJ. Relationship between clinical-radiographic evaluation and outcome of teeth replantation. Dent Traumatol. 2008; 24:183–188.
Article3. Gutmann JL, Gutmann MS. Cause, incidence, and prevention of trauma to teeth. Dent Clin North Am. 1995; 39:1–13.
Article4. Glendor U, Halling A, Andersson L, Eilert-Petersson E. Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed Dent J. 1996; 20:15–28.5. Ram D, Cohenca N. Therapeutic protocols for avulsed permanent teeth: review and clinicalupdate. Pediatr Dent. 2004; 26:251–255.6. Kwan SC, Johnson JD, Cohenca N. The effect of splint material and thickness on tooth mobility afterextraction and replantation using a human cadaveric model. Dent Traumatol. 2012; 28:277–281.
Article7. Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, Diangelis AJ, Kenny DJ, Sigurdsson A, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Tsukiboshi M. International association of dental traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2012; 28:88–96.
Article8. Ram D, Cohenca N. Therapeutic protocols for avulsed permanent teeth: review and clinicalupdate. Pediatr Dent. 2004; 26:251–255.9. Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root of treatmentfactors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol. 2004; 20:203–211.
Article10. Frost HM. A determinant of bone architecture. The minimum effective strain. Clin Orthop Relat Res. 1983; (175):286–292.11. Frost HM. Skeletal structural adaptations to mechanical usage (SATMU):1. Redefining Wolff's law: the bone modeling problem. Anat Rec. 1990; 226:403–413.
Article12. Yasuda T, Kinoshita M, Abe M, Shibayama Y. Unfavorable effect of knee immobilization on Achilles tendon healing in rabbits. Acta Orthop Scand. 2000; 71:69–73.
Article13. Vailas AC, Tipton CM, Matthes RD, Gart M. Physical activity and its influence on the repair process of medialcollateral ligaments. Connect Tissue Res. 1981; 9:25–31.
Article14. Becker H, Diegelmann RF. The influence of tension in intrinsic tendon fibroplasia. Orthop Rev. 1984; 13:65–71.15. American Association of Endodontists Guideline. Recommended guidelines of the AAE for the treatment of traumatic dental injuries. revised 2013. Available from: http://www.nxtbook.com/nxtbooks/aae/traumaguidelines/index.php.16. Mazzoleni S, Meschia G, Cortesi R, Bressan E, Tomasi C, Ferro R, Stellini E. In vitro comparison of the flexibility of different splint systems used in dental traumatology. Dent Traumatol. 2010; 26:30–36.
Article17. Andresen M, Mackie I, Worthington H. The Periotest in traumatology. Part I. Does it have the properties necessary for use as a clinical device and can the measurements be interpreted? Dent Traumatol. 2003; 19:214–217.
Article18. Berthold C, Auer FJ, Potapov S, Petschelt A. In vitro splint rigidity evaluation-comparison of a dynamic and a static measuring method. Dent Traumatol. 2011; 27:414–421.
Article19. Berthold C, Holst S, Schmitt J, Goellner M, Petschelt A. An evaluation of the Periotest method as a tool for monitoring toothmobility in dental traumatology. Dent Traumatol. 2010; 26:120–128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COMPARISON OF WEAR RESISTANCE AMONG RESIN DENTURE TEETH OPPOSING VARIOUS RESTORATIVE MATERIALS
- THE SHEAR BOND STRENGTH OF RESIN TEETH TO THE DENTURE BASE RESIN
- Changes of bite force and occlusal contacts after stabilization splint therapy
- Morphological Assessment of Proximal Restoration Depending on Different Matrix Systems in Primary Molars with a 3D Scanner: In Vitro Studies
- Evaluation of polymerization ability of resin-based materials used for teeth splinting