J Korean Assoc Oral Maxillofac Surg.
2017 Jun;43(3):197-203. 10.5125/jkaoms.2017.43.3.197.
Modified drainage of submasseteric space abscess
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Wonkwang University, Iksan, Korea. omschoi@wonkwang.ac.kr
- 2Wonkwang Dental Research Institute, Wonkwang University, Iksan, Korea.
- KMID: 2386367
- DOI: http://doi.org/10.5125/jkaoms.2017.43.3.197
Abstract
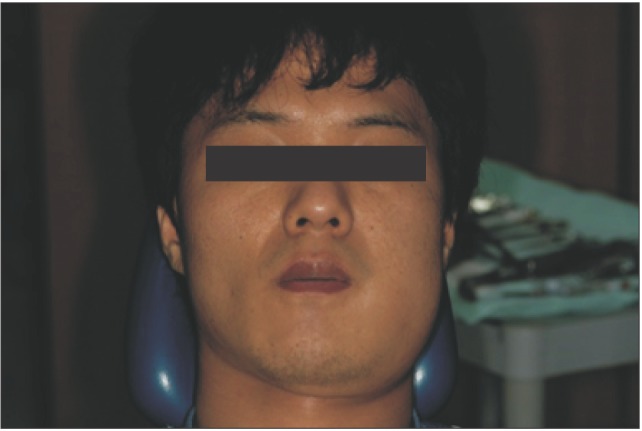
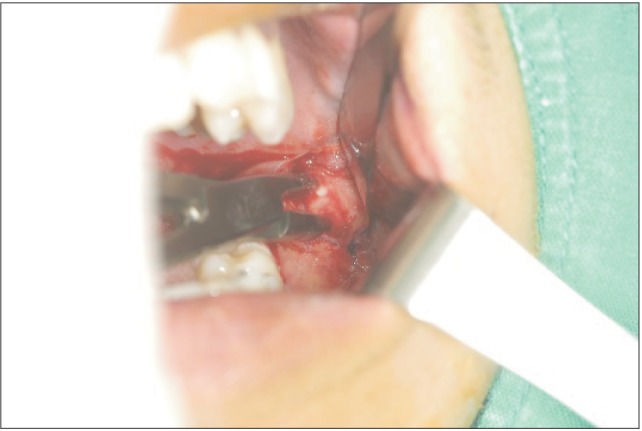
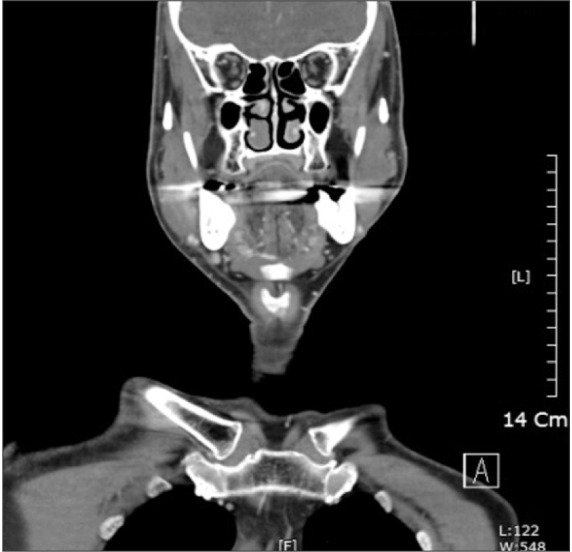
- Once a submasseteric space infection is diagnosed, the key to resolving the infection is via surgical intervention to evacuate the pus. Although it is possible and occasionally practical to drain the submasseteric space via an intraoral approach, an extraoral approach may sometimes be required. Surgeons have encountered complications such as facial nerve damage during extraoral incision and drainage procedures, and they have felt that extraoral dissection was very difficult. As such, an easier and simpler technique is needed. Our department recently modified various drainage techniques for submasseteric space abscesses. Damage to the marginal branch of the facial nerve did not occur, and this technique was very simple and rapid, such that a novice physician could perform this procedure. This modified technique was possible with trismus and under local anesthesia. After intraorally checking the position of the drain, the intraoral wound is closed with an absorbable suture and the drain is fixed to the extraoral skin. When a masseteric space infection is diagnosed, multiple space involvement is ruled out, and dependent drainage is required, this modified drainage technique can be useful.
MeSH Terms
Figure
Reference
-
1. Balatsouras DG, Kloutsos GM, Protopapas D, Korres S, Economou C. Submasseteric abscess. J Laryngol Otol. 2001; 115:68–70. PMID: 11233632.
Article2. Bransby-Zachary GM. The sub-masseteric space. Br Dent J. 1948; 84:10–13. PMID: 18900171.3. Mandel L. Submasseteric abscess caused by a dentigerous cyst mimicking a parotitis: report of two cases. J Oral Maxillofac Surg. 1997; 55:996–999. PMID: 9294513.
Article4. Mandel L. Diagnosing protracted submasseteric abscess: the role of computed tomography. J Am Dent Assoc. 1996; 127:1646–1650. PMID: 8952242.5. Kay LW, Killey HC. The surgical problem of submasseteric abscess. Br J Oral Surg. 1963; 1:55–62. PMID: 14090547.
Article6. Topazian RG, Goldberg MH. Oral and maxillofacial infections. 2nd ed. Philadelphia: WB Saunders;1987. p. 177–180.7. Peterson LJ, Indresano AT, Marciani RD, Roser SM. Principles of oral and maxillofacial surgery. 2nd ed. Philadelphia: Lippincott;1992. p. 177.8. Newman MH Jr, Emley WE. Chronic masticator space infection. Arch Otolaryngol. 1974; 99:128–131. PMID: 4809940.
Article9. Leu YS, Lee JC, Chang KC. Submasseteric abscess: report of two cases. Am J Otolaryngol. 2000; 21:281–283. PMID: 10937916.
Article10. Schuknecht B, Stergiou G, Graetz K. Masticator space abscess derived from odontogenic infection: imaging manifestation and pathways of extension depicted by CT and MR in 30 patients. Eur Radiol. 2008; 18:1972–1979. PMID: 18418606.
Article11. Haggerty CJ, Laughlin RM. Atlas of operative oral and maxillofacial surgery. New Delhi: Wiley Blackwell, William & Wilkins;2015. p. 69–70.12. Sicher H. Oral anatomy. St. Louis: Mosby;1965.13. Sayuti R, Baharudin A, Amran M. Submasseteric abscess: an unusal head and neck condition. Arch Orofac Sci. 2007; 2:59–60.