Ann Rehabil Med.
2017 Feb;41(1):104-112. 10.5535/arm.2017.41.1.104.
Therapeutic Effect of Microcurrent Therapy in Children With In-toeing Gait Caused by Increased Femoral Anteversion: A Pilot Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea.
- 2Department of Rehabilitation Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. cateyesn@naver.com
- KMID: 2383684
- DOI: http://doi.org/10.5535/arm.2017.41.1.104
Abstract
OBJECTIVE
To investigate the efficacy of portable microcurrent therapy device (PMTD) of the hip internal rotators in the treatment of in-toeing gait caused by increased femoral anteversion in children over 8 years of age.
METHODS
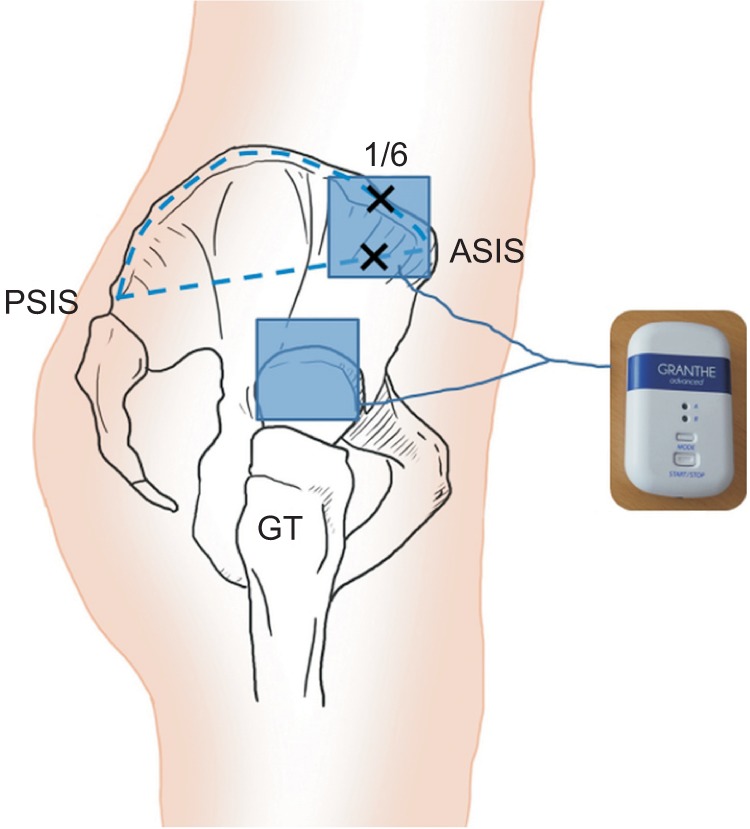
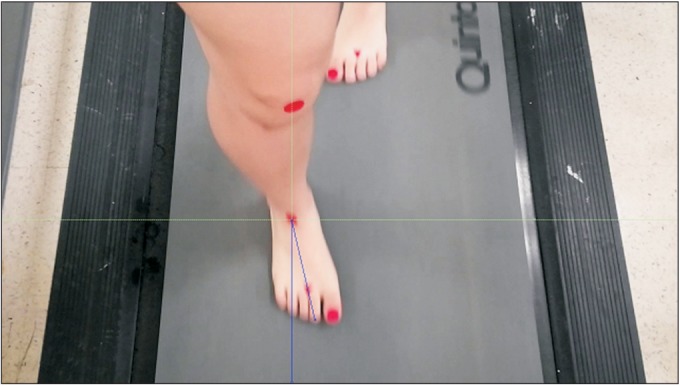
Eleven children (22 legs; 4 boys and 7 girls; mean age, 10.4±1.6 years) with in-toeing gait caused by increased femoral anteversion were included in the present study. All children received 60 minutes of PMTD (intensity, 25 µA; frequency, 8 Hz) applied to the hip internal rotators daily for 4 weeks. Hip internal rotation (IR) angle, external rotation (ER) angle, and midmalleolar-second toe angle (MSTA) measurement during stance phase at transverse plane and Family Satisfaction Questionnaire, frequency of tripping and fatigue like pains about the PMTD were performed before treatment and at 4 weeks after initial PMTD treatment. Paired t-test and Fisher exact test were used for statistical analysis.
RESULTS
Hip IR/ER/MSTA was 70.3°±5.4°/20.1°±5.5°/-11.4°±2.7°, and 55.7°±7.8°/33.6°±8.2°/-2.6°±3.8° before treatment and at 4 weeks after initial PMTD treatment, respectively (p<0.01). Ten of 11 (91%) children's family stated that they were generally satisfied with the PMTD treatment. The frequency of tripping and fatigue like pains was significantly lower at 4 weeks after PMTD treatment (p<0.05). Excellent inter-rater and intra-rater reliability was observed for repeated MSTA measurements between the examiners (k=0.91-0.96 and k=0.93-0.99), respectively.
CONCLUSION
PMTD of the hip internal rotators can be effective in improving the gait pattern of children with in-toeing gait caused by increased femoral anteversion.
MeSH Terms
Figure
Cited by 1 articles
-
Toe-in Gait, Associated Complications, and Available Conservative Treatments: A Systematic Review of Literature
Mohammad Taghi Karimi
J Korean Foot Ankle Soc. 2023;27(1):17-23. doi: 10.14193/jkfas.2023.27.1.17.
Reference
-
1. Thackeray C, Beeson P. Is in-toeing gait a developmental stage? Foot. 1996; 6:19–24.
Article2. Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children: normal values to guide management. J Bone Joint Surg Am. 1985; 67:39–47. PMID: 3968103.
Article3. Winter WG Jr, Lafferty JF. The skiing sequelae of tibial torsion. Orthop Clin North Am. 1976; 7:231–240. PMID: 1256791.
Article4. Staheli LT. Torsion: treatment indications. Clin Orthop Relat Res. 1989; (247):61–66.5. Crane L. Femoral torsion and its relation to toeing-in and toeing-out. J Bone Joint Surg Am. 1959; 41-A:421–428. PMID: 13641293.
Article6. Munuera PV, Castillo JM, Dominguez G, Lafuente G. Orthotic devices with out-toeing wedge as treatment for in-toed gait in children. J Am Podiatr Med Assoc. 2010; 100:472–478. PMID: 21084533.
Article7. Fabry G, MacEwen GD, Shands AR Jr. Torsion of the femur: a follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. 1973; 55:1726–1738. PMID: 4804993.8. Rethlefsen SA, Healy BS, Wren TA, Skaggs DL, Kay RM. Causes of intoeing gait in children with cerebral palsy. J Bone Joint Surg Am. 2006; 88:2175–2180. PMID: 17015594.
Article9. LeVeau BF, Bernhardt DB. Developmental biomechanics: effect of forces on the growth, development, and maintenance of the human body. Phys Ther. 1984; 64:1874–1882. PMID: 6505032.10. Chadayammuri V, Garabekyan T, Bedi A, Pascual-Garrido C, Rhodes J, O'Hara J, et al. Passive hip range of motion predicts femoral torsion and acetabular version. J Bone Joint Surg Am. 2016; 98:127–134. PMID: 26791033.
Article11. Salter RB. Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. J Bone Joint Surg Am. 1966; 48:1413–1439. PMID: 5921797.
Article12. Staheli LT, Duncan WR, Schaefer E. Growth alterations in the hemiplegic child: a study of femoral anteversion, neck-shaft angle, hip rotation, C.E. angle, limb length and circumference in 50 hemiplegic children. Clin Orthop Relat Res. 1968; 60:205–212. PMID: 5703292.13. Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine. 1998; 23:1009–1015. PMID: 9589539.
Article14. Gelberman RH, Cohen MS, Desai SS, Griffin PP, Salamon PB, O'Brien TM. Femoral anteversion: a clinical assessment of idiopathic intoeing gait in children. J Bone Joint Surg Br. 1987; 69:75–79. PMID: 3818738.
Article15. Svenningsen S, Terjesen T, Auflem M, Berg V. Hip rotation and in-toeing gait: a study of normal subjects from four years until adult age. Clin Orthop Relat Res. 1990; (251):177–182.16. Fabry G, Cheng LX, Molenaers G. Normal and abnormal torsional development in children. Clin Orthop Relat Res. 1994; (302):22–26.
Article17. Uden H, Kumar S. Non-surgical management of a pediatric “intoed” gait pattern: a systematic review of the current best evidence. J Multidiscip Healthc. 2012; 5:27–35. PMID: 22328828.18. Cibulka MT. Determination and significance of femoral neck anteversion. Phys Ther. 2004; 84:550–558. PMID: 15161420.
Article19. Maenpaa H, Jaakkola R, Sandstrom M, Von Wendt L. Does microcurrent stimulation increase the range of movement of ankle dorsiflexion in children with cerebral palsy? Disabil Rehabil. 2004; 26:669–677. PMID: 15204506.20. Byl NN, McKenzie AL, West JM, Whitney JD, Hunt TK, Hopf HW, et al. Pulsed microamperage stimulation: a controlled study of healing of surgically induced wounds in Yucatan pigs. Phys Ther. 1994; 74:201–213. PMID: 8115454.
Article21. Kim MY, Kwon DR, Lee HI. Therapeutic effect of microcurrent therapy in infants with congenital muscular torticollis. PM R. 2009; 1:736–739. PMID: 19695526.
Article22. Kwon DR, Park GY. Efficacy of microcurrent therapy in infants with congenital muscular torticollis involving the entire sternocleidomastoid muscle: a randomized placebo-controlled trial. Clin Rehabil. 2014; 28:983–991. PMID: 24240061.
Article23. Shah SB, Peters D, Jordan KA, Milner DJ, Friden J, Capetanaki Y, et al. Sarcomere number regulation maintained after immobilization in desmin-null mouse skeletal muscle. J Exp Biol. 2001; 204:1703–1710. PMID: 11316490.
Article24. Clarren SK. Plagiocephaly and torticollis: etiology, natural history, and helmet treatment. J Pediatr. 1981; 98:92–95. PMID: 7452415.
Article25. Kim HD, Lee DS, Eom MJ, Hwang JS, Han NM, Jo GY. Relationship between physical examinations and two-dimensional computed tomographic findings in children with intoeing gait. Ann Rehabil Med. 2011; 35:491–498. PMID: 22506164.
Article26. Semciw AI, Green RA, Pizzari T, Briggs C. Verification of a standardized method for inserting intramuscular EMG electrodes into uniquely oriented segments of gluteus minimus and gluteus medius. Clin Anat. 2013; 26:244–252. PMID: 22374796.
Article27. Inan M, Altintaş F, Duru I. The evaluation and management of rotational deformity in cerebral palsy. Acta Orthop Traumatol Turc. 2009; 43:106–112. PMID: 19448350.
Article28. Li YH, Leong JC. Intoeing gait in children. Hong Kong Med J. 1999; 5:360–366. PMID: 10870163.29. Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009; 43:417–422. PMID: 19372088.
Article30. Kolber MJ, Hanney WJ. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. Int J Sports Phys Ther. 2012; 7:306–313. PMID: 22666645.31. Gordon AM, Huxley AF, Julian FJ. The variation in isometric tension with sarcomere length in vertebrate muscle fibres. J Physiol. 1966; 184:170–192. PMID: 5921536.
Article32. Akai M, Shirasaki Y, Tateishi T. Electrical stimulation on joint contracture: an experiment in rat model with direct current. Arch Phys Med Rehabil. 1997; 78:405–409. PMID: 9111461.
Article33. Gibson JN, Smith K, Rennie MJ. Prevention of disuse muscle atrophy by means of electrical stimulation: maintenance of protein synthesis. Lancet. 1988; 2:767–770. PMID: 2901612.
Article34. Cheng N, Van Hoof H, Bockx E, Hoogmartens MJ, Mulier JC, De Dijcker FJ, et al. The effects of electric currents on ATP generation, protein synthesis, and membrane transport of rat skin. Clin Orthop Relat Res. 1982; (171):264–272.35. Farmer SE, James M. Contractures in orthopaedic and neurological conditions: a review of causes and treatment. Disabil Rehabil. 2001; 23:549–558. PMID: 11451189.36. Akki A, Yang H, Gupta A, Chacko VP, Yano T, Leppo MK, et al. Skeletal muscle ATP kinetics are impaired in frail mice. Age. 2014; 36:21–30. PMID: 23695949.
Article37. Fleischli JG, Laughlin TJ. Electrical stimulation in wound healing. J Foot Ankle Surg. 1997; 36:457–461. PMID: 9430002.
Article38. Brown MD, Cotter MA, Hudlicka O, Vrbova G. The effects of different patterns of muscle activity on capillary density, mechanical properties and structure of slow and fast rabbit muscles. Pflugers Arch. 1976; 361:241–250. PMID: 943767.
Article39. Losel S, Burgess-Milliron MJ, Micheli LJ, Edington CJ. A simplified technique for determining foot progression angle in children 4 to 16 years of age. J Pediatr Orthop. 1996; 16:570–574. PMID: 8865038.40. Milliron M, Loesel S, Micheli L, Edington C. Comparison of methods for calculation of foot progression angle: 1036. Med Sci Sports Exerc. 1992; 24(5 Suppl):S173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Femoral Anteversion and Tibial Torsion in Intoeing Gait
- Gait Patterns According to the Torsional Deformities in Spastic Hemiplegia: A Preliminary Report
- Change of Femoral Anteversion Angle in Children With Intoeing Gait Measured by Three-Dimensional Computed Tomography Reconstruction: 3-Year Follow-Up Study
- Gait Patterns According to the Transverse Plane Deformities in Spastic Diplegia: A Preliminary Report
- Relationship between Physical Examinations and Two-Dimensional Computed Tomographic Findings in Children with Intoeing Gait