J Gastric Cancer.
2016 Dec;16(4):254-259. 10.5230/jgc.2016.16.4.254.
Outcome of Gastric Cancer Surgery in Elderly Patients
- Affiliations
-
- 1Department of Surgery, School of Medicine, Chosun University, Gwangju, Korea. sungsoo73@chosun.ac.kr
- KMID: 2389851
- DOI: http://doi.org/10.5230/jgc.2016.16.4.254
Abstract
- PURPOSE
Owing to increased life expectancy, the number of elderly patients with gastric cancer has increased. This study aimed to identify the outcomes of gastric cancer patients aged 80 years or older through comparison of their clinicopathological characteristics, surgical outcomes, and oncologic outcomes.
MATERIALS AND METHODS
Between January 2006 and December 2013, the records of 478 patients who underwent surgery for gastric cancer were retrospectively evaluated. Patients were divided into two groups: patients <80 years old (n=446) and patients ≥80 years old (n=32).
RESULTS
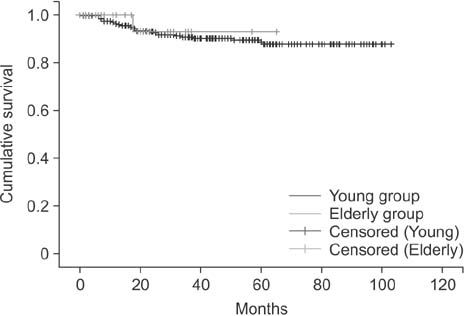
There were no significant differences in sex, body mass index, length of hospital stay, duration of surgery, depth of invasion, nodal metastasis, histologic type, or tumor size between the two groups. However, significant differences were found for the American Society of Anesthesiologist score and the serum albumin level between the two groups. Postoperative morbidity, mortality, disease-free survival, and recurrence rate did not differ between curatively resected patients in the two groups.
CONCLUSIONS
In elderly patients with gastric cancer, active treatment including radical gastrectomy is necessary.
MeSH Terms
Figure
Reference
-
1. Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012; 13:790–801.2. Korean Statistical Information Service [Internet]. Daejeon: Korean Statistical Information Service;2016. cited 2016 Aug 29. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42&conn_path=I2.3. Tavares A, Gandra A, Viveiros F, Cidade C, Maciel J. Analysis of clinicopathologic characteristics and prognosis of gastric cancer in young and older patients. Pathol Oncol Res. 2013; 19:111–117.4. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.5. National Cancer Information Center [Internet]. Goyang: National Cancer Information Center;2013. cited 2016 Aug 22. Available from: http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040202000000.6. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011; 11:69–77.7. Matsushita I, Hanai H, Kajimura M, Tamakoshi K, Nakajima T, Matsubayashi Y, et al. Should gastric cancer patients more than 80 years of age undergo surgery? Comparison with patients not treated surgically concerning prognosis and quality of life. J Clin Gastroenterol. 2002; 35:29–34.8. Bittner R, Butters M, Ulrich M, Uppenbrink S, Beger HG. Total gastrectomy. Updated operative mortality and long-term survival with particular reference to patients older than 70 years of age. Ann Surg. 1996; 224:37–42.9. Eguchi T, Takahashi Y, Ikarashi M, Kasahara M, Fujii M. Is extended lymph node dissection necessary for gastric cancer in elderly patients? Eur J Surg. 2000; 166:949–953.10. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.11. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.12. Clavien PA, Strasberg SM. Severity grading of surgical complications. Ann Surg. 2009; 250:197–198.13. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.14. Wu CW, Lo SS, Shen KH, Hsieh MC, Lui WY, P'eng FK. Surgical mortality, survival, and quality of life after resection for gastric cancer in the elderly. World J Surg. 2000; 24:465–472.15. Pisanu A, Montisci A, Piu S, Uccheddu A. Curative surgery for gastric cancer in the elderly: treatment decisions, surgical morbidity, mortality, prognosis and quality of life. Tumori. 2007; 93:478–484.16. Saidi RF, Bell JL, Dudrick PS. Surgical resection for gastric cancer in elderly patients: is there a difference in outcome? J Surg Res. 2004; 118:15–20.17. Takeshita H, Ichikawa D, Komatsu S, Kubota T, Okamoto K, Shiozaki A, et al. Surgical outcomes of gastrectomy for elderly patients with gastric cancer. World J Surg. 2013; 37:2891–2898.18. Sun Z, Kong XJ, Jing X, Deng RJ, Tian ZB. Nutritional risk screening 2002 as a predictor of postoperative outcomes in patients undergoing abdominal surgery: a systematic review and meta-analysis of prospective cohort studies. PLoS One. 2015; 10:e0132857.19. Watanabe M, Iwatsuki M, Iwagami S, Ishimoto T, Baba Y, Baba H. Prognostic nutritional index predicts outcomes of gastrectomy in the elderly. World J Surg. 2012; 36:1632–1639.20. Korean Statistical Inforamtion Service [Internet]. Daejeon: Korean Statistical Inforamtion Service;2016. cited 2016 Aug 22. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1YL0201&conn_path=I2.21. Suh M, Choi KS, Lee YY, Park B, Jun JK. Cancer screening in Korea, 2012: results from the Korean National Cancer Screening Survey. Asian Pac J Cancer Prev. 2013; 14:6459–6463.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Resection of Early Gastric Cancer in Elderly
- Laparoscopy-Assisted Distal Gastrectomy for Early Gastric Cancer in the Elderly
- Analysis of Clinicopathological Features and Risk Factors for Severe Complications after Gastrectomy for Gastric Cancer in Elderly Patients
- Comparison of the Clinicopathologic Features and the Survival Rates in Young and Elderly Patients with Gastric Cancer
- Operative Treatment of Patients Over 75 Years Old with Gastric Cancer