J Endocr Surg.
2017 Jun;17(2):80-88. 10.16956/jes.2017.17.2.80.
Staging of Differentiated Thyroid Cancer from a Single Institution: Comparison of the 7th and 8th Editions of AJCC/UICC Staging
- Affiliations
-
- 1Department of Surgery, The Catholic University of Korea College of Medicine, Seoul St. Mary's Hospital, Seoul, Korea. leesohee@catholic.ac.kr
- KMID: 2383825
- DOI: http://doi.org/10.16956/jes.2017.17.2.80
Abstract
- PURPOSE
Traditional clinicopathological variables are used to predict prognosis in differentiated thyroid cancer, including age at diagnosis, tumor size, and extrathyroidal extension (ETE). The American Joint Committee on Cancer/Union for International Cancer Control (AJCC/UICC) 8th edition for thyroid cancer was released in 2016 and included major revisions regarding tumor, node, and metastasis (TNM) stages, resulting in significant stage migration. The aim of our study was to describe this stage migration of the 7th and 8th editions of the AJCC/UICC staging system using a cohort of differentiated thyroid cancer patients from a single institution.
METHODS
We reviewed 2,447 patients who underwent thyroidectomy between September 2008 and December 2011. Of these, the complete medical records of 2,234 differentiated thyroid cancer patients were retrospectively included in the study. TNM stage was analyzed using the 7th and 8th editions of the AJCC/UICC staging system.
RESULTS
TNM stage showed notable changes owing to changes in age cutoff point, and the definitions of ETE and N0. Upon reclassification, 835 patients of T3 were downgraded to T1 and T2, resulting in increased numbers of T1 and T2 patients (49.3% to 85.0% and 1.3% to 3.0%, respectively). Reclassification of nodal stage resulted in 191 cases (8.6%) of NX, according the 7th edition, to be re-categorized into N0; therefore, N0 cases increased from 49.5% to 58.1%. Additionally, stage I and II tumor cases increased from 60.6% to 89.3%, and 0.2% to 9.8%, respectively, and stage III and IV cases showed corresponding decreases from 28.2% to 0.9%, and 5.4% to 0.1%, respectively.
CONCLUSION
Staging of differentiated thyroid cancer cases using the AJCC/UICC staging system 8th edition results in marked TNM staging migration in the direction of downstaging.
Keyword
MeSH Terms
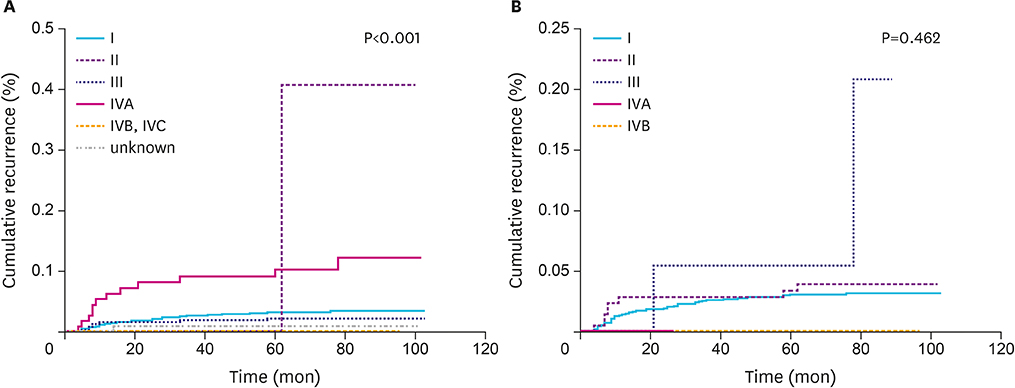
Figure
Reference
-
1. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014; 140:317–322.
Article2. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017; 317:1338–1348.
Article3. Momesso DP, Tuttle RM. Update on differentiated thyroid cancer staging. Endocrinol Metab Clin North Am. 2014; 43:401–421.
Article4. Schemper M, Stare J. Explained variation in survival analysis. Stat Med. 1996; 15:1999–2012.
Article5. Vrachimis A, Gerss J, Stoyke M, Wittekind C, Maier T, Wenning C, et al. No significant difference in the prognostic value of the 5th and 7th editions of AJCC staging for differentiated thyroid cancer. Clin Endocrinol (Oxf). 2014; 80:911–917.
Article6. Singer PA, Cooper DS, Daniels GH, Ladenson PW, Greenspan FS, Levy EG, et al. Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Arch Intern Med. 1996; 156:2165–2172.
Article7. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.8. Compton CC, Byrd DR, Garcia-Aguilar J, Kurtzman SH, Olawaiye A, Washington MK. AJCC Cancer Staging Atlas: a Companion to the Seventh Editions of the AJCC Cancer Staging Manual and Handbook. 2nd ed. New York (NY): Springer;2012.9. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer Staging Manual. 8th ed. New York (NY): Springer;2016.10. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.
Article11. Nixon IJ, Kuk D, Wreesmann V, Morris L, Palmer FL, Ganly I, et al. Defining a valid age cutoff in staging of well-differentiated thyroid cancer. Ann Surg Oncol. 2016; 23:410–415.
Article12. Ganly I, Nixon IJ, Wang LY, Palmer FL, Migliacci JC, Aniss A, et al. Survival from differentiated thyroid cancer: what has age got to do with it? Thyroid. 2015; 25:1106–1114.
Article13. Oyer SL, Smith VA, Lentsch EJ. Reevaluating the prognostic significance of age in differentiated thyroid cancer. Otolaryngol Head Neck Surg. 2012; 147:221–226.
Article14. Hendrickson-Rebizant J, Sigvaldason H, Nason RW, Pathak KA. Identifying the most appropriate age threshold for TNM stage grouping of well-differentiated thyroid cancer. Eur J Surg Oncol. 2015; 41:1028–1032.
Article15. Kim SJ, Myong JP, Suh H, Lee KE, Youn YK. Optimal cutoff age for predicting mortality associated with differentiated thyroid cancer. PLoS One. 2015; 10:e0130848.
Article16. Mazurat A, Torroni A, Hendrickson-Rebizant J, Benning H, Nason RW, Pathak KA. The age factor in survival of a population cohort of well-differentiated thyroid cancer. Endocr Connect. 2013; 2:154–160.
Article17. National Cancer Information Center (KR). Cancer statistics [Internet]. Goyang: National Cancer Center;2016. cited 2017 Jun 3. Available from: http://www.cancer.go.kr/mbs/cancer/.18. Arora N, Turbendian HK, Scognamiglio T, Wagner PL, Goldsmith SJ, Zarnegar R, et al. Extrathyroidal extension is not all equal: Implications of macroscopic versus microscopic extent in papillary thyroid carcinoma. Surgery. 2008; 144:942–947.
Article19. Radowsky JS, Howard RS, Burch HB, Stojadinovic A. Impact of degree of extrathyroidal extension of disease on papillary thyroid cancer outcome. Thyroid. 2014; 24:241–244.
Article20. Woo CG, Sung CO, Choi YM, Kim WG, Kim TY, Shong YK, et al. Clinicopathological significance of minimal extrathyroid extension in solitary papillary thyroid carcinomas. Ann Surg Oncol. 2015; 22:Suppl 3. S728–S733.
Article21. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006; 295:2164–2167.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Differences in Survival Rates between the 7th and 8th Editions of the AJCC TNM Staging System for Gastric Adenocarcinoma: a Single-Institution Study of 5,507 Patients in Korea
- Assessment of the Prognostic Staging System of American Joint Committee on Cancer 8th Edition for Breast Cancer: Comparisons with the Conventional Anatomic Staging System
- Prognostic Predictability of American Joint Committee on Cancer 8th Staging System for Perihilar Cholangiocarcinoma: Limited Improvement Compared with the 7th Staging System
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- Does the New UICC/AJCC TNM Staging System (7th Edition) Improve Assessing Prognosis in Gastric Cancer Compared to the Old System (6th Edition)?