Ann Hepatobiliary Pancreat Surg.
2017 Aug;21(3):114-121. 10.14701/ahbps.2017.21.3.114.
Diaphragmatic hernia following liver resection: case series and review of the literature
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Surgery and Liver Transplantation, Henri Mondor Hospital, Créteil, France. daniel.azoulay@hmn.aphp.fr
- 2INSERM, U955, Créteil, France.
- KMID: 2389987
- DOI: http://doi.org/10.14701/ahbps.2017.21.3.114
Abstract
- BACKGROUNDS/AIMS
Postoperative diaphragmatic hernia, following liver resection, is a rare complication.
METHODS
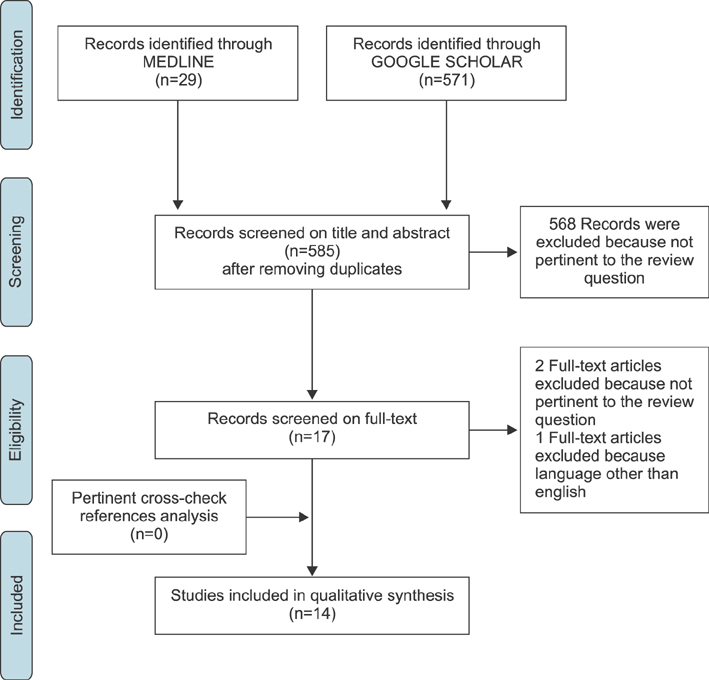
Data of patients who underwent major hepatectomy for liver tumors, between 2011 and 2015 were retrospectively reviewed. The literature was searched for studies reporting the occurrence of diaphragmatic hernia following liver resection.
RESULTS
Diaphragmatic hernia developed in 2.3% of patients (3/131) with a median delay of 14 months (4-31 months). One patient underwent emergency laparotomy for bowel obstruction and two patients underwent elective diaphragmatic hernia repair. At last follow-up, no recurrences were observed. Fourteen studies including 28 patients were identified in the literature search (donor hepatectomy, n=11: hepatectomy for liver tumors, n=17). Diaphragmatic hernia was repaired emergently in 42.9% of cases and digestive resection was necessary in 28.5% of the cases. One patient died 3 months after hepatectomy, secondary to sepsis, from a segment of small bowel that perforated into the diaphragmatic hernia.
CONCLUSIONS
Although rare, diaphragmatic hernia should be considered as an important complication, especially in living donor liver transplant patients. Diaphragmatic hernia should be repaired surgically, even for asymptomatic patients.
MeSH Terms
Figure
Cited by 1 articles
-
Acquired diaphragmatic hernia after hepatectomy and liver transplantation in adults and children: A case series and literature review
Valentine Martin, Emilie Gregoire, Sophie Chopinet, Olivier Scatton, Rémi Dubois, Antoinette Lasseur, Jérôme Dumortier, Olivier Boillot
Ann Hepatobiliary Pancreat Surg. 2021;25(4):462-471. doi: 10.14701/ahbps.2021.25.4.462.
Reference
-
1. Lee MK 4th, Gao F, Strasberg SM. Perceived complexity of various liver resections: results of a survey of experts with development of a complexity score and classification. J Am Coll Surg. 2015; 220:64–69.2. Zimmitti G, Roses RE, Andreou A, Shindoh J, Curley SA, Aloia TA, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg. 2013; 17:57–64. discussion p.64-65.3. Rubikas R. Diaphragmatic injuries. Eur J Cardiothorac Surg. 2001; 20:53–57.4. Tabrizian P, Jibara G, Shrager B, Elsabbagh AM, Roayaie S, Schwartz ME. Diaphragmatic hernia after hepatic resection: case series at a single Western institution. J Gastrointest Surg. 2012; 16:1910–1914.5. Willemse P, Schütte PR, Plaisier PW. Thoracoscopic repair of a Bochdalek hernia in an adult. Surg Endosc. 2003; 17:162.6. Hawxby AM, Mason DP, Klein AS. Diaphragmatic hernia after right donor and hepatectomy: a rare donor complication of partial hepatectomy for transplantation. Hepatobiliary Pancreat Dis Int. 2006; 5:459–461.7. Kousoulas L, Becker T, Richter N, Emmanouilidis N, Schrem H, Barg-Hock H, et al. Living donor liver transplantation: effect of the type of liver graft donation on donor mortality and morbidity. Transpl Int. 2011; 24:251–258.8. Dieter RA Jr, Spitz J, Kuzycz G. Incarcerated diaphragmatic hernia with intrathoracic bowel obstruction after right liver donation. Int Surg. 2011; 96:239–244.9. Vernadakis S, Paul A, Kykalos S, Fouzas I, Kaiser GM, Sotiropoulos GC. Incarcerated diaphragmatic hernia after right hepatectomy for living donor liver transplantation: case report of an extremely rare late donor complication. Transplant Proc. 2012; 44:2770–2772.10. Mizuno S, Tanemura A, Isaji S. Incarcerated left diaphragmatic hernia following left hepatectomy for living donor liver transplantation. Transpl Int. 2014; 27:e65–e67.11. Jeng KS, Huang CC, Lin CK, Lin CC, Wu JM, Chen KH, et al. Early incarcerated diaphragmatic hernia following right donor hepatectomy: a case report. Transplant Proc. 2015; 47:815–816.12. Livingstone SM, Andres A, Shapiro AM, Kneteman NN, Bigam DL. Diaphragmatic hernia after living donor right hepatectomy: proposal for a screening protocol. Transplant Direct. 2016; 2:e84.13. Hemming AW, Reed AI, Langham MR, Fujita S, van der Werf WJ, Howard RJ. Hepatic vein reconstruction for resection of hepatic tumors. Ann Surg. 2002; 235:850–858.14. Sugita M, Nagahori K, Kudo T, Yamanaka K, Obi Y, Shizawa R, et al. Diaphragmatic hernia resulting from injury during microwave-assisted laparoscopic hepatectomy. Surg Endosc. 2003; 17:1849–1850.15. Matz D, Kirchhoff P, Kocher TM, Heizmann O. Consecutive cecum perforation due to incarcerated diaphragmatic hernia after liver surgery. Int J Colorectal Dis. 2009; 24:1353–1354.16. Schellhaas E, Döbler O, Kroesen AJ, Buhr HJ, Hotz HG. Gangrenous intrathoracic appendicitis, a rare cause of right-sided chest pain: report of a case. Surg Today. 2010; 40:874–877.17. Lodhia JV, Appiah S, Tcherveniakov P, Krysiak P. Diaphragmatic hernia masquerading as a pulmonary metastasis. Ann R Coll Surg Engl. 2015; 97:e27–e29.18. Patrizi A, Jezequel C, Sulpice L, Meunier B, Rayar M, Boudjema K. Disposable bipolar irrigated sealer (Aquamantys(®)) for liver resection: use with caution. Updates Surg. 2016; 68:171–177.19. Lim C, Compagnon P, Sebagh M, Salloum C, Calderaro J, Luciani A, et al. Hepatectomy for hepatocellular carcinoma larger than 10 cm: preoperative risk stratification to prevent futile surgery. HPB (Oxford). 2015; 17:611–623.20. Memeo R, de'Angelis N, Compagnon P, Salloum C, Cherqui D, Laurent A, et al. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg. 2014; 38:2919–2926.21. Azoulay D, Marin-Hargreaves G, Castaing D, Adam R, Savier E, Bismuth H. The anterior approach: the right way for right massive hepatectomy. J Am Coll Surg. 2001; 192:412–417.22. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009; 3:e123–e130.23. Al-Nouri O, Hartman B, Freedman R, Thomas C, Esposito T. Diaphragmatic rupture: Is management with biological mesh feasible? Int J Surg Case Rep. 2012; 3:349–353.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Morgagni Hernia
- Congenital diaphragmatic Hernia Associated with Hypoplasia of the Lung
- Diaphragmatic Hernia of the Right Hepatic Lobe Mistaken for Diaphragmatic Paralysis in Adult
- Unilateral Congenital Diaphragmatic Eventration Mimicking Congenital Diaphragmatic Hernia
- A Case of Maternal Diaphragmatic Hernia in Pregnancy