Ann Clin Neurophysiol.
2017 Jul;19(2):131-135. 10.14253/acn.2017.19.2.131.
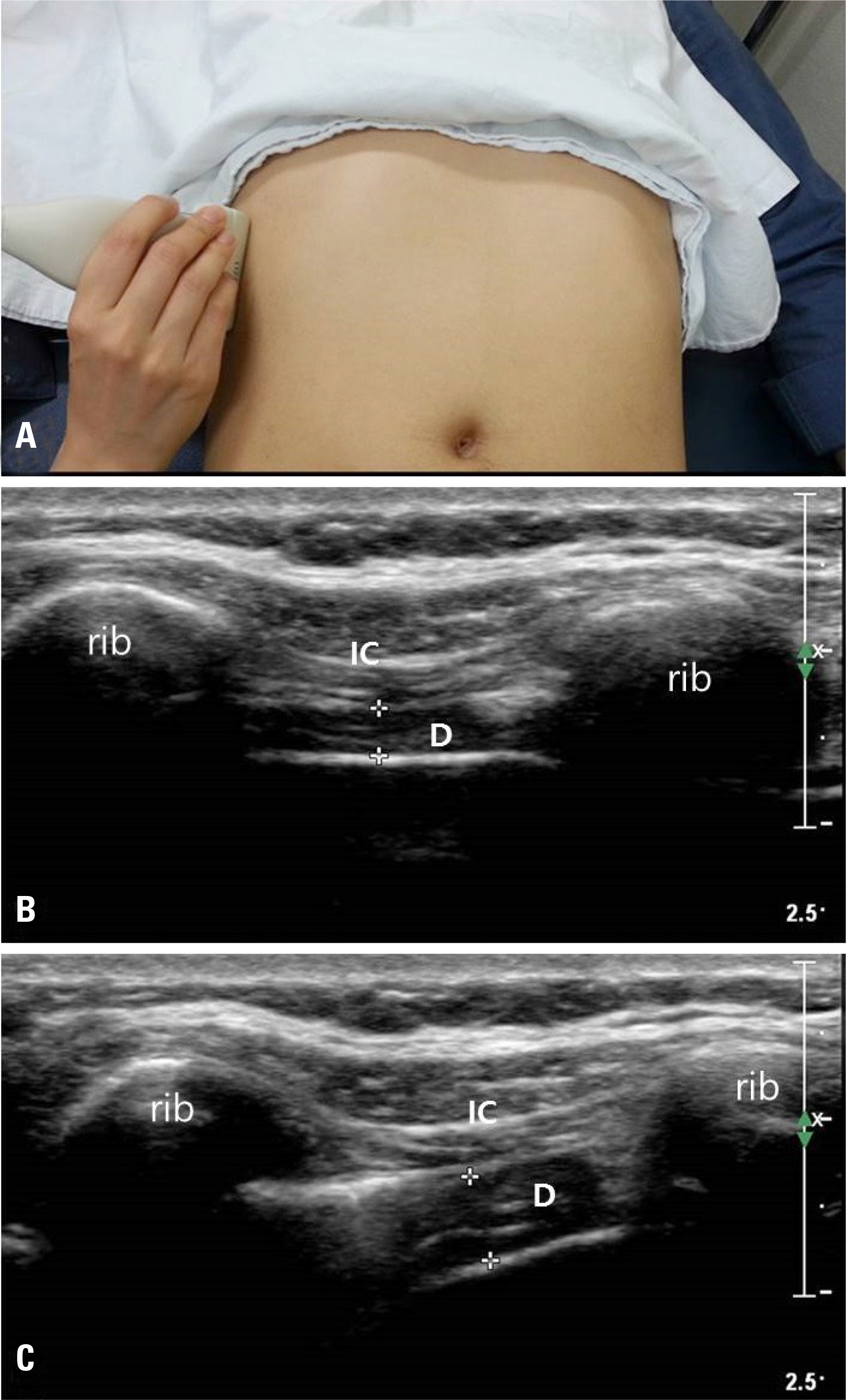
Ultrasonographic findings of the normal diaphragm: thickness and contractility
- Affiliations
-
- 1Department of Neurology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 2Department of Neurology, Wake Forest University School of Medicine, Winston-Salem, NC, USA. fwalker@wakehealth.edu
- 3Medical Statistics & Informatics, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 4Department of Neurology, CHA Gumi Medical Center, CHA University, Gumi, Korea.
- KMID: 2387234
- DOI: http://doi.org/10.14253/acn.2017.19.2.131
Abstract
- BACKGROUND
Neuromuscular ultrasound can be used to assess the diaphragm. Before it can be used clinically, the reference ranges of diaphragm thickness and contractility must be determined.
METHODS
We measured the thickness of the diaphragm and the diaphragmatic thickening fraction (DTF) in 80 healthy volunteers with ultrasound and collected their demographic information to determine if age, sex, and body mass index (BMI) influence these measures.
RESULTS
The thickness of the diaphragm at resting end expiration was 0.193 ± 0.044 cm on the right side and 0.187 ± 0.039 cm on the left. The DTF was 104.8 ± 50.6% on the right side and 114.9 ± 49.2% on the left. Sex, weight, height, and BMI significantly affected the thickness of the diaphragm, but had little effect on the DTF.
CONCLUSIONS
Normal reference values for the diaphragm should be helpful when evaluating the diaphragm. The DTF appears more useful than resting diaphragm thickness because it is affected less by individual variation.
Keyword
Figure
Cited by 2 articles
-
Is ultrasonography a main armament or just a supplement for evaluating patients with neuromuscular disorder?
Ye-Ji Kwon, Byung-Jo Kim
Ann Clin Neurophysiol. 2017;19(2):77-78. doi: 10.14253/acn.2017.19.2.77.Sonographic evaluation of the dia-phragm in patients with unilateral dia-phragmatic paralysis
Jung Im Seok, Kyung Chan Kim, Hye Joo Rha, Sung Rok Lee
Ann Clin Neurophysiol. 2018;20(2):93-96. doi: 10.14253/acn.2018.20.2.93.
Reference
-
1.McCool FD., Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med. 2012. 366:932–942.
Article2.Podgaetz E., Garza-Castillon R Jr., Andrade RS. Best approach and benefit of plication for paralyzed diaphragm. Thorac Surg Clin. 2016. 26:333–346.
Article3.Ko MA., Darling GE. Acquired paralysis of the diaphragm. Thorac Surg Clin. 2009. 19:501–510.
Article4.Sarwal A., Walker FO., Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013. 47:319–329.
Article5.Qureshi A. Diaphragm paralysis. Semin Respir Crit Care Med. 2009. 30:315–320.
Article6.Chetta A., Rehman AK., Moxham J., Carr DH., Polkey MI. Chest radiography cannot predict diaphragm function. Respir Med. 2005. 99:39–44.
Article7.Boon AJ., Alsharif KI., Harper CM., Smith J. Ultrasound-guided needle EMG of the diaphragm: technique description and case report. Muscle Nerve. 2008. 38:1623–1626.
Article8.Boon AJ., Harper CJ., Ghahfarokhi LS., Strommen JA., Watson JC., Sorenson EJ. Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve. 2013. 47:884–889.
Article9.Harper CJ., Shahgholi L., Cieslak K., Hellyer NJ., Strommen JA., Boon AJ. Variability in diaphragm motion during normal breathing, assessed with B-mode ultrasound. J Orthop Sports Phys Ther. 2013. 43:927–931.
Article10.Ueki J., De Bruin PF., Pride NB. In vivo assessment of diaphragm contraction by ultrasound in normal subjects. Thorax. 1995. 50:1157–1161.
Article11.Gottesman E., McCool FD. Ultrasound evaluation of the paralyzed diaphragm. Am J Respir Crit Care Med. 1997. 155:1570–1574.
Article12.Baldwin CE., Paratz JD., Bersten AD. Diaphragm and peripheral muscle thickness on ultrasound: intrarater reliability and variabil-ity of a methodology using non-standard recumbent positions. Respirology. 2011. 16:1136–1143.
Article13.De Bruin PF., Ueki J., Bush A., Khan Y., Watson A., Pride NB. Diaphragm thickness and inspiratory strength in patients with Duchenne muscular dystrophy. Thorax. 1997. 52:472–475.
Article14.Summerhill EM., El-Sameed YA., Glidden TJ., McCool FD. Monitor-ing recovery from diaphragm paralysis with ultrasound. Chest. 2008. 133:737–743.
Article15.Hellyer NJ., Andreas NM., Bernstetter AS., Cieslak KR., Donahue GF., Steiner EA, et al. Comparison of diaphragm thickness measure-ments among postures via ultrasound imaging. PM R. 2017. 9:21–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonographic evaluation of the diaphragm in patients with unilateral diaphragmatic paralysis
- Speckle tracking ultrasonography as a new tool to assess diaphragmatic function: a feasibility study
- Ultrasound Imaging of the Trunk Muscles in Acute Stroke Patients and Relations With Balance Scales
- Ultrasound Imaging of the Diaphragm
- Crura Sign: Differentiation between Traumatic Rupture of the Diaphragm and Nontraumatic Elevation on CT