Anesth Pain Med.
2017 Jul;12(3):247-250. 10.17085/apm.2017.12.3.247.
The effect-site concentration of remifentanil for blunting hemodynamic responses: comparative study in single-lumen endotracheal and double-lumen endobronchial intubation
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeju National University School of Medicine, Jeju, Korea. hjanesthesia@empas.com
- KMID: 2388841
- DOI: http://doi.org/10.17085/apm.2017.12.3.247
Abstract
- BACKGROUND
This study undertook to compare the effect-site concentration of remifentanil for prevention of hemodynamic responses to endotracheal intubation, employing the single-lumen tracheal tube and the double-lumen bronchial tube during total intravenous anesthesia.
METHODS
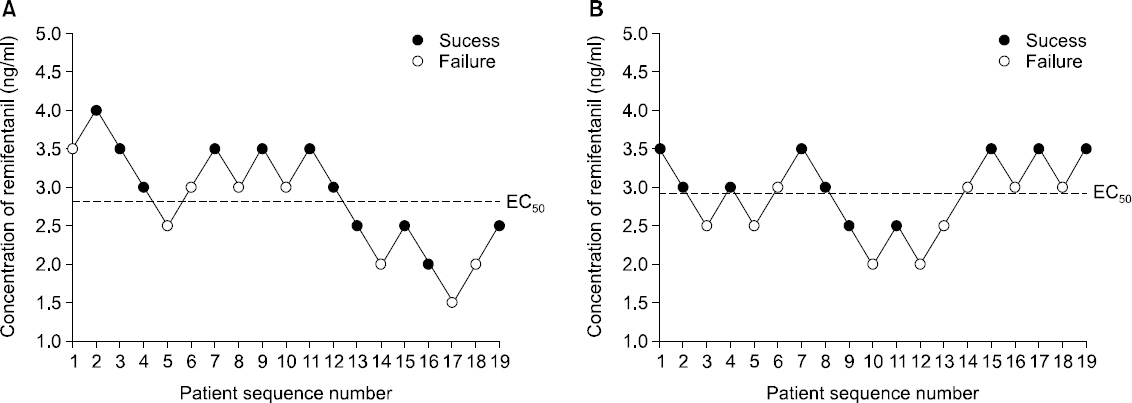
Based on the nature of the surgery, 38 patients undergoing general anesthesia were assigned either to the single-lumen tube group or the double-lumen tube group. Anesthesia was induced by a target controlled infusion of propofol, with an effect-site concentration of 4 µg/ml. Remifentanil was then administered to the first patient in each group, with an effect-site concentration of 3.5 ng/ml. Subsequent concentration of remifentanil was determined by hemodynamic responses of the previous patient to intubation, based on the up-and-down method.
RESULTS
The effect-site concentrations of remifentanil for prevention of hemodynamic responses to endotracheal intubation in 50% of patients (ECâ‚…â‚€) were 2.8 ng/ml (95% CI, 2.0-3.7 ng/ml) in the single-lumen tube group, and 2.9 ng/ml (95% CI, 2.5-3.2 ng/ml) in the double-lumen tube group. No significant difference was observed between the two groups.
CONCLUSIONS
The effect-site concentration of remifentanil for prevention of hemodynamic responses to endotracheal intubation did not differ during total intravenous anesthesia, using either the single-lumen tracheal tube or the double-lumen bronchial tube.
Keyword
MeSH Terms
Figure
Reference
-
1. Bucx MJ, van Geel RT, Scheck PA, Stijnen T. Cardiovascular effects of forces applied during laryngoscopy. The importance of tracheal intubation. Anaesthesia. 1992; 47:1029–33. DOI: 10.1111/j.1365-2044.1992.tb04195.x. PMID: 1489023.2. Kim JS, Kim DH, Min SK, Kim KM, Kim JY. Comparison of effect-site concentration of remifentanil for tracheal intubation with the lightwand and laryngoscopy during propofol target-controlled infusion. Korean J Anesthesiol. 2011; 60:393–7. DOI: 10.4097/kjae.2011.60.6.393. PMID: 21738840. PMCID: PMC3121084.3. Ithnin F, Lim Y, Shah M, Shen L, Sia AT. Tracheal intubating conditions using propofol and remifentanil target-controlled infusion: a comparison of remifentanil EC50 for Glidescope and Macintosh. Eur J Anaesthesiol. 2009; 26:223–8. DOI: 10.1097/EJA.0b013e328324b4fc. PMID: 19237984.4. Takahashi S, Mizutani T, Miyabe M, Toyooka H. Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand intubating device (Trachlight) in adults with normal airway. Anesth Analg. 2002; 95:480–4. DOI: 10.1097/00000539-200208000-00046. PMID: 12145076.5. Nabecker S, Grubhofer G, Hager H, Goliasch G, Fischer H, Bernardi M, et al. Hemodynamic and humoral response to intubation with double-lumen endotracheal tubes versus single-lumen tubes combined with an endobronchial blocker: a randomized clinical trial. J Anesth Clin Res. 2014; 5:1–5. DOI: 10.4172/2155-6148.1000377.6. Shinn HK, Lee HS, Lee CS, Chung CK, Cha DC, Kim HH, et al. The effect-site concentration of remifentanil for prevention of increase of blood pressure and heart rate to tracheal intubation during propofol-remifentanil total intravenous anesthesia in Korean. Korean J Anesthesiol. 2006; 51:312–7. DOI: 10.4097/kjae.2006.51.3.312.7. Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, et al. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005; 101:125–30. DOI: 10.1213/01.ANE.0000153012.35120.FE. PMID: 15976218.8. Lee JH, Kim SI, Ok SY, Kim SC. Evaluation of effect-site concentration of remifentanil for blunting hemodynamic responses to endotracheal intubation during total intravenous anesthesia using propofol. Korean J Anesthesiol. 2007; 52:269–74. DOI: 10.4097/kjae.2007.52.3.269. DOI: 10.4097/kjae.2007.52.5.521.9. Jung YH, Lim YH, Kwon YS, Lee SS, Lee WY, Yon JH, et al. An analysis of correlation between remifentanil effect site concentration and age blunting hemodynamic response to endotracheal intubation. Anesth Pain Med. 2009; 4:113–7.10. Dixon WJ. Staircase bioassay: the up-and-down method. Neurosci Biobehav Rev. 1991; 15:47–50. DOI: 10.1016/S0149-7634(05)80090-9.11. Shin HY, Seo BB, Lee YC, Kim JM, Kim AR, Jang YH, et al. Optimal dose of remifentanil to attenuate cardiovascular responses to laryngoscopic double-lumen endobronchial intubation. Korean J Anesthesiol. 2007; 53:48–53. DOI: 10.4097/kjae.2007.53.1.48.12. Heo BH, Yoon MH, Lee HG, Kim WM. Effect-site concentration of remifentanil for blunting hemodynamic response to double lumen endobronchial intubation during target controlled infusion- total intravenous anesthesia using propofol with remifentanil. Korean J Anesthesiol. 2009; 57:8–12. DOI: 10.4097/kjae.2009.57.1.8.13. Yoo KY, Jeong CW, Kim WM, Lee HK, Jeong S, Kim SJ, et al. Cardiovascular and arousal responses to single-lumen endotracheal and double-lumen endobronchial intubation in the normotensive and hypertensive elderly. Korean J Anesthesiol. 2011; 60:90–7. DOI: 10.4097/kjae.2011.60.2.90. PMID: 21390163. PMCID: PMC3049888.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect-site concentration of remifentanil for blunting hemodynamic response to double lumen endobronchial intubation during target controlled infusion-total intravenous anesthesia using propofol with remifentanil
- Optimal Dose of Remifentanil to Attenuate Cardiovascular Responses to Laryngoscopic Double-lumen Endobronchial Intubation
- Effect-site concentration of remifentanil for blunting hemodynamic responses to tracheal intubation using light wand during target controlled infusion-total intravenous anesthesia
- Evaluation of Effect-site Concentration of Remifentanil for Blunting Hemodynamic Responses to Endotracheal Intubation during Total Intravenous Anesthesia using Propofol
- What is the Optimal Effect-site Concentration of Remifentanil for Minimizing the Cardiovascular Changes to Endotracheal Intubation during Induction with Propofol?