Allergy Asthma Respir Dis.
2017 Mar;5(2):105-110. 10.4168/aard.2017.5.2.105.
Risk factors for latent tuberculosis in children who had close contact to households with pulmonary tuberculosis
- Affiliations
-
- 1Department of Pediatrics, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. jy7.shim@samsung.com
- KMID: 2392382
- DOI: http://doi.org/10.4168/aard.2017.5.2.105
Abstract
- PURPOSE
Tuberculosis (TB) is a common and possibly fatal infectious disease, and its incidence and prevalence is quite high in Korea compared to other Organization for Economic Co-operation and Development countries. Patients who have active TB can cause latent tuberculosis infection (LTBI) in children, which may progress to reactivated tuberculosis. This study was performed to analyze the risk of adult TB that affects children's LTBI.
METHODS
From June 2013 to May 2014, 60 children (32 boys, 28 girls) who came into close contact with adult patients diagnosed with pulmonary TB underwent LTBI tests. The children were divided into the 2 groups: the first group was finally diagnosed to LTBI, and the second group was proven not to have LTBI. We compared the risk of adult patients with pulmonary TB between children with LTBI and those without through a medical record review.
RESULTS
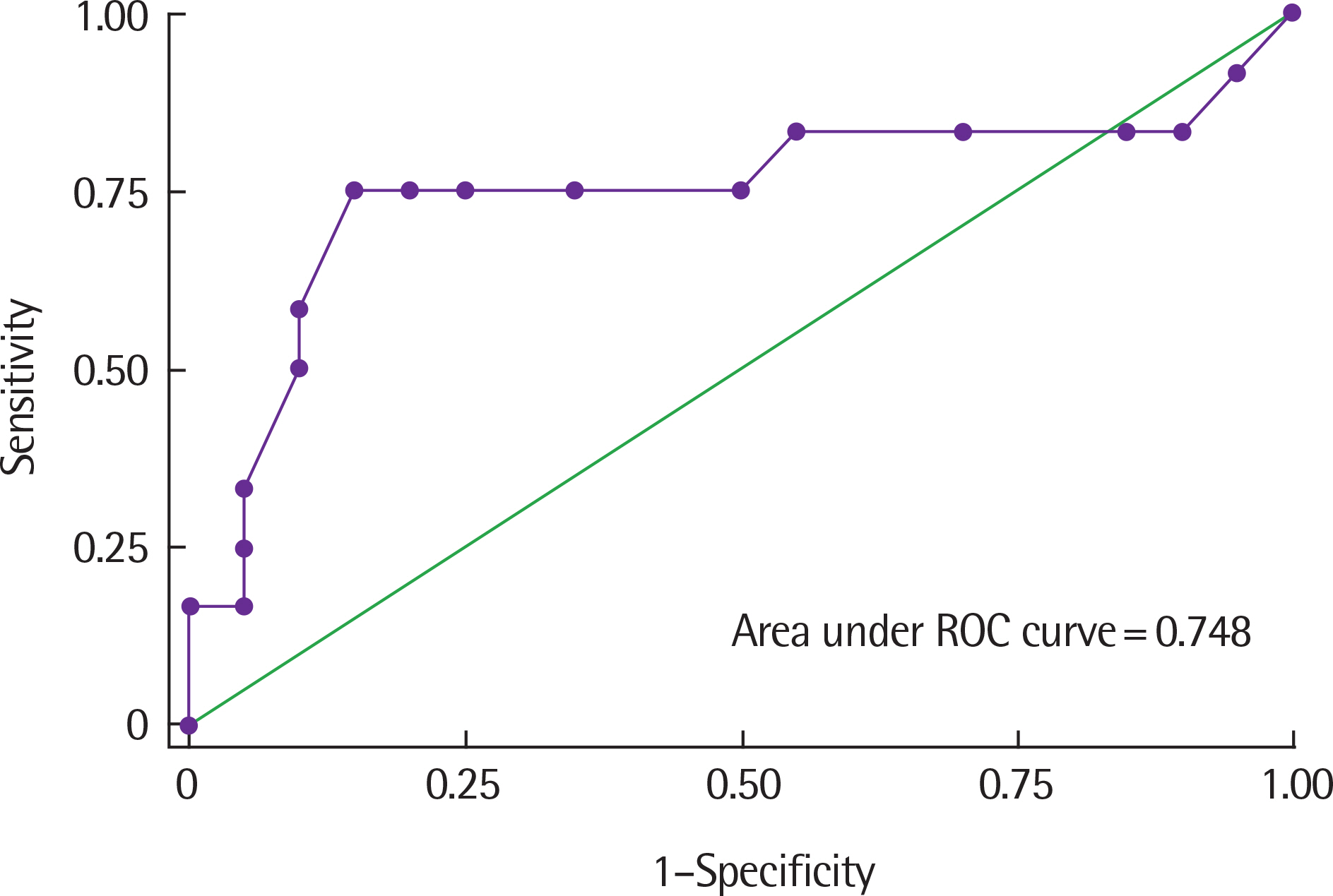
The number of adult patients with TB was 36 (father 68%, mother 23%, grandparents 8%). The patients who came into close contact with the LTBI group were older (47.0±12.8 years vs. 41.3±6.6 years) and had higher erythrocyte sedimentation rate (ESR) levels than those of the second group. The rate of negative acid-fast-bacilli smear with positive culture results in patients who came into contact with the LBTI group was higher than in the second group. The cutoff value of ESR for the diagnosis of LTBI was 31 mm/hr with a sensitivity of 0.75 and a specificity of 0.85 (area under curve=0.748).
CONCLUSION
Adult pulmonary TB patients who are older and have higher ESR levels may be risk factors for LTBI in children coming into close contact with them.
MeSH Terms
Figure
Cited by 1 articles
-
Childhood Tuberculosis Contact Investigation and Treatment of Latent Tuberculosis Infection: a Single Center Study, 2014–2017
Woo Jin Hwang, Go Un Lee, So Hyun Kim, Eun Young Cho
Pediatr Infect Vaccine. 2019;26(1):32-41. doi: 10.14776/piv.2019.26.e4.
Reference
-
1. World Health Organization. Global tuberculosis control: WHO Report 2010. Geneva (Switzerland): World Health Organization;2011. p. 9–27.2. Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012; 367:348–61.
Article3. Kim HJ. Current status of tuberculosis in Korea. Korean J Med. 2012; 82:257–62.
Article4. Mack U, Migliori GB, Sester M, Rieder HL, Ehlers S, Goletti D, et al. LTBI: latent tuberculosis infection or lasting immune responses to M. tuberculosis? A TBNET consensus statement. Eur Respir J. 2009; 33:956–73.
Article5. Marais BJ, Gie RP, Schaaf HS, Beyers N, Donald PR, Starke JR. Childhood pulmonary tuberculosis: old wisdom and new challenges. Am J Respir Crit Care Med. 2006; 173:1078–90.6. Joint Committee for the Development of Korean Guidelines for Tuberculosis Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. 2nd ed.Cheongju: Korea Centers for Disease Control and Prevention;2014. p. 143–5.7. Riley RL, Moodie AS. Infectivity of patients with pulmonary tuberculosis in inner city homes. Am Rev Respir Dis. 1974; 110:810–2.8. Wood R, Johnstone-Robertson S, Uys P, Hargrove J, Middelkoop K, Lawn SD, et al. Tuberculosis transmission to young children in a South African community: modeling household and community infection risks. Clin Infect Dis. 2010; 51:401–8.
Article9. Gessner BD, Weiss NS, Nolan CM. Risk factors for pediatric tuberculosis infection and disease after household exposure to adult index cases in Alaska. J Pediatr. 1998; 132(3 Pt 1):509–13.
Article10. Behr MA, Warren SA, Salamon H, Hopewell PC, Ponce de Leon A, Daley CL, et al. Transmission of Mycobacterium tuberculosis from patients smear-negative for acid-fast bacilli. Lancet. 1999; 353:444–9.
Article11. Nakaoka H, Lawson L, Squire SB, Coulter B, Ravn P, Brock I, et al. Risk for tuberculosis among children. Emerg Infect Dis. 2006; 12:1383–8.
Article12. Joint Committee for the Development of Korean Guidelines for Tuberculosis Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. Cheongju: Korea Centers for Disease Control and Prevention;2011. p. 141–9.13. Al-Marri MR, Kirkpatrick MB. Erythrocyte sedimentation rate in childhood tuberculosis: is it still worthwhile? Int J Tuberc Lung Dis. 2000; 4:237–9.14. Furuhashi K, Shirai T, Suda T, Chida K. Inflammatory markers in active pulmonary tuberculosis: association with Th1/Th2 and Tc1/Tc2 balance. Kekkaku. 2012; 87:1–7.15. Ali NS, Hussain SF, Azam SI. Is there a value of mantoux test and erythrocyte sedimentation rate in pre-employment screening of health care workers for tuberculosis in a high prevalence country? Int J Tuberc Lung Dis. 2002; 6:1012–6.16. Walzl G, Ronacher K, Djoba Siawaya JF, Dockrell HM. Biomarkers for TB treatment response: challenges and future strategies. J Infect. 2008; 57:103–9.
Article17. Lobue P, Menzies D. Treatment of latent tuberculosis infection: an update. Respirology. 2010; 15:603–22.
Article18. Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Nelson LJ, et al. The clinical epidemiology of childhood pulmonary tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004; 8:278–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Survey of Secondary Infections within the Households of Newly Diagnosed Tuberculosis Patients
- Prevalence and Risk Factors for Mycobacterium tuberculosis Infection among Contacts of Pulmonary Tuberculosis Patients
- A Study on Clinical Manifestations of Pulmonary Tuberculosis and Tuberculosis Contact Investigation in School-Age Children and Adolescents at Two Centers
- Korean Guidelines for Diagnosis and Treatment of Tuberculosis in Children and Adolescents
- Childhood Tuberculosis Contact Investigation and Treatment of Latent Tuberculosis Infection: a Single Center Study, 2014–2017