Korean J Gastroenterol.
2016 Feb;67(2):116-118. 10.4166/kjg.2016.67.2.116.
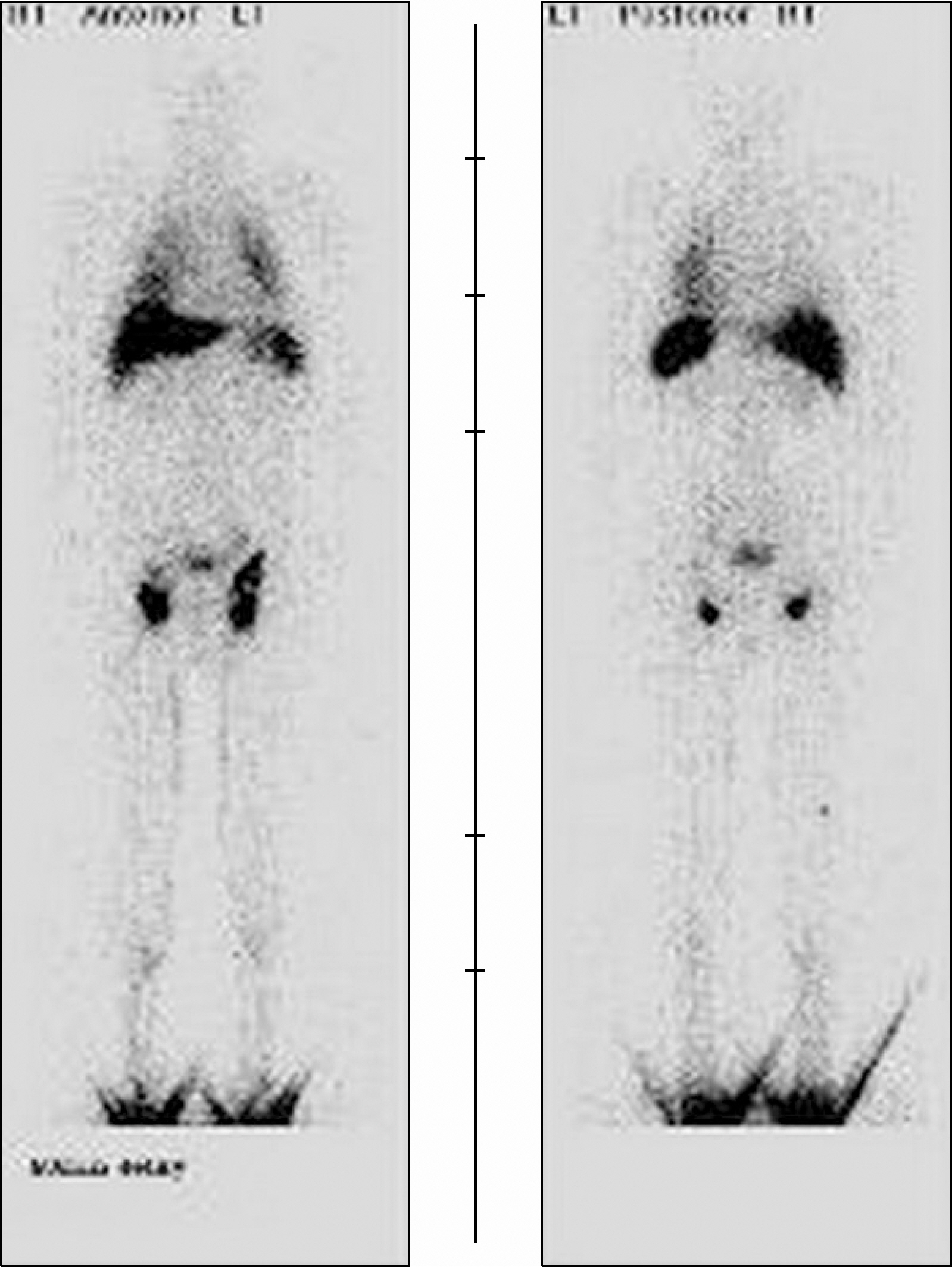
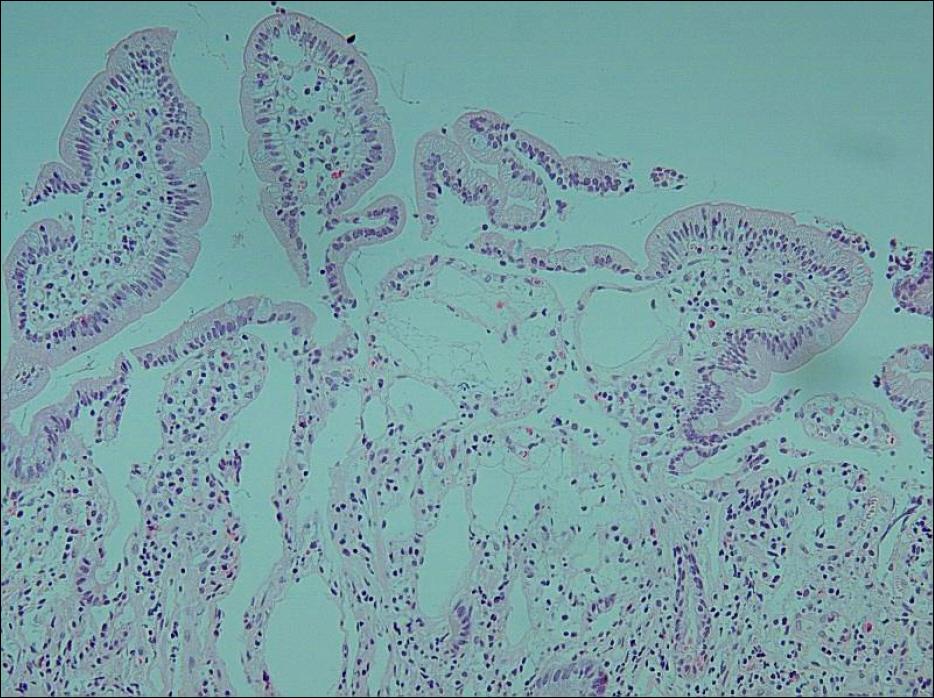
Primary Intestinal Lymphangiectasia Diagnosed by Chylous Ascites
- Affiliations
-
- 1Department of Internal Medicine, Eulji University School of Medicine, Seoul, Korea. cyk@eulji.ac.kr
- 2Department of Radiology, Eulji University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Eulji University School of Medicine, Seoul, Korea.
- KMID: 2383552
- DOI: http://doi.org/10.4166/kjg.2016.67.2.116
Abstract
- No abstract available.
Figure
Reference
-
References
1. Wen J, Tang Q, Wu J, Wang Y, Cai W. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010; 55:3466–3472.
Article2. Vignes S, Bellanger J. Primary intestinal lymphangiectasia (Waldmann's disease). Orphanet J Rare Dis. 2008; 3:5.
Article3. Umar SB, DiBaise JK. Protein-losing enteropathy: case illus-trations and clinical review. Am J Gastroenterol. 2010; 105:43–49.
Article4. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011; 3:235–240.
Article5. Rao R, Shashidhar H. Intestinal lymphangiectasia presenting as abdominal mass. Gastrointest Endosc. 2007; 65:522–523.
Article6. Maamer AB, Baazaoui J, Zaafouri H, Soualah W, Cherif A. Primary intestinal lymphangiectasia or Waldmann's disease: a rare cause of lower gastrointestinal bleeding. Arab J Gastroenterol. 2012; 13:97–98.
Article7. Imbesi V, Ciccocioppo R, Corazza GR. Long-standing intestinal lymphangiectasia detected by double-balloon enteroscopy. Clin Gastroenterol Hepatol. 2011; 9:e88–e89.
Article8. Chamouard P, Nehme-Schuster H, Simler JM, Finck G, Baumann R, Pasquali JL. Videocapsule endoscopy is useful for the diagnosis of intestinal lymphangiectasia. Dig Liver Dis. 2006; 38:699–703.
Article9. Filik L, Oguz P, Koksal A, Koklu S, Sahin B. A case with intestinal lymphangiectasia successfully treated with slow-release octreotide. Dig Liver Dis. 2004; 36:687–690.
Article10. Suehiro K, Morikage N, Murakami M, Yamashita O, Hamano K. Late-onset primary intestinal lymphangiectasia successfully managed with octreotide: a case report. Ann Vasc Dis. 2012; 5:96–99.
Article11. Zhu LH, Cai XJ, Mou YP, Zhu YP, Wang SB, Wu JG. Partial enter-ectomy: treatment for primary intestinal lymphangiectasia in four cases. Chin Med J (Engl). 2010; 123:760–764.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Intestinal Lymphangiectasia
- A Case of Primary Intestinal Lymphangiectasia Diagnosed by Double Balloon Enteroscopy
- The Update of Treatment for Primary Intestinal Lymphangiectasia
- A case of persistent chylous ascites after staging operation for primary fallopian tubal cancer
- Chylous Ascites Following Bariatric Surgery Report of Two Cases