J Korean Assoc Oral Maxillofac Surg.
2017 Aug;43(4):276-281. 10.5125/jkaoms.2017.43.4.276.
Lateral approach for maxillary sinus membrane elevation without bone materials in maxillary mucous retention cyst with immediate or delayed implant rehabilitation: case reports
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Medicine, Dong-A University, Busan, Korea. bbp2000@hanmail.net
- 2CS Dental Hospital, Busan, Korea.
- KMID: 2391360
- DOI: http://doi.org/10.5125/jkaoms.2017.43.4.276
Abstract
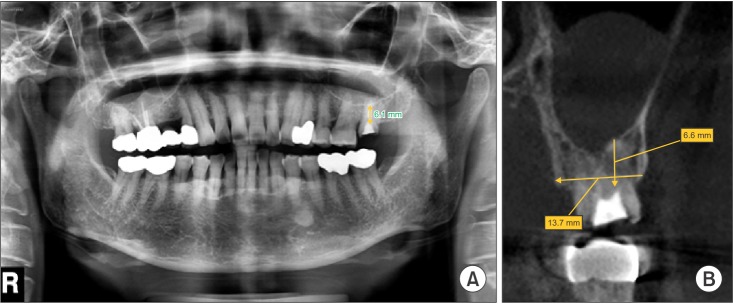
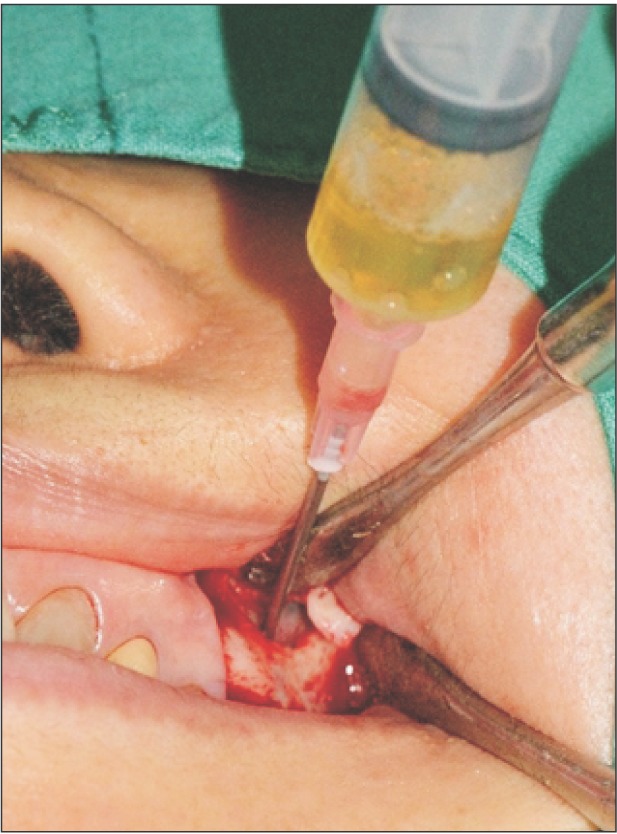
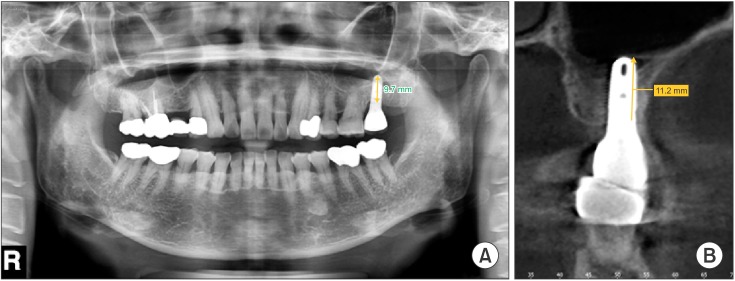
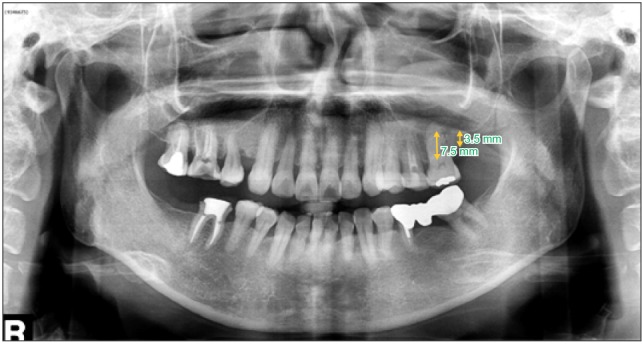
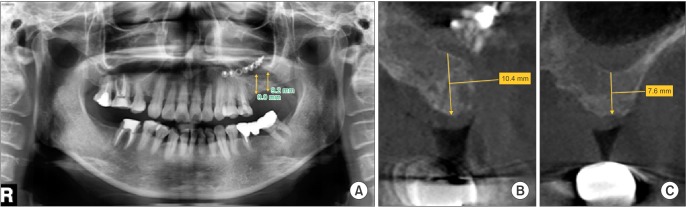
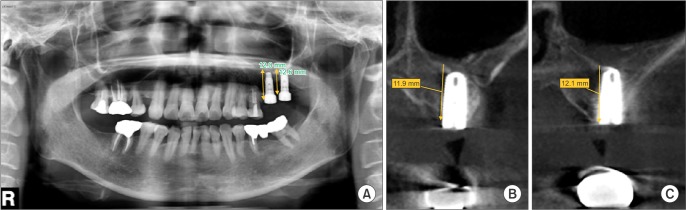
- This case series study demonstrates the possibility of successful implant rehabilitation without bone augmentation in the atrophic posterior maxilla with cystic lesion in the sinus. Sinus lift without bone graft using the lateral approach was performed. In one patient, the cyst was aspirated and simultaneous implantation under local anesthesia was performed, whereas the other cyst was removed under general anesthesia, and the sinus membrane was elevated in a second process, followed by implantation. In both cases, tapered 11.5-mm-long implants were utilized. With all of the implants, good stability and appropriate bone height were achieved. The mean bone level gain was 5.73 mm; adequate bone augmentation around the implants was shown, the sinus floor was moved apically, and the cyst was no longer radiologically detected. Completion of all of the treatments required an average of 12.5 months. The present study showed that sufficient bone formation and stable implantation in a maxilla of insufficient bone volume are possible through sinus lift without bone materials. The results serve to demonstrate, moreover, that surgical treatment of mucous retention cyst can facilitate rehabilitation. These techniques can reduce the risk of complications related to bone grafts, save money, and successfully treat antral cyst.
MeSH Terms
Figure
Cited by 1 articles
-
Sinus membrane elevation and implant placement
Young-Kyun Kim, Jeong-Kui Ku
J Korean Assoc Oral Maxillofac Surg. 2020;46(4):292-298. doi: 10.5125/jkaoms.2020.46.4.292.
Reference
-
1. Thor A, Rasmusson L, Wennerberg A, Thomsen P, Hirsch JM, Nilsson B, et al. The role of whole blood in thrombin generation in contact with various titanium surfaces. Biomaterials. 2007; 28:966–974. PMID: 17095084.
Article2. Esposito M, Grusovin MG, Worthington HV, Coulthard P. Interventions for replacing missing teeth: bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2006; (1):CD003607. PMID: 16437460.
Article3. Garg AK. Augmentation grafting of the maxillary sinus for placement of dental implants: anatomy, physiology, and procedures. Implant Dent. 1999; 8:36–46. PMID: 10356455.4. Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology--eleven years of surgical experience (1979-1990). J Oral Implantol. 1990; 16:199–209. PMID: 2098563.5. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–616. PMID: 6993637.6. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004; 75:511–516. PMID: 15152813.
Article7. Tong DC, Rioux K, Drangsholt M, Beirne OR. A review of survival rates for implants placed in grafted maxillary sinuses using meta-analysis. Int J Oral Maxillofac Implants. 1998; 13:175–182. PMID: 9581402.8. Thor A, Sennerby L, Hirsch JM, Rasmusson L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: an evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg. 2007; 65(7 Suppl 1):64–72. PMID: 17586351.
Article9. Li J, Wang HL. Common implant-related advanced bone grafting complications: classification, etiology, and management. Implant Dent. 2008; 17:389–401. PMID: 19077576.
Article10. Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:180–184. PMID: 17234532.
Article11. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007; 22(Suppl):49–70. PMID: 18437791.12. Moreno Vazquez JC, Gonzalez de Rivera AS, Gil HS, Mifsut RS. Complication rate in 200 consecutive sinus lift procedures: guidelines for prevention and treatment. J Oral Maxillofac Surg. 2014; 72:892–901. PMID: 24583086.
Article13. Kasabah S, Krug J, Simůnek A, Lecaro MC. Can we predict maxillary sinus mucosa perforation? Acta Medica (Hradec Kralove). 2003; 46:19–23. PMID: 12747535.
Article14. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg. 1997; 55:936–939. discussion 940. PMID: 9294502.
Article15. Palma VC, Magro-Filho O, de Oliveria JA, Lundgren S, Salata LA, Sennerby L. Bone reformation and implant integration following maxillary sinus membrane elevation: an experimental study in primates. Clin Implant Dent Relat Res. 2006; 8:11–24. PMID: 16681489.
Article16. Lundgren S, Andersson S, Gualini F, Sennerby L. Bone reformation with sinus membrane elevation: a new surgical technique for maxillary sinus floor augmentation. Clin Implant Dent Relat Res. 2004; 6:165–173. PMID: 15726851.
Article17. Moon JW, Sohn DS, Heo JU, Shin HI, Jung JK. New bone formation in the maxillary sinus using peripheral venous blood alone. J Oral Maxillofac Surg. 2011; 69:2357–2367. PMID: 21719179.
Article18. de Oliveira GR, Olate S, Cavalieri-Pereira L, Pozzer L, Asprino L, de Moraes M, et al. Maxillary sinus floor augmentation using blood without graft material. Preliminary results in 10 patients. J Oral Maxillofac Surg. 2013; 71:1670–1675. PMID: 23891012.
Article19. Takata T, Wang HL, Miyauchi M. Migration of osteoblastic cells on various guided bone regeneration membranes. Clin Oral Implants Res. 2001; 12:332–338. PMID: 11488862.
Article20. Misch CE. The maxillary sinus lift and sinus graft surgery. In : Misch CE, editor. Contemporary implant dentistry. 2nd ed. St. Louis: CV Mosby;1999. p. 482–493.21. Frost A, Jonsson KB, Ridefelt P, Nilsson O, Ljunghall S, Ljunggren O. Thrombin, but not bradykinin, stimulates proliferation in isolated human osteoblasts, via a mechanism not dependent on endogenous prostaglandin formation. Acta Orthop Scand. 1999; 70:497–503. PMID: 10622485.
Article22. Pagel CN, de Niese MR, Abraham LA, Chinni C, Song SJ, Pike RN, et al. Inhibition of osteoblast apoptosis by thrombin. Bone. 2003; 33:733–743. PMID: 14555279.
Article23. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004; 91:4–15. PMID: 14691563.
Article24. Lundgren S, Andersson S, Sennerby L. Spontaneous bone formation in the maxillary sinus after removal of a cyst: coincidence or consequence? Clin Implant Dent Relat Res. 2003; 5:78–81. PMID: 14536041.
Article25. Paparella MM. Mucosal cyst of the maxillary sinus. Arch Otolaryngol. 1963; 77:650–670. PMID: 13941289.
Article26. MacDonald-Jankowski DS. Mucosal antral cysts observed within a London inner-city population. Clin Radiol. 1994; 49:195–198. PMID: 8143412.
Article27. Ziccardi VB, Betts NJ. Complications of maxillary sinus augmentation. In : Jensen OT, editor. The sinus bone graft. Chicago: London: Quintessence Publishing;1999. p. 201–208.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sinus lifts in the presence of pseudoantral and mucous retention cysts
- Implant placement simultaneously sinus augmentation using crestal approach in severely atrophic maxilla; minimally invasive approach
- One-step Approach for Radicular Cyst Removal in the Maxillary Sinus and Implant Placement in the Posterior Maxilla: A Case Report with a 3-Year Follow-Up
- Clinical evaluation of sinus bone graft in patients with mucous retention cyst
- Evaluation of clinical outcomes of implants placed into the maxillary sinus with a perforated sinus membrane: a retrospective study