J Korean Med Assoc.
2017 Sep;60(9):727-731. 10.5124/jkma.2017.60.9.727.
Definition and treatment of lacrimal drainage disease
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2389791
- DOI: http://doi.org/10.5124/jkma.2017.60.9.727
Abstract
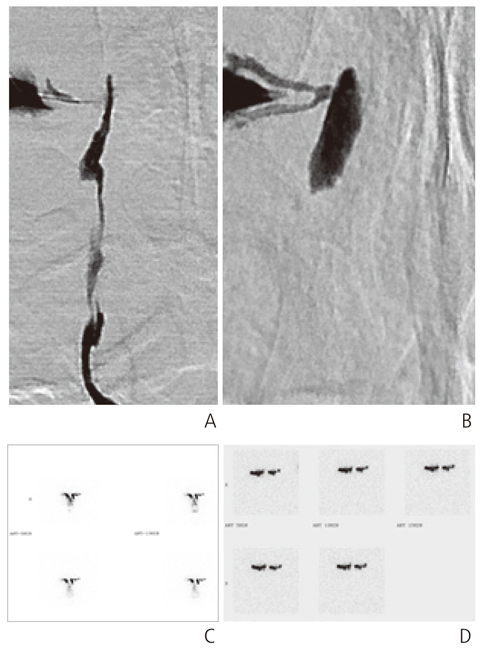
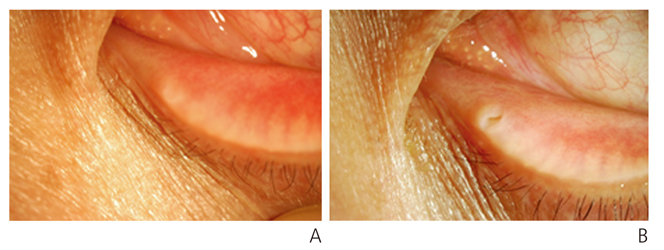
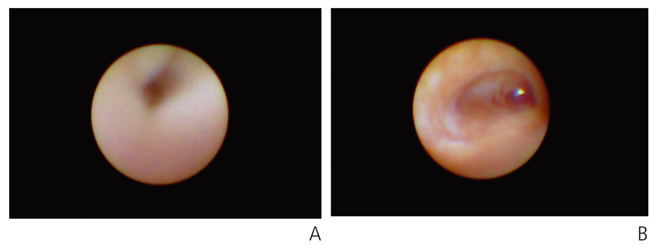
- Epiphora is one of the most common problems in ophthalmological practice, and is caused by dysfunction of the lacrimal pathway. The lacrimal drainage system is a continuous anatomical structure consisting of the lacrimal punctum, inferior and superior canaliculi, common canaliculus, lacrimal sac, and nasolacrimal duct. Lacrimal disease can be medically treated in case of acute inflammation or partial obstruction at the beginning of treatment, but surgical treatment is necessary in most cases. This paper discusses the etiology, clinical features, diagnosis, and surgical treatment of various lacrimal diseases through a selective review of the relevant literature. Advances in lacrimal duct surgery can now be performed in such a way that the structural integrity and normal physiological function of the entire efferent lacrimal pathway is preserved.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Introduction of ophthalmic plastic and reconstructive surgery
Suk-Woo Yang
J Korean Med Assoc. 2017;60(9):717-718. doi: 10.5124/jkma.2017.60.9.717.
Reference
-
1. Jones LT. An anatomical approach to problems of the eyelids and lacrimal apparatus. Arch Ophthalmol. 1961; 66:111–124.
Article2. Paulsen FP, Thale AB, Hallmann UJ, Schaudig U, Tillmann BN. The cavernous body of the human efferent tear ducts: function in tear outflow mechanism. Invest Ophthalmol Vis Sci. 2000; 41:965–970.3. Yoshida M, Hondo R. Transmission of herpes simplex virus infection via lacrimal canaliculi. Ophthalmologica. 1992; 204:101–102.
Article4. Kim DG, Lee JJ, Ham DS, Yang JW. Surgical outcomes of dacryocystorhinostomy in lacrimal drainage obstruction after systemic chemotherapy or radioactive iodine therapy. J Korean Ophthalmol Soc. 2016; 57:1684–1690.
Article5. Kim SD, Koh SI, Kim JD. Diagnosis and therapy of canaliculitis. J Korean Ophthalmol Soc. 1998; 39:2207–2210.6. Ahn SM, Kim HC, Jang JW, Kim SJ. Treatment of the SmartPLUG-related canaliculitis. J Korean Ophthalmol Soc. 2009; 50:1768–1773.
Article7. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology. 1986; 93:1055–1063.8. Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthal Plast Reconstr Surg. 1993; 9:38–41.
Article9. Higashi H, Tamada T, Mizukawa K, Ito K. MR dacryocystography: comparison with dacryoendoscopy in positional diagnosis of nasolacrimal duct obstruction. Radiol Med. 2016; 121:580–587.
Article10. Joo KS, Lee JK. Comparison of lacrimal scintigraphy and fluorescein dye disappearance test in functional blockage of lacrimal system. J Korean Ophthalmol Soc. 2011; 52:1013–1018.
Article11. Jeong S. A simple test for epiphora caused by punctal stenosis. J Korean Ophthalmol Soc. 1998; 39:2864–2866.12. Kwon JK, Chang MW, Baek SH, Lee TS. Punctoplasty using a radiofrequency surgical unit for punctal stenosis. J Korean Ophthalmol Soc. 2012; 53:1727–1731.
Article13. Choi CU, Seo SW, Kim SD. The comparison of punctoplasty and silicone tube intubation in patients with punctal obstruction. J Korean Ophthalmol Soc. 2008; 49:543–547.
Article14. Lee TS, Lee H. Purse-string suture technique for jones tube fixation in conjunctivodacryocystorhinostomy. J Korean Ophthalmol Soc. 2008; 49:1553–1558.
Article15. Rose GE, Welham RA. Jones' lacrimal canalicular bypass tubes: twenty-five years' experience. Eye (Lond). 1991; 5(Pt 1):13–19.
Article16. Davies DL. Lacrymal obstruction: the results of the anastomotic method of treatment (Toti). Proc R Soc Med. 1921; 14(Sect Ophthalmol):59–64.
Article17. Weidenbecher M, Hosemann W, Buhr W. Endoscopic endonasal dacryocystorhinostomy: results in 56 patients. Ann Otol Rhinol Laryngol. 1994; 103(5 Pt 1):363–367.
Article18. Shin IH, Lim HB, Lee JJ, Lee SB. Prognostic factors for successful endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2015; 56:1661–1666.
Article19. Keith CG. Lacrimal obstruction. Trans Ophthalmol Soc U K. 1969; 88:519–522.20. Kim HD, Jeong SK. Silicone tube intubation in acquired nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2000; 41:327–331.21. Kwon YH, Lee YJ. Long-term results of silicone tube intubation in incomplete nasolacrimal duct obstruction (NLDO). J Korean Ophthalmol Soc. 2008; 49:190–194.
Article22. Sasaki T, Nagata Y, Sugiyama K. Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy: part II. Inferior meatal dacryorhinotomy. Am J Ophthalmol. 2005; 140:1070–1074.
Article23. Oh HS, Ahn Y. The incidence and medical treatment of congenital nasolacrimal duct obstruction in Korean infants. J Korean Ophthalmol Soc. 1995; 36:1007–1013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Management of the Lacrimal Drainage System
- Efficacy of Dacryoscintigraphy in Patients with Functional Block of Lacrimal Drainage System
- Dacryoscintigraphy: The Assessment of Epiphora in Children
- Surgical Outcomes of Dacryocystorhinostomy in Lacrimal Drainage Obstruction after Systemic Chemotherapy or Radioactive Iodine Therapy
- Two Cases of Lacrimal Drainage Obstruction Associated With S-1 Anticancer Treatment