Ann Rehabil Med.
2012 Oct;36(5):729-734.
Surgical Treatments on Patients with Anterior Cervical Hyperostosis-Derived Dysphagia
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul Veterans Hospital, Seoul 134-791, Korea. yang7310@naver.com
- 2Department of Orthopedic Surgery, Seoul Veterans Hospital, Seoul 134-791, Korea.
- 3Department of Neurosurgery, Seoul Veterans Hospital, Seoul 134-791, Korea.
- 4Ahn Ui Health Center, Hamyang-gun 676-823, Korea.
Abstract
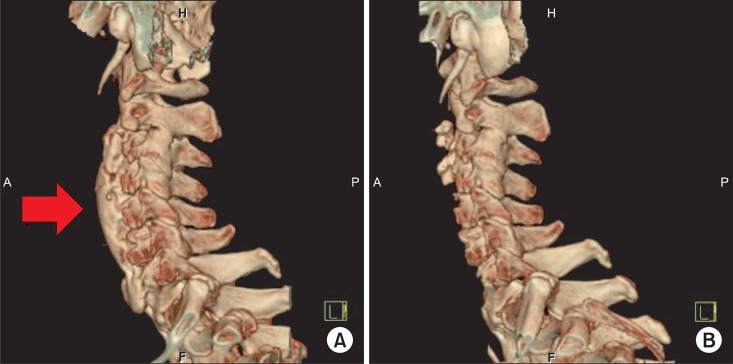
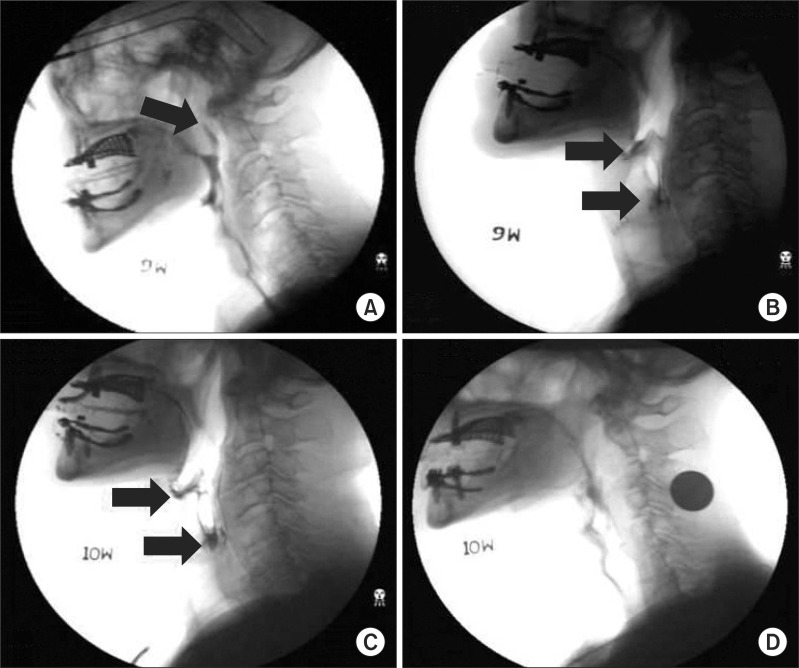
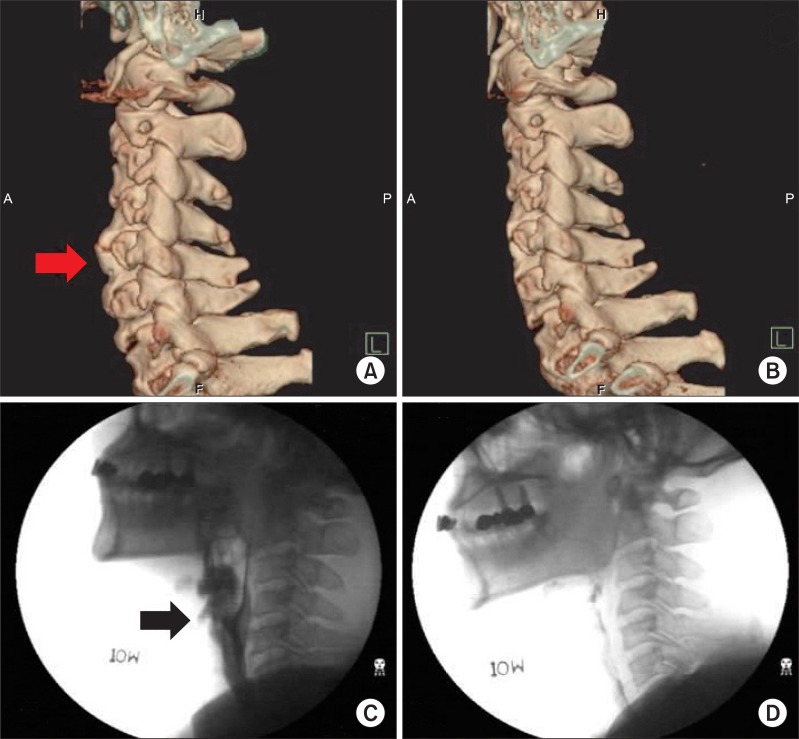
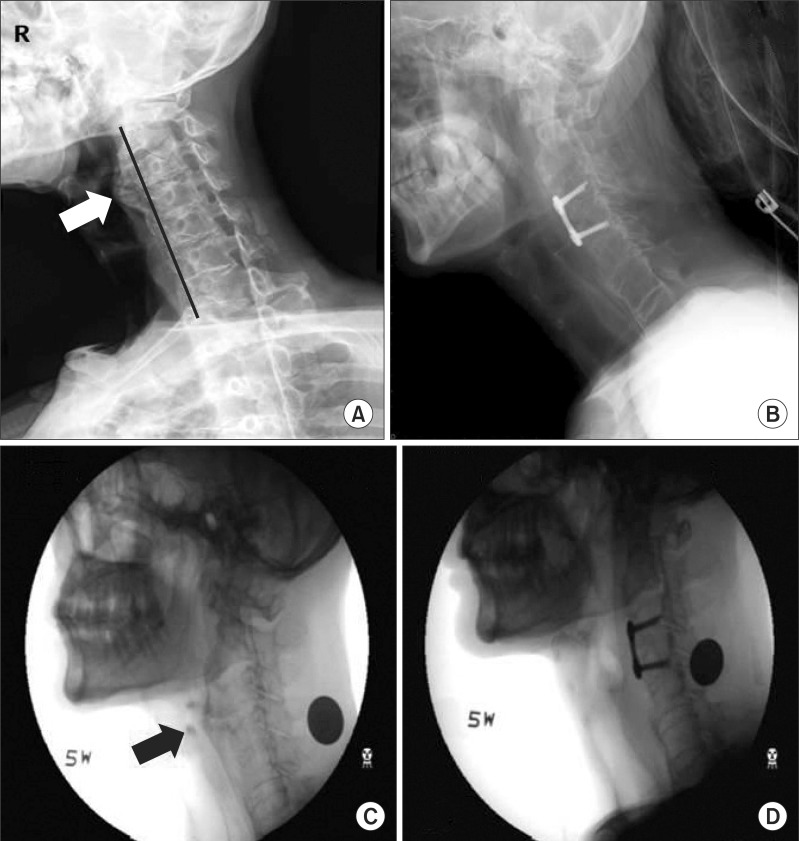
- Anterior cervical hyperostosis may be a cause of dysphagia. For anterior cervical hyperostosis, medical or surgical treatments can be adhibited in view of the causative mechanisms and intensities of dysphagia. We report 3 cases of cervical hyperostosis-derived progressive dysphagia that underwent operation. Radiologic diagnosis and Video Fluoroscopic Swallowing Study were performed on the three patients for evaluation. One had history of recurrent aspiration pneumonia accompanied by weight loss, another complained of dysphagia only when swallowing pills, and the third experienced recurrence symptom with reossification. All patients reported gradual improvement of dysphagia immediately after their cervical osteophytes were resected through the anterior approach. In relation to postoperative improvement, however, they expressed different degrees of satisfaction according to severity of symptoms. Surgical treatment, performed for the anterior cervical hyperostosis-derived dysphagia, can immediately relieve symptoms of difficulty in swallowing. This might especially be considered as an appropriate treatment option for severe dysphagia.
Keyword
MeSH Terms
Figure
Reference
-
1. Freed ML, Freed L, Chatburn RL, Christian M. Electrical stimulation for swallowing disorders caused by stroke. Respir Care. 2001; 46:466–474. PMID: 11309186.2. Utsinger PD, Resnick D, Shapiro R. Diffuse skeletal abnormalities in Forestier disease. Arch Intern Med. 1976; 136:763–768. PMID: 938166.
Article3. Sobol SM, Rigual NR. Anterolateral extrapharyngeal approach for cervical osteophyte-induced dysphagia. Literature review. Ann Otol Rhinol Laryngol. 1984; 93:498–504. PMID: 6388464.4. Kissel P, Youmans JR. Posttraumatic anterior cervical osteophyte and dysphagia: surgical report and literature review. J Spinal Disord. 1992; 5:104–107. PMID: 1571607.5. Eviatar E, Harell M. Diffuse idiopathic skeletal hyperostosis with dysphagia (a review). J Laryngol Otol. 1987; 101:627–632. PMID: 3496409.6. Kodama M, Sawada H, Udaka F, Kameyama M, Koyama T. Dysphagia caused by an anterior cervical osteophyte: case report. Neuroradiology. 1995; 37:58–59. PMID: 7708191.
Article7. McGarrah PD, Teller D. Posttraumatic cervical osteophytosis causing progressive dysphagia. South Med J. 1997; 90:858–860. PMID: 9258320.
Article8. Fahrer H, Markwalder T. Dysphagia caused by diffuse idiopathic skeletal hyperostosis. Clin Rheumatol. 1988; 7:117–121. PMID: 3409642.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Traction May Induce Acute Onset Dysphagia With Diffuse Idiopathic Skeletal Hyperostosis After Anterior Cervical Discectomy
- Dysphagia Due to Diffuse Idiopathic Skeletal Hyperostosis of The Cervical Spine: A Case Report
- A Case of Dysphagia due to Cricopharyngeal Dysfunction and Diffuse Idiopathic Skeletal Hyperostosis
- Giant Anterior Cervical Osteophyte Leading to Dysphagia
- Swallowing Difficulty in Diffuse Idiopathic Skeletal Hyperostosis with Metabolic Syndrome