J Korean Soc Spine Surg.
2017 Jun;24(2):137-145. 10.4184/jkss.2017.24.2.137.
Delayed Vertebral Collapse in Osteoporotic Vertebral Compression Fractures: Risk Factors and Treatment Strategies
- Affiliations
-
- 1Department of Orthopedic Surgery, Graduate School, College of Medicine, Kyung Hee University, Seoul, Korea. superdave@hanmail.net
- KMID: 2385651
- DOI: http://doi.org/10.4184/jkss.2017.24.2.137
Abstract
- STUDY DESIGN: Literature review.
OBJECTIVES
To review the complications of osteoporotic vertebral compression fractures (OCFs) with regard to risk factors and treatment strategies. SUMMARY OF LITERATURE REVIEW: Understanding the complications and treatment methods of OCFs is important given their increasing prevalence.
MATERIALS AND METHODS
Review of the literature.
RESULTS
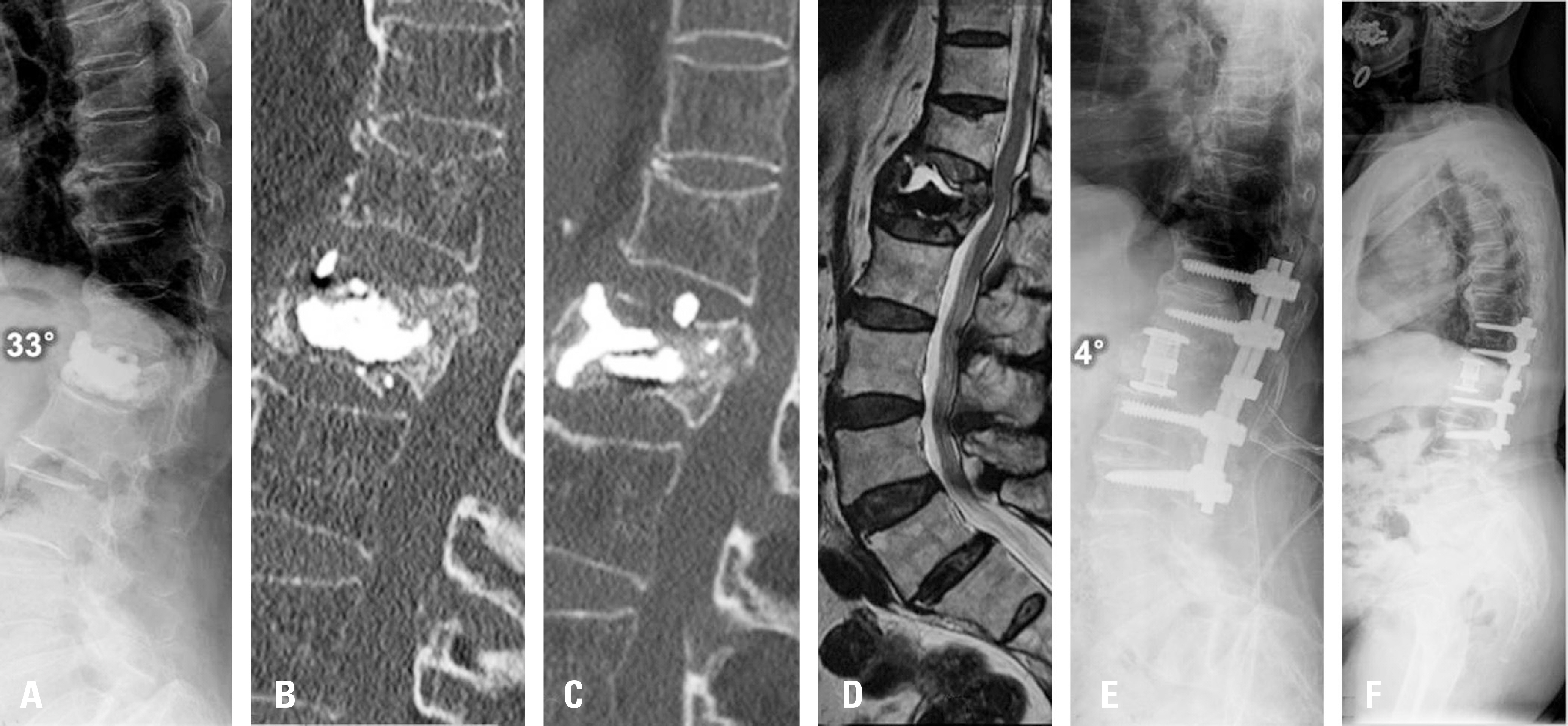
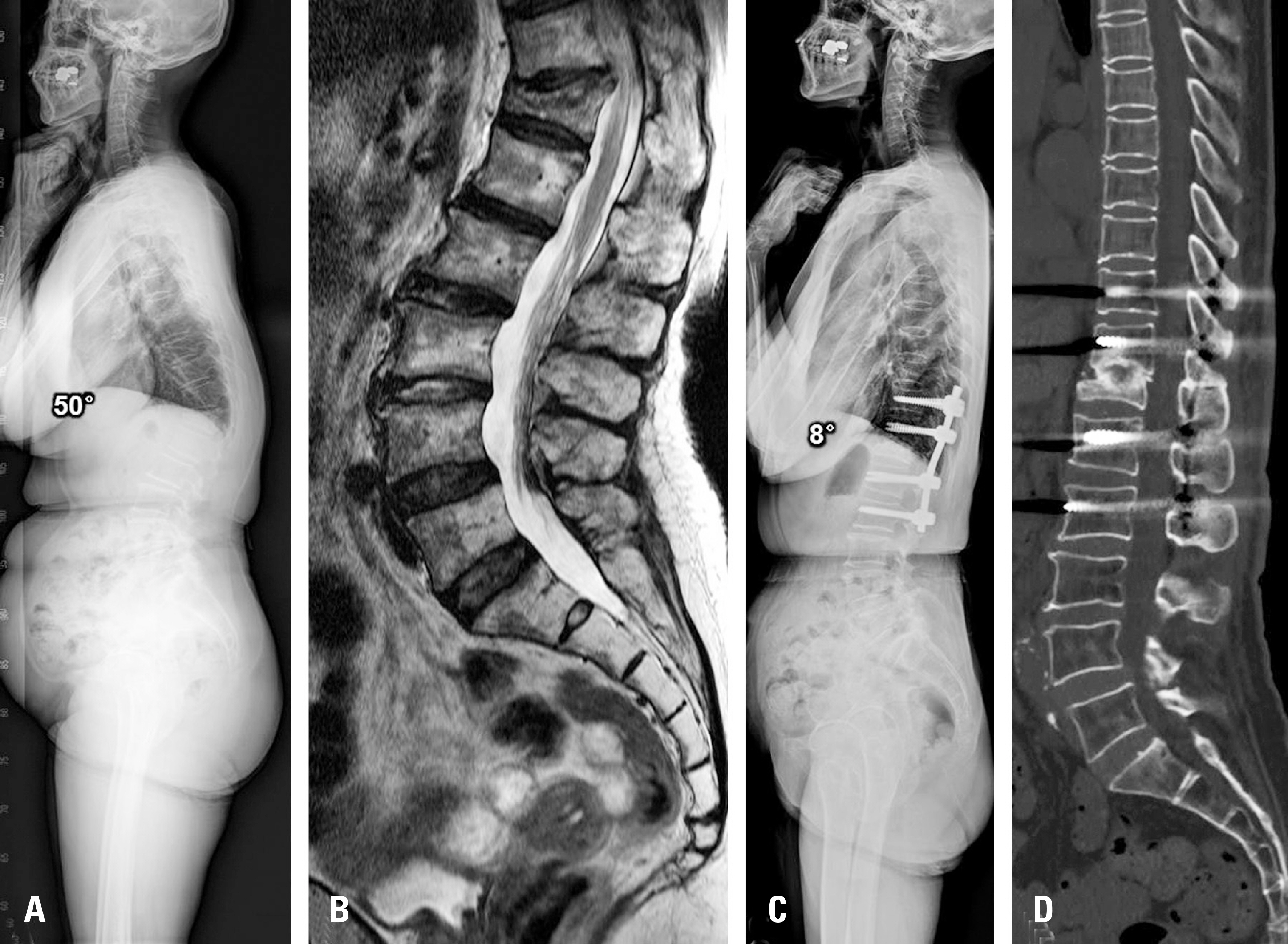
The complications of OCFs include kyphotic deformity due to a delayed collapse of the vertebral body and neurologic deficits. The pathophysiologic mechanism of these complications has not been established; however, the most accepted theory is posttraumatic avascular necrosis of the vertebral body. The risk factors for these complications include fracture at the thoracolumbar junction, systemic usage of steroids, severe osteoporosis, and radiological intravertebral vacuum cleft. Most of these complications require surgical treatment, the indications for which include progressing axial back pain, pseudarthrosis, kyphotic deformity, and neurologic deficits. Surgical approaches for treating the complications of OCFs include anterior, posterior, and combined anterior-posterior approaches. Osteotomies should be done when deformity correction is needed. The decision among these various surgical methods should be made considering patient factors and the surgeon's ability to achieve the best outcomes with solid fusion.
CONCLUSIONS
complications of OCFs include kyphotic deformity due to delayed collapse of the vertebral body and neurologic deficits. Most of these complications require surgical treatment, in which achieving solid fusion at the fracture site is the ultimate goal. Patient-related factors and the surgeon's ability should be considered prior to making decisions regarding surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Suk SI, Kim JH, Lee SM, et al. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine (Phila Pa 1976). 2003; 28:2170–5.
Article2. Kummell Hs. Der heutige Standpunkt der posttraumatisch-en Wir-belerkrankung(“Kummelshce Krankheit’). Arch Orthop Unfallchir. 1928; 26:471–502.3. Young WF, Brown D, Kendler A, et al. Delayed posttraumatic osteonecrosis of a vertebral body (Kummell's disease). Acta Orthop Belg. 2002; 68:13–9.4. Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978; 129:23–9.
Article5. Ito Y, Hasegawa Y, Toda K, et al. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002; 2:101–6.
Article6. Ha KY, Kim YH. Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int. 2013; 24:1207–13.
Article7. Hashidate H, Kamimura M, Nakagawa H, et al. Pseudoarthrosis of vertebral fracture: radiographic and characteristic clinical features and natural history. J Orthop Sci. 2006; 11:28–33.
Article8. Kanchiku T, Imajo Y, Suzuki H, et al. Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech. 2014; 27:E61–5.
Article9. Kumpan W, Salomonowitz E, Seidl G, et al. The intravertebral vacuum phenomenon. Skeletal Radiol. 1986; 15:444–7.
Article10. Kaneda K, Asano S, Hashimoto T, et al. The treatment of osteoporotic-posttraumatic vertebral collapse using the Kaneda device and a bioactive ceramic vertebral prosthesis. Spine (Phila Pa 1976). 1992; 17(Suppl):295–303.
Article11. Tsujio T, Nakamura H, Terai H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976). 2011; 36:1229–35.12. Sugita M, Watanabe N, Mikami Y, et al. Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech. 2005; 18:376–81.
Article13. Patil S, Nene AM. Predictors of kyphotic deformity in osteoporotic vertebral compression fractures: a radiological study. Eur Spine J. 2014; 23:2737–42.
Article14. Okuda S, Oda T, Miyauchi A, et al. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 2006; 88:2714–20.
Article15. Coe JD, Warden KE, Herzig MA, et al. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976). 1990; 15:902–7.
Article16. Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992; 17:528–40.17. Roberson JR, Whitesides TE Jr. Surgical reconstruction of late post-traumatic thoracolumbar kyphosis. Spine (Phila Pa 1976). 1985; 10:307–12.
Article18. Abel R, Gerner HJ, Smit C, et al. Residual deformity of the spinal canal in patients with traumatic paraplegia and secondary changes of the spinal cord. Spinal Cord. 1999; 37:14–9.
Article19. Arciero RA, Leung KY, Pierce JH. Spontaneous unstable burst fracture of the thoracolumbar spine in osteoporosis. A report of two cases. Spine (Phila Pa 1976). 1989; 14:114–7.20. Gurr KR, McAfee PC, Shih CM. Biomechanical analysis of anterior and posterior instrumentation systems after corpectomy. A calf-spine model. J Bone Joint Surg Am. 1988; 70:1182–91.
Article21. Royle ND. The operative removal of an accessory vertebra. Med J Aust. 1928; 1:467.
Article22. Capener N. The evolution of lateral rhachotomy. J Bone Joint Surg Br. 1954; 36:173–9.
Article23. Heinig CF. Eggshell procedure. Luque E, editor. editor.Segmental Spinal Instrumentation. New Jersey: Slack;1984. p. 221–34.24. Shikata J, Yamamuro T, Iida H, et al. Surgical treatment for paraplegia resulting from vertebral fractures in senile osteoporosis. Spine (Phila Pa 1976). 1990; 15:485–9.
Article25. Gertzbein SD, Harris MB. Wedge osteotomy for the correction of post-traumatic kyphosis. A new technique and a report of three cases. Spine (Phila Pa 1976). 1992; 17:374–9.26. Wu SS, Hwa SY, Lin LC, et al. Management of rigid post-traumatic kyphosis. Spine (Phila Pa 1976). 1996; 21:2260–6.
Article27. Lehmer SM, Keppler L, Biscup RS, et al. Posterior transver-tebral osteotomy for adult thoracolumbar kyphosis. Spine (Phila Pa 1976). 1994; 19:2060–7.
Article28. Streitz W, Brown JC, Bonnett CA. Anterior fibular strut grafting in the treatment of kyphosis. Clin Orthop Relat Res. 1977. 140–8.
Article29. Malcolm BW, Bradford DS, Winter RB, et al. Post-trau-matic kyphosis. A review of forty-eight surgically treated patients. J Bone Joint Surg Am. 1981; 63:891–9.
Article30. Lee JH, Oh HS, Choi JG. Comparison of the Posterior Vertebral Column Resection with the Expandable Cage versus the Nonexpandable Cage in Thoracolumbar Angular Kyphosis. Clin Spine Surg. 2016 Jun 28. [Epub ahead of print].
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posttraumatic Delayed Vertebral Collapse : Kummell's Disease
- Prediction of Subsequent Vertebral Collapse after Osteoporotic Thoracolumbar Vertebral Fractures
- The Diagnosis of Osteoporotic Occult Vertebral Fracture and Vertebroplasty
- Radiographic Diagnosis of the Osteoporotic Vertebral Fractures
- Association Between Osteoporotic Vertebral Fracture and Body Mass Index