J Cerebrovasc Endovasc Neurosurg.
2017 Sep;19(3):184-188. 10.7461/jcen.2017.19.3.184.
A Case of Unusual Presentation of Contrast-induced Encephalopathy after Cerebral Angiography Using Iodixanol
- Affiliations
-
- 1Department of Neurosurgery, Hallym University Sacred Heart Hospital, Anyang, Korea. sparkahn@naver.com
- 2Kangwon National University College of Medicine, Chuncheon, Korea.
- KMID: 2393500
- DOI: http://doi.org/10.7461/jcen.2017.19.3.184
Abstract
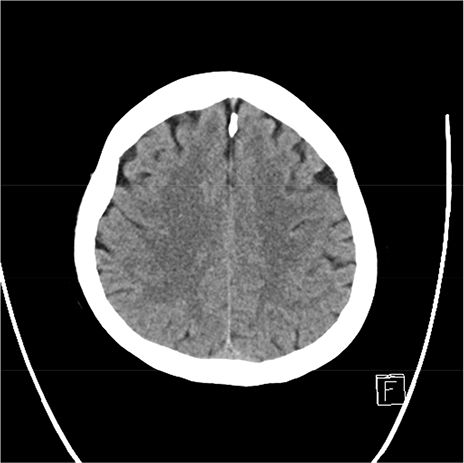
- Contrast-induced encephalopathy after cerebral angiography is a rare complication and until now, only few cases have been reported. This paper reports on contras-induced encephalopathy mimicking meningoencephalitis after cerebral angiography by using iodixanol, an iso-osmolar non-ionic contrast agent. A 58-year-old woman underwent cerebral angiography for the evaluation of multiple intracranial aneurysms. A few hours later, she had persistent headache, vomiting, fever, and seizures. Brain computed tomography (CT) showed sulcal obliteration of right cerebral hemisphere and cerebrospinal fluid profile was unremarkable. The next day, she developed left side hemiparesis, sensory loss, and left-sided neglect with drowsy mentality. Brain magnetic resonance imaging (MRI) showed cerebral swelling with leptomeningeal enhancement in the right parieto-occipital lobe without sign of ischemia or hemorrhage. The patient was managed with intravenous dexamethasone, mannitol and anticonvulsant. There was a progressive neurological improvement with complete resolution of the symptoms at day 6. This observation highlights that contrast-induced encephalopathy can be caused by an iso-osmolar non-ionic contrast agent. This rare entity should be suspected if neurologic deterioration after cerebral angiography is not explained by other frequent causes such as acute infarction or hemorrhage.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Unusual Magnetic Resonance Imaging Findings Contrast-induced Encephalopathy following Cerebral Angiography
Won Ho Cho, Jung Hwan Lee, Tae Hong Lee, Chang Hwa Choi, Jun Kyeung Ko
Kosin Med J. 2021;36(1):51-55. doi: 10.7180/kmj.2021.36.1.51.
Reference
-
1. Baik SK, Kim YS, Lee HJ, Park J, Kim GC. Immediate CT findings following embolization of cerebral aneurysms: suggestion of blood-brain barrier or vascular permeability change. Neuroradiology. 2008; 03. 50(3):259–266.
Article2. Brisman JL, Jilani M, McKinney JS. Contrast enhancement hyperdensity after endovascular coiling of intracranial aneurysms. AJNR Am J Neuroradiol. 2008; 03. 29(3):588–593.
Article3. Broman T, Olsson O. The tolerance of cerebral blood-vessels to a contrast medium of the diodrast group: An experimental study of the effect on the blood-brain-barrier. Acta Radiologica. 1948; 07. 30(4-5):326–342.
Article4. Chisci E, Setacci F, de Donato G, Setacci C. A case of contrast-induced encephalopathy using iodixanol. J Endovasc Ther. 2011; 08. 18(4):540–544.
Article5. Frontera JA, Pile-Spellman J, Mohr JP. Contrast-induced neurotoxicity and selective cortical injury. Cerebrovasc Dis. 2007; 24(1):148–151.
Article6. Guimaraens L, Vivas E, Fonnegra A, Sola T, Soler L, Balaguer E, et al. Transient encephalopathy from angiographic contrast: a rare complication in neurointerventional procedures. Cardiovasc Intervent Radiol. 2010; 04. 33(2):383–388.
Article7. Hansson HA, Johansson B, Blomstrand C. Ultrastructural studies on cerebrovascular permeability in acute hypertension. Acta Neuropathol. 1975; 08. 32(3):187–198.
Article8. Kocabay G, Karabay CY, Kalayci A, Akgun T, Guler A, Oduncu V, et al. Contrast-induced neurotoxicity after coronary angiography. Herz. 2014; 06. 39(4):522–527.
Article9. Lantos G. Cortical blindness due to osmotic disruption of the blood-brain barrier by angiographic contrast material: CT and MRI studies. Neurology. 1989; 04. 39(4):567–571.
Article10. Latchaw RE. The use of nonionic contrast agents in neuroangiography. A review of the literature and recommendations for clinical use. Invest Radiol. 1993; 11. 28:Suppl 5. S55–S59. discussion S60-1.11. Law S, Panichpisal K, Demede M, John S, Marmur JD, Nath J, et al. Contrast-Induced Neurotoxicity following Cardiac Catheterization. Case Rep Med. 2012; 2012:267860.
Article12. Leong S, Fanning NF. Persistent neurological deficit from iodinated contrast encephalopathy following intracranial aneurysm coiling. A case report and review of the literature. Interv Neuroradiol. 2012; 03. 18(1):33–41.13. Mani RL, Eisenberg RL. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. III. Assessment of arteries injected, contrast medium used, duration of procedure, and age of patient. AJR Am J Roentgenol. 1978; 11. 131(5):871–874.
Article14. Ozturk A, Saatci I, Pamuk AG, Erdogan C, Akmangit I, Geyik S, et al. Focal increased cortical density in immediate postembolization CT scans of patients with intracranial aneurysms. AJNR Am J Neuroradiol. 2006; 10. 27(9):1866–1875.15. Potsi S, Chourmouzi D, Moumtzouoglou A, Nikiforaki A, Gkouvas K, Drevelegas A. Transient contrast encephalopathy after carotid angiography mimicking diffuse subarachnoid haemorrhage. Neurol Sci. 2012; 04. 33(2):445–448.
Article16. Rapoport SI, Levitan H. Neurotoxicity of X-ray contrast media. Relation to lipid solubility and blood-brain barrier permeability. Am J Roentgenol Radium Ther Nucl Med. 1974; 09. 122(1):186–193.17. Rapoport SI, Thompson HK, Bidinger JM. Equi-osmolal opening of the blood-brain barrier in the rabbit by different contrast media. Acta Radiol Diagn (Stockh). 1974; 01. 15(1):21–32.
Article18. Saigal G, Bhatia R, Bhatia S, Wakhloo AK. MR findings of cortical blindness following cerebral angiography: is this entity related to posterior reversible leukoencephalopathy? AJNR Am J Neuroradiol. 2004; 02. 25(2):252–256.19. Shinoda J, Ajimi Y, Yamada M, Onozuka S. Cortical blindness during coil embolization of an unruptured intracranial aneurysm--case report. Neurol Med Chir (Tokyo). 2004; 08. 44(8):416–419.
Article20. Wishart DL. Complications in vertebral angiography as compared to non-vertebral cerebral angiography in 447 studies. Am J Roentgenol Radium Ther Nucl Med. 1971; 11. 113(3):527–537.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hyperintense Acute Reperfusion Marker on FLAIR in Patient with Possible Contrast-Induced Encephalopathy Following Cerebral Angiography
- Unusual Magnetic Resonance Imaging Findings Contrast-induced Encephalopathy following Cerebral Angiography
- Contrast-Induced Encephalopathy after Coil Embolization: A Case Report and Review of Literature
- Fully Reversible Contrast-Induced Encephalopathy Mimicking Stroke after Flow Diverter Treatment of Carotid Cave Aneurysm
- A case of anaphylactoid reaction to nonionic contrast agent, Iodixanol (Visipaque(R)) during coronary angiography