Korean J Crit Care Med.
2017 Aug;32(3):240-246. 10.4266/kjccm.2017.00360.
Biochemical Markers as Predictors of In-Hospital Mortality in Patients with Severe Trauma: A Retrospective Cohort Study
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine and Institute of Health Sciences, Jinju, Korea.
- 2Department of Thoracic and Cardiovascular Surgery, Gyeongsang National University Changwon Hospital, Gyeongsang National University School of Medicine and Institute of Health Sciences, Changwon, Korea. romejuliet@naver.com
- 3Department of Neurology, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 4Department of Thoracic and Cardiovascular Surgery, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine and Institute of Health Sciences, Jinju, Korea.
- 5Department of Neurosurgery, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- KMID: 2391183
- DOI: http://doi.org/10.4266/kjccm.2017.00360
Abstract
- BACKGROUND
Initial evaluation of injury severity in trauma patients is an important and challenging task. We aimed to assess whether easily measurable biochemical parameters (hemoglobin, pH, and prothrombin time/international normalized ratio [PT/INR]) can predict in-hospital mortality in patients with severe trauma.
METHODS
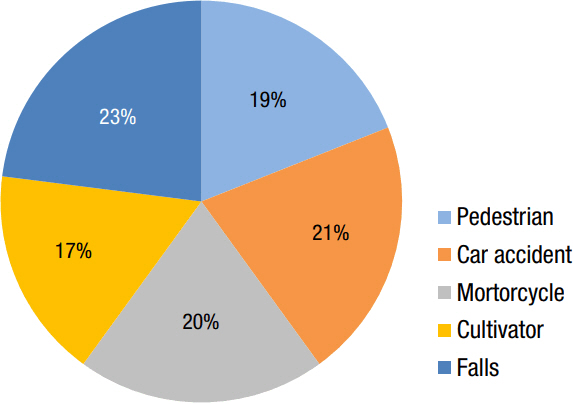
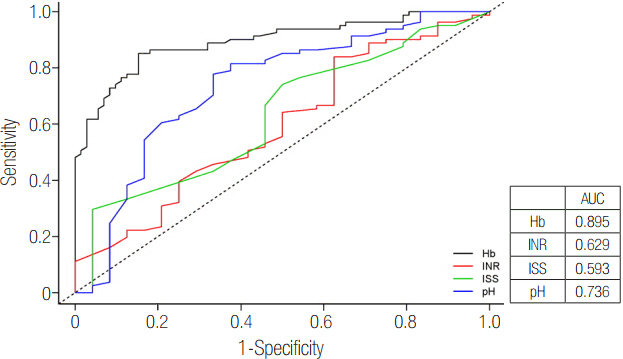
This retrospective study involved review of the medical records of 315 patients with severe trauma and an injury severity score >15 who were managed at Gyeongsang National University Hospital between January 2005 and December 2015. We extracted the following data: in-hospital mortality, injury severity score, and initial hemoglobin level, pH, and PT/INR. The predictive values of these variables were compared using receiver operation characteristic curves.
RESULTS
Of the 315 patients, 72 (22.9%) died. The in-hospital mortality rates of patients with hemoglobin levels <8.4 g/dl and ≥8.4 g/dl were 49.8% and 9.9%, respectively (P < 0.001). At a cutoff hemoglobin level of 8.4 g/dl, the sensitivity and specificity values for mortality were 81.9% and 86.4%, respectively. At a pH cutoff of 7.25, the sensitivity and specificity values for mortality were 66.7% and 77.8%, respectively; 66.7% of patients with a pH <7.25 died versus 22.2% with a pH ≥7.25 (P < 0.001). The in-hospital mortality rates for patients with PT/INR values ≥1.4 and <1.4 were 37.5% and 16%, respectively (P < 0.001; sensitivity, 37.5%; specificity, 84%).
CONCLUSIONS
Using the suggested cutoff values, hemoglobin level, pH, and PT/INR can simply and easily be used to predict in-hospital mortality in patients with severe trauma.
MeSH Terms
Figure
Reference
-
References
1. Sammour T, Kahokehr A, Caldwell S, Hill AG. Venous glucose and arterial lactate as biochemical predictors of mortality in clinically severely injured trauma patients: a comparison with ISS and TRISS. Injury. 2009; 40:104–8.2. Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988; 28:69–77.
Article3. Mikhail J. The trauma triad of death: hypothermia, acidosis, and coagulopathy. AACN Clin Issues. 1999; 10:85–94.
Article4. Kashuk JL, Moore EE, Millikan JS, Moore JB. Major abdominal vascular trauma: a unified approach. J Trauma. 1982; 22:672–9.5. Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The new Injury Severity Score: a more accurate predictor of in-hospital mortality than the Injury Severity Score. J Trauma. 2004; 56:1312–20.
Article6. Rutledge R, Fakhry S, Rutherford E, Muakkassa F, Meyer A. Comparison of APACHE II, Trauma Score, and Injury Severity Score as predictors of outcome in critically injured trauma patients. Am J Surg. 1993; 166:244–7.
Article7. Raum MR, Nijsten MW, Vogelzang M, Schuring F, Lefering R, Bouillon B, et al. Emergency trauma score: an instrument for early estimation of trauma severity. Crit Care Med. 2009; 37:1972–7.
Article8. Knottenbelt JD. Low initial hemoglobin levels in trauma patients: an important indicator of ongoing hemorrhage. J Trauma. 1991; 31:1396–9.9. Bruns B, Lindsey M, Rowe K, Brown S, Minei JP, Gentilello LM, et al. Hemoglobin drops within minutes of injuries and predicts need for an intervention to stop hemorrhage. J Trauma. 2007; 63:312–5.
Article10. Kaplan LJ, Kellum JA. Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med. 2004; 32:1120–4.
Article11. Summersgill A, Kanter M, Fraser RM, Caputo ND, Simon R. Determining the utility of metabolic acidosis for trauma patients in the emergency department. J Emerg Med. 2015; 48:693–8.
Article12. Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit Care Med. 1992; 20:80–93.
Article13. Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009; 23:231–40.
Article14. Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J Trauma. 2008; 6:1211–7.
Article15. Brohi K. Trauma induced coagulopathy. J R Army Med Corps. 2009; 155:320–2.
Article16. Verma A, Kole T. International normalized ratio as a predictor of mortality in trauma patients in India. World J Emerg Med. 2014; 5:192–5.
Article17. Peltan ID, Vande Vusse LK, Maier RV, Watkins TR. An international normalized ratio-based definition of acute traumatic coagulopathy is associated with mortality, venous thromboembolism, and multiple organ failure after injury. Crit Care Med. 2015; 43:1429–38.
Article18. Owen JL, Bolenbaucher RM, Moore ML. Trauma registry databases: a comparison of data abstraction, interpretation, and entry at two level I trauma centers. J Trauma. 1999; 46:1100–4.19. Scheingraber S, Rehm M, Sehmisch C, Finsterer U. Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology. 1999; 90:1265–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of the Initial Risk Factors for Mortality among Patients with Severe Trauma on Admission to the Emergency Department
- Usefulness of Shock Index to Predict Outcomes of Trauma Patient: A Retrospective Cohort Study
- The prognostic usefulness of the lactate/albumin ratio for predicting multiple organ dysfunction syndrome in severe trauma
- Changes of Bone Mineral Density and Biochemical Bone Markers during Perimenopausal Period for Healthy Women: Retrospective Cohort Study
- Effect of the Emergency Trauma Team's Management on the Treatment of Patients with Multiple Severe Trauma