J Korean Assoc Oral Maxillofac Surg.
2017 Oct;43(5):331-335. 10.5125/jkaoms.2017.43.5.331.
Protrusive maxillomandibular fixation for intracapsular condylar fracture: a report of two cases
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery and Dental Research Institute, College of Dentistry, Wonkwang University, Iksan, Korea. cejoms@wku.ac.kr
- KMID: 2393599
- DOI: http://doi.org/10.5125/jkaoms.2017.43.5.331
Abstract
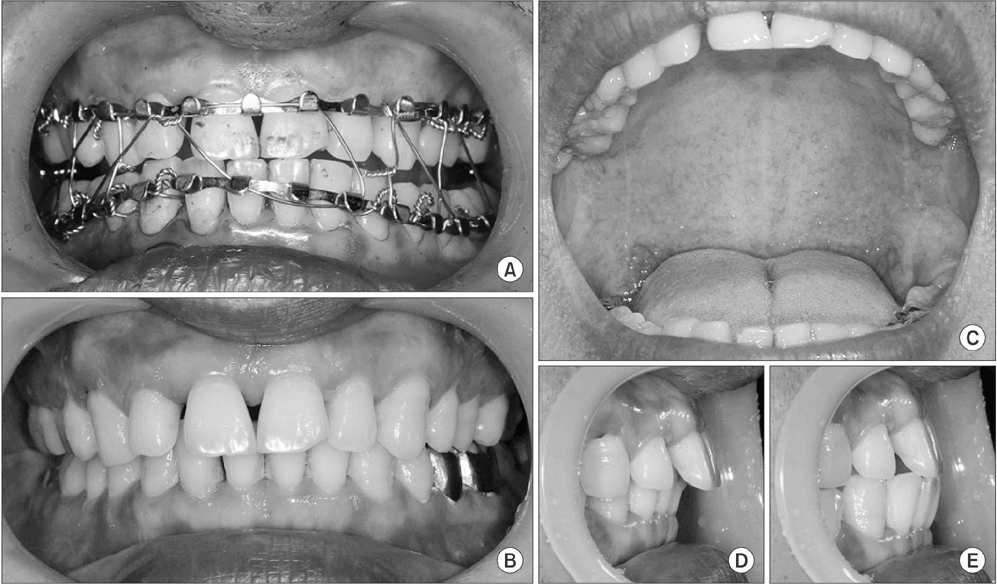
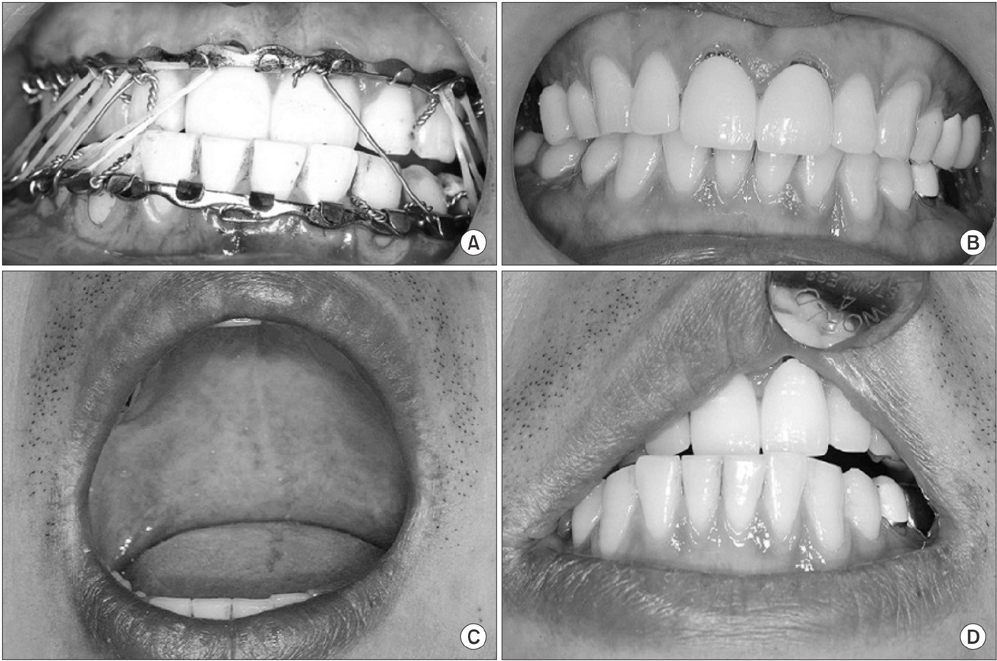
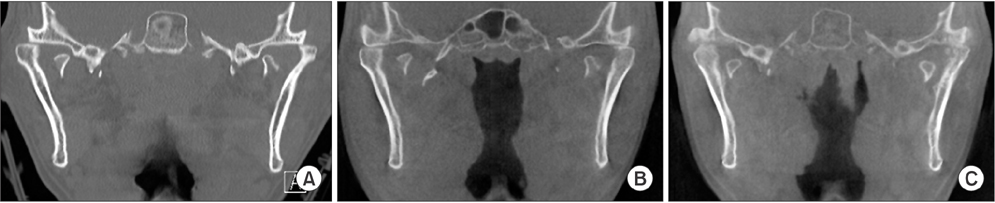
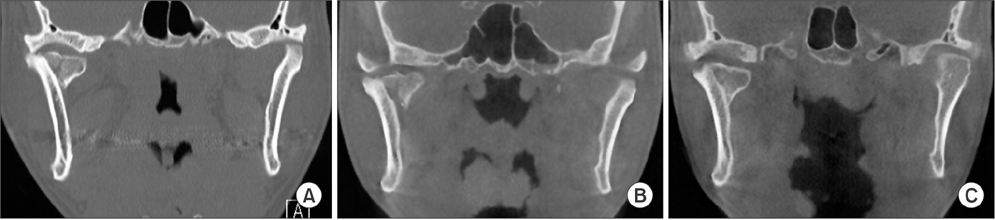
- Clinical limitations following closed reduction of an intracapsular condylar fracture include a decrease in maximum mouth opening, reduced range of mandibular movements such as protrusion/lateral excursion, and reduced occlusal stability. Anteromedial and inferior displacement of the medial condyle fragment by traction of the lateral pterygoid muscle can induce bone overgrowth due to distraction osteogenesis between the medial and lateral condylar fragments, causing structural changes in the condyle. In addition, when conventional maxillomandibular fixation (MMF) is performed, persistent interdental contact sustains masticatory muscle hyperactivity, leading to a decreased vertical dimension and premature contact of the posterior teeth. To resolve the functional problems of conventional closed reduction, we designed a novel method for closed reduction through protrusive MMF for two weeks. Two patients diagnosed with intracapsular condylar fracture had favorable occlusion after protrusive MMF without premature contact of the posterior teeth. This particular method has two main advantages. First, in the protrusive position, the lateral condylar fragment is moved in the anterior-inferior direction closer to the medial fragment, minimizing bone formation between the two fragments and preventing structural changes. Second, in the protrusive position, posterior disclusion occurs, preventing masticatory muscle hyperactivity and the subsequent gradual decrease in ramus height.
MeSH Terms
Figure
Reference
-
1. Kermer Ch, Undt G, Rasse M. Surgical reduction and fixation of intracapsular condylar fractures. A follow up study. Int J Oral Maxillofac Surg. 1998; 27:191–194.2. Hlawitschka M, Loukota R, Eckelt U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int J Oral Maxillofac Surg. 2005; 34:597–604.
Article3. Miloro M, Ghali GE, Larsen PE, Waite P. Peterson's principles of oral and maxillofacial surgery. 3rd ed. Shelton: PMPH-USA;2012. p. 445–446.4. Long X, Goss AN. A sheep model of intracapsular condylar fracture. J Oral Maxillofac Surg. 2007; 65:1102–1108.
Article5. Hlawitschka M, Eckelt U. Assessment of patients treated for intracapsular fractures of the mandibular condyle by closed techniques. J Oral Maxillofac Surg. 2002; 60:784–791.
Article6. Takenoshita Y, Ishibashi H, Oka M. Comparison of functional recovery after nonsurgical and surgical treatment of condylar fractures. J Oral Maxillofac Surg. 1990; 48:1191–1195.
Article7. Brandt MT, Haug RH. Open versus closed reduction of adult mandibular condyle fractures: a review of the literature regarding the evolution of current thoughts on management. J Oral Maxillofac Surg. 2003; 61:1324–1332.
Article8. Loukota RA, Eckelt U, De Bont L, Rasse M. Subclassification of fractures of the condylar process of the mandible. Br J Oral Maxillofac Surg. 2005; 43:72–73.
Article9. Walker RV. Condylar fractures: nonsurgical management. J Oral Maxillofac Surg. 1994; 52:1185–1188.
Article10. Li Z, Djae KA, Li ZB. Post-traumatic bifid condyle: the pathogenesis analysis. Dent Traumatol. 2011; 27:452–454.
Article11. Assael LA. Open versus closed reduction of adult mandibular condyle fractures: an alternative interpretation of the evidence. J Oral Maxillofac Surg. 2003; 61:1333–1339.
Article12. Liu CK, Liu P, Meng FW, Deng BL, Xue Y, Mao TQ, et al. The role of the lateral pterygoid muscle in the sagittal fracture of mandibular condyle (SFMC) healing process. Br J Oral Maxillofac Surg. 2012; 50:356–360.
Article13. Dawson PE. Functional occlusion: from TMJ to smile design. St. Louis: Mosby Elsevier;2007.14. Cascone P, Sassano P, Spallaccia F, Rivaroli A, Di Paolo C. Condylar fractures during growth: follow-up of 16 patients. J Craniofac Surg. 1999; 10:87–92.15. Alajbeg IZ, Valentic-Peruzovic M, Alajbeg I, Cifrek M. The influence of age and dental status on elevator and depressor muscle activity. J Oral Rehabil. 2006; 33:94–101.
Article16. Canter HI, Kayikcioglu A, Aksu M, Mavili ME. Botulinum toxin in closed treatment of mandibular condylar fracture. Ann Plast Surg. 2007; 58:474–478.
Article17. Williamson EH, Lundquist DO. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983; 49:816–823.
Article18. Sarmiento A, Latta LL. Functional fracture bracing. J Am Acad Orthop Surg. 1999; 7:66–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- T-Condylar Fracture of Distal Humerus in a Child: A Case Report
- Current Concepts in the Mandibular Condyle Fracture Management Part I: Overview of Condylar Fracture
- Noninvasive Functional therapy of Mandibular Condylar Fracture
- Clinical study on surgical management of mandibular condylar fractures
- Modified high-submandibular appraoch for open reduction and internal fixation of condylar fracture: case series report