J Periodontal Implant Sci.
2017 Oct;47(5):312-327. 10.5051/jpis.2017.47.5.312.
Bone-level implants placed in the anterior maxilla: an open-label, single-arm observational study
- Affiliations
-
- 1Department of Stomatology, China-Japan Friendship Hospital, Beijing, China.
- 2Key Laboratory for Oral Biomedical Engineering of Ministry of Education, Wuhan University School and Hospital of Stomatology, Wuhan, China.
- 3Department of Oral and Maxillofacial Surgery, Seoul National University School of Dentistry, Seoul, Korea. leejongh@snu.ac.kr
- 4Department of Oral and Maxillofacial Surgery, Seoul National University Gwanak Dental Hospital, Seoul, Korea.
- 5Department of Oral and Maxillofacial Surgery, Clinical Trial Center, Seoul National University Dental Hospital, Seoul, Korea.
- KMID: 2392718
- DOI: http://doi.org/10.5051/jpis.2017.47.5.312
Abstract
- PURPOSE
This study assessed marginal bone remodeling and soft tissue esthetics after the loading of single bone-level implants in the anterior maxilla.
METHODS
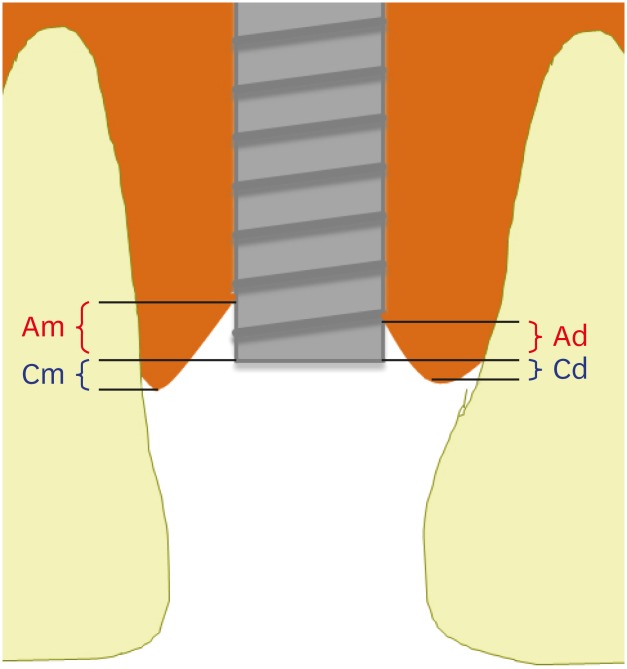
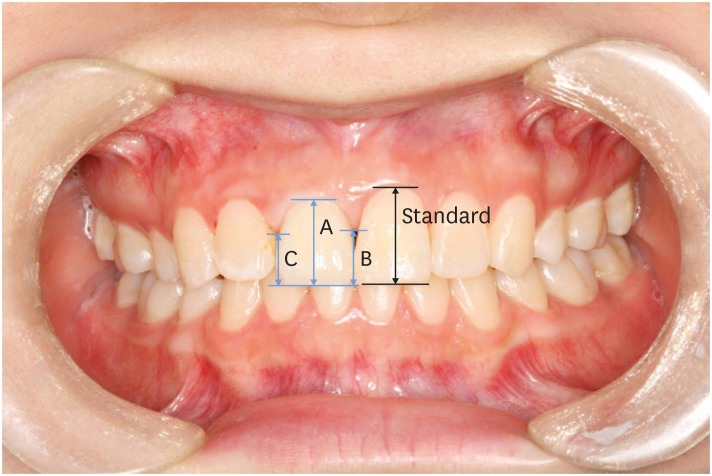
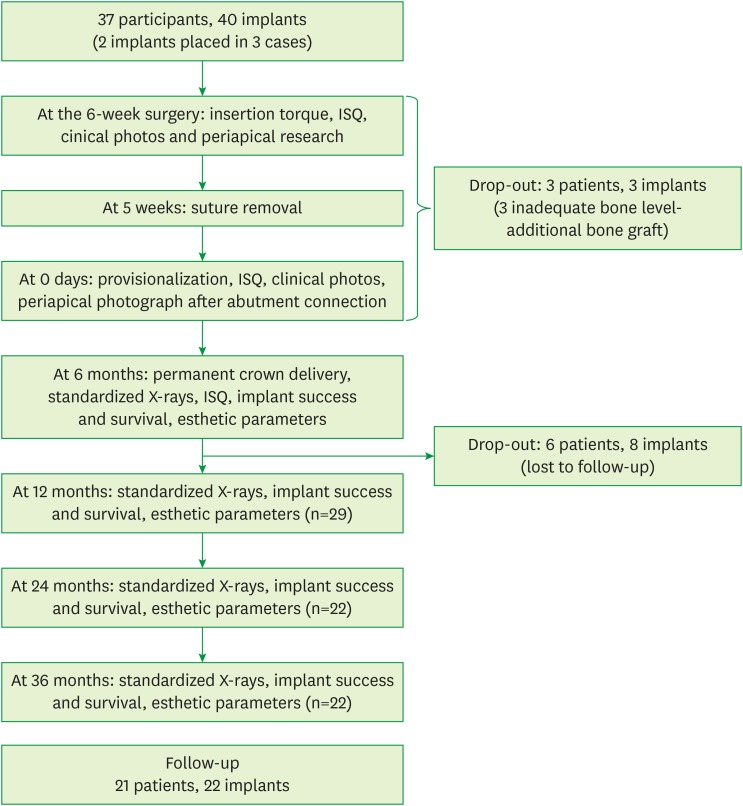
An open, single-arm observational clinical trial with 3 years of follow-up was performed, including 22 implants. The patients presented with a single tooth gap in the anterior maxilla (tooth positions 14-24), with natural or restored adjacent teeth. An implant was placed at least 8 weeks post-extraction and healed submerged for 6 weeks. After the second-stage operation, a fixed provisional prosthesis was provided. The final restoration was placed 6 months after the provisional restoration. The time of the provisional crown connection was considered to be the baseline in this study. Esthetic parameters and the marginal bone level were assessed at 6, 12, 24, and 36 months.
RESULTS
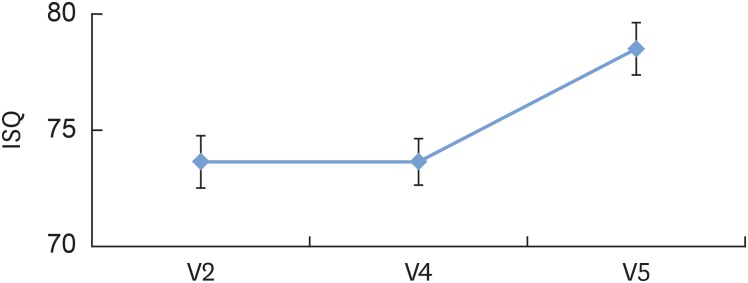
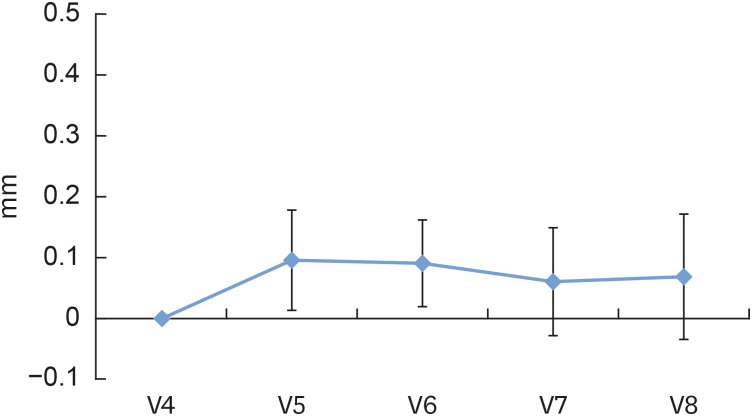
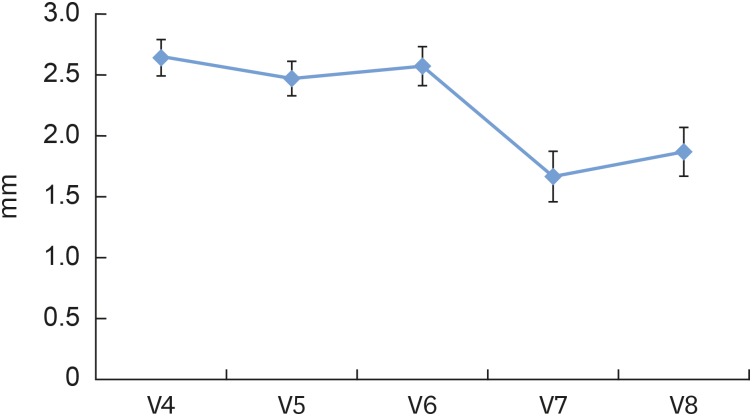
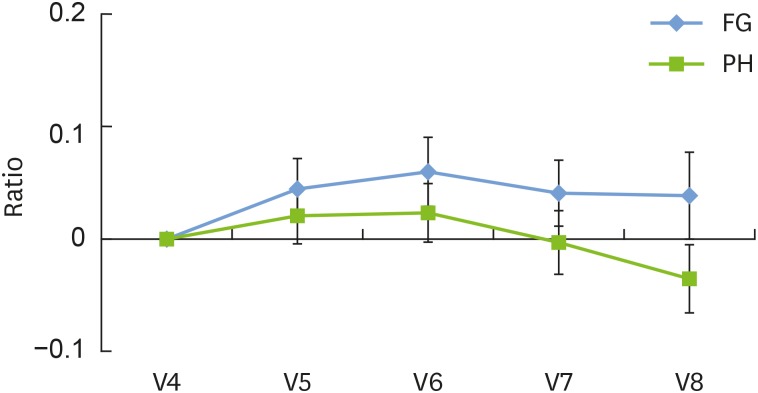
All implants were well integrated in the bone. A statistically significant increase was found in the mean implant stability quotient between the time of the provisional prosthesis and the time of the final prosthesis. Most implants (95.5%) revealed marginal bone resorption (<0.5 mm), and just 1 implant (4.5%) showed a change of 2.12 mm from baseline to 36 months (mean 0.07±0.48 mm), while the crestal bone level decreased significantly, from 2.34±0.93 mm at baseline to 1.70±1.10 mm at 36 months. The facial gingival margin and papilla were stable and the esthetic scores indicated high patient and dentist satisfaction.
CONCLUSIONS
Platform-switching bone-level implants placed in maxillary single-tooth gaps resulted in successful osseointegration with minimal marginal bone resorption. The peri-implant soft tissue was also esthetically satisfying and stable.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Bone loss-related factors in tissue and bone level dental implants: a systematic review of clinical trials
Hamed Mortazavi, Amin Khodadoustan, Aida Kheiri, Lida Kheiri
J Korean Assoc Oral Maxillofac Surg. 2021;47(3):153-174. doi: 10.5125/jkaoms.2021.47.3.153.
Reference
-
1. Belser UC, Bernard JP, Buser D. Implant-supported restorations in the anterior region: prosthetic considerations. Pract Periodontics Aesthet Dent. 1996; 8:875–883. PMID: 9242147.2. Rufenacht CR. Fundamentals of esthetics. Chicago (IL): Quintessence;1990.3. Buser D, von Arx T. Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res. 2000; 11(Suppl 1):83–100.
Article4. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25. PMID: 3527955.5. Weber HP, Buser D, Fiorellini JP, Williams RC. Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants. Clin Oral Implants Res. 1992; 3:181–188. PMID: 1298433.
Article6. Brägger U, Häfeli U, Huber B, Hämmerle CH, Lang NP. Evaluation of postsurgical crestal bone levels adjacent to non-submerged dental implants. Clin Oral Implants Res. 1998; 9:218–224. PMID: 9760896.
Article7. Pham AN, Fiorellini JP, Paquette D, Williams RC, Weber HP. Longitudinal radiographic study of crestal bone levels adjacent to non-submerged dental implants. J Oral Implantol. 1994; 20:26–34. PMID: 7932853.8. Ricci G, Aimetti M, Stablum W, Guasti A. Crestal bone resorption 5 years after implant loading: clinical and radiologic results with a 2-stage implant system. Int J Oral Maxillofac Implants. 2004; 19:597–602. PMID: 15346759.9. Hartman GA, Cochran DL. Initial implant position determines the magnitude of crestal bone remodeling. J Periodontol. 2004; 75:572–577. PMID: 15152822.
Article10. Belser UC, Buser D, Hess D, Schmid B, Bernard JP, Lang NP. Aesthetic implant restorations in partially edentulous patients--a critical appraisal. Periodontol 2000. 1998; 17:132–150. PMID: 10337321.11. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987; 2:145–151. PMID: 3507627.
Article12. Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990; 1:33–40. PMID: 2099210.13. Bornstein MM, Schmid B, Belser UC, Lussi A, Buser D. Early loading of non-submerged titanium implants with a sandblasted and acid-etched surface. 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res. 2005; 16:631–638. PMID: 16307568.14. Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009; 80:140–151. PMID: 19228100.
Article15. Jung RE, Jones AA, Higginbottom FL, Wilson TG, Schoolfield J, Buser D, et al. The influence of non-matching implant and abutment diameters on radiographic crestal bone levels in dogs. J Periodontol. 2008; 79:260–270. PMID: 18251640.
Article16. Biancu S, Ericsson I, Lindhe J. The periodontal ligament of teeth connected to osseointegrated implants. An experimental study in the beagle dog. J Clin Periodontol. 1995; 22:362–370. PMID: 7601917.
Article17. Besimo CE, Guindy JS, Lewetag D, Meyer J. Prevention of bacterial leakage into and from prefabricated screw-retained crowns on implants in vitro . Int J Oral Maxillofac Implants. 1999; 14:654–660. PMID: 10531737.18. Engquist B, Astrand P, Dahlgren S, Engquist E, Feldmann H, Gröndahl K. Marginal bone reaction to oral implants: a prospective comparative study of Astra Tech and Brånemark System implants. Clin Oral Implants Res. 2002; 13:30–37. PMID: 12005142.19. Cardaropoli G, Lekholm U, Wennström JL. Tissue alterations at implant-supported single-tooth replacements: a 1-year prospective clinical study. Clin Oral Implants Res. 2006; 17:165–171. PMID: 16584412.
Article20. Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, Cochran DL, et al. Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res. 2004; 83:529–533. PMID: 15218041.
Article21. Schwarz F, Herten M, Sager M, Wieland M, Dard M, Becker J. Bone regeneration in dehiscence-type defects at chemically modified (SLActive) and conventional SLA titanium implants: a pilot study in dogs. J Clin Periodontol. 2007; 34:78–86. PMID: 17137467.
Article22. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996; 23:971–973. PMID: 8915028.23. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006; 26:9–17. PMID: 16515092.24. Hürzeler M, Fickl S, Zuhr O, Wachtel HC. Peri-implant bone level around implants with platform-switched abutments: preliminary data from a prospective study. J Oral Maxillofac Surg. 2007; 65:33–39. PMID: 17586347.
Article25. Fickl S, Zuhr O, Stein JM, Hürzeler MB. Peri-implant bone level around implants with platform-switched abutments. Int J Oral Maxillofac Implants. 2010; 25:577–581. PMID: 20556258.26. Buser D, Chappuis V, Kuchler U, Bornstein MM, Wittneben JG, Buser R, et al. Long-term stability of early implant placement with contour augmentation. J Dent Res. 2013; 92:176S–82S. PMID: 24158332.
Article27. Buser D, Bornstein MM, Weber HP, Grütter L, Schmid B, Belser UC. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: a cross-sectional, retrospective study in 45 subjects with a 2- to 4-year follow-up. J Periodontol. 2008; 79:1773–1781. PMID: 18771381.
Article28. Buser D, Halbritter S, Hart C, Bornstein MM, Grütter L, Chappuis V, et al. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: 12-month results of a prospective study with 20 consecutive patients. J Periodontol. 2009; 80:152–162. PMID: 19228101.
Article29. Hämmerle CH, Jung RE, Sanz M, Chen S, Martin WC, Jackowski J, et al. Submerged and transmucosal healing yield the same clinical outcomes with two-piece implants in the anterior maxilla and mandible: interim 1-year results of a randomized, controlled clinical trial. Clin Oral Implants Res. 2012; 23:211–219. PMID: 21722188.
Article30. Santing HJ, Raghoebar GM, Vissink A, den Hartog L, Meijer HJ. Performance of the Straumann Bone Level Implant system for anterior single-tooth replacements in augmented and nonaugmented sites: a prospective cohort study with 60 consecutive patients. Clin Oral Implants Res. 2013; 24:941–948. PMID: 22540833.
Article31. Nisapakultorn K, Suphanantachat S, Silkosessak O, Rattanamongkolgul S. Factors affecting soft tissue level around anterior maxillary single-tooth implants. Clin Oral Implants Res. 2010; 21:662–670. PMID: 20384705.
Article32. Cairo F, Pagliaro U, Nieri M. Soft tissue management at implant sites. J Clin Periodontol. 2008; 35:163–167. PMID: 18724848.
Article33. Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001; 72:1364–1371. PMID: 11699478.
Article34. Kan JY, Rungcharassaeng K. Interimplant papilla preservation in the esthetic zone: a report of six consecutive cases. Int J Periodontics Restorative Dent. 2003; 23:249–259. PMID: 12854775.35. Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003; 74:1785–1788. PMID: 14974820.
Article36. Lops D, Chiapasco M, Rossi A, Bressan E, Romeo E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket: 1-year prospective study. Clin Oral Implants Res. 2008; 19:1135–1140. PMID: 18983316.
Article37. Kourkouta S, Dedi KD, Paquette DW, Mol A. Interproximal tissue dimensions in relation to adjacent implants in the anterior maxilla: clinical observations and patient aesthetic evaluation. Clin Oral Implants Res. 2009; 20:1375–1385. PMID: 19681967.
Article38. Sorni-Bröker M, Peñarrocha-Diago M, Peñarrocha-Diago M. Factors that influence the position of the peri-implant soft tissues: a review. Med Oral Patol Oral Cir Bucal. 2009; 14:e475–9. PMID: 19415054.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oral rehabilitation with mandibular anterior segmental osteotomy and implantation: A case report
- The Comparison between the success rates of single implants replacing the mandibular first and second molar
- A Retrospective study on the survival rate of the sinus perforated implants
- Treatment concepts for the posterior maxilla and mandible: short implants versus long implants in augmented bone
- Retrospective study on marginal bone loss around maxillary anterior implants with or without bone graft