Clin Endosc.
2017 Jan;50(1):51-57. 10.5946/ce.2016.015.
Correlation of Endoscopic Findings of Gastric Mucosa-Associated Lymphoid Tissue Lymphoma with Recurrence after Complete Remission
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. dhljohn@snubh.org
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2383490
- DOI: http://doi.org/10.5946/ce.2016.015
Abstract
- BACKGROUND/AIMS
In gastric mucosa-associated lymphoid tissue (MALT) lymphoma, the clinical significance of various endoscopic findings has not yet been determined. This study aimed to compare the time to complete remission (CR) and relapse-free survival (RFS) in gastric MALT lymphoma based on endoscopic findings.
METHODS
In this single-center retrospective cohort study, the medical records of 122 consecutive adult patients with gastric MALT lymphoma were collected over a period of 12 years. CR was defined by the absence of macroscopic or microscopic features of lymphoma on two subsequent follow-ups. Relapse was clinically defined by a positive endoscopic biopsy after CR.
RESULTS
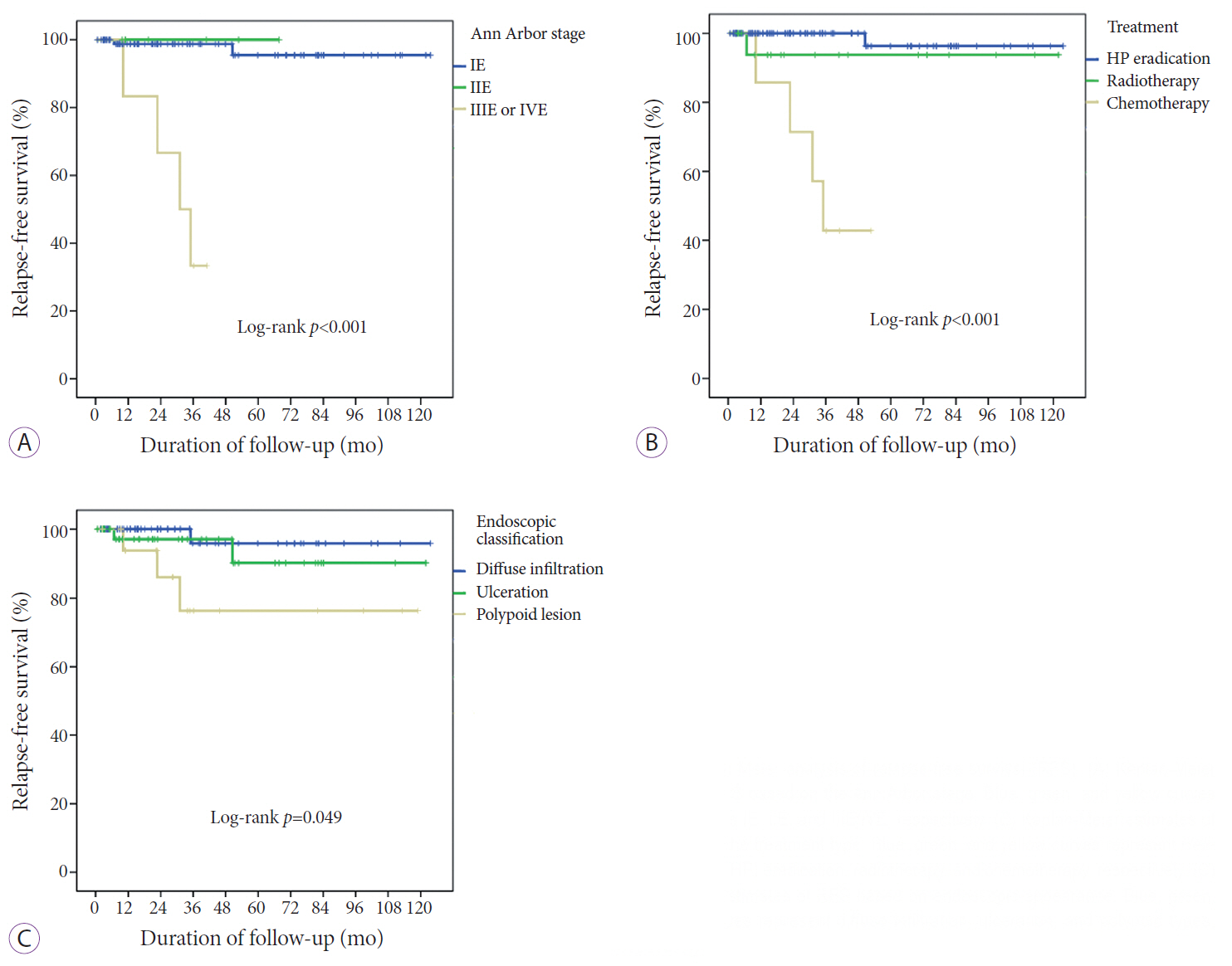
The median time to CR did not differ significantly between treatment methods. However, it was significantly longer in the group with polypoid endoscopic appearance than in the groups with diffuse infiltration or ulceration (7.83, 3.43, and 3.10 months, respectively; p=0.003). Six patients relapsed after CR. Kaplan-Meier analysis showed that RFS differed significantly between groups based on Ann Arbor staging, treatment methods, and initial endoscopic findings.
CONCLUSIONS
In gastric MALT lymphoma, the endoscopically defined polypoid type was characterized by a longer duration to CR, with a higher likelihood of recurrence, compared to the endoscopically defined diffuse infiltration or ulceration types.
MeSH Terms
Figure
Cited by 2 articles
-
Gastric Mucosa-associated Lymphoid Tissue Lymphoma Based on Outcome of Domestic Treatment
Jin Tae Jung
Korean J Gastroenterol. 2016;68(4):175-178. doi: 10.4166/kjg.2016.68.4.175.Endoscopic Findings of Gastric Extranodal Marginal Zone B-Cell Mucosa-Associated Lymphoid Tissue Lymphoma
Sang Kil Lee
Clin Endosc. 2017;50(1):1-2. doi: 10.5946/ce.2017.014.
Reference
-
1. Ruskoné-Fourmestraux A, Fischbach W, Aleman BM, et al. EGILS consensus report. Gastric extranodal marginal zone B-cell lymphoma of MALT. Gut. 2011; 60:747–758.
Article2. Zucca E, Copie-Bergman C, Ricardi U, et al. Gastric marginal zone lymphoma of MALT type: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24 Suppl 6:vi144–vi148.
Article3. Dreyling M, Thieblemont C, Gallamini A, et al. ESMO consensus conferences: guidelines on malignant lymphoma. Part 2: marginal zone lymphoma, mantle cell lymphoma, peripheral T-cell lymphoma. Ann Oncol. 2013; 24:857–877.
Article4. Zullo A, Hassan C, Cristofari F, et al. Effects of Helicobacter pylori eradication on early stage gastric mucosa-associated lymphoid tissue lymphoma. Clin Gastroenterol Hepatol. 2010; 8:105–110.
Article5. Isaacson PG. Gastric MALT lymphoma: from concept to cure. Ann Oncol. 1999; 10:637–645.
Article6. Sackmann M, Morgner A, Rudolph B, et al. Regression of gastric MALT lymphoma after eradication of Helicobacter pylori is predicted by endosonographic staging. MALT Lymphoma Study Group. Gastroenterology. 1997; 113:1087–1090.
Article7. Kim SJ, Yang S, Min BH, et al. Helicobacter pylori eradication for stage I(E1) gastric mucosa-associated lymphoid tissue lymphoma: predictive factors of complete remission. Korean J Gastroenterol. 2010; 55:94–99.8. Ryu KD, Kim GH, Park SO, et al. Treatment outcome for gastric mucosa-associated lymphoid tissue lymphoma according to Helicobacter pylori infection status: a single-center experience. Gut Liver. 2014; 8:408–414.9. Suzuki H, Saito Y, Hibi T. Helicobacter pylori and gastric mucosa-associated lymphoid tissue (MALT) lymphoma: updated review of clinical outcomes and the molecular pathogenesis. Gut Liver. 2009; 3:81–87.
Article10. Radaszkiewicz T, Dragosics B, Bauer P. Gastrointestinal malignant lymphomas of the mucosa-associated lymphoid tissue: factors relevant to prognosis. Gastroenterology. 1992; 102:1628–1638.
Article11. Pinotti G, Zucca E, Roggero E, et al. Clinical features, treatment and outcome in a series of 93 patients with low-grade gastric MALT lymphoma. Leuk Lymphoma. 1997; 26:527–537.
Article12. Taal BG, den Hartog Jager FC, Tytgat GN. The endoscopic spectrum of primary non-Hodgkin’s lymphoma of the stomach. Endoscopy. 1987; 19:190–192.
Article13. Kolve M, Fischbach W, Greiner A, Wilms K. Differences in endoscopic and clinicopathological features of primary and secondary gastric non-Hodgkin’s lymphoma. German gastrointestinal lymphoma study group. Gastrointest Endosc. 1999; 49(3 Pt 1):307–315.14. Zullo A, Hassan C, Andriani A, et al. Primary low-grade and high-grade gastric MALT-lymphoma presentation. J Clin Gastroenterol. 2010; 44:340–344.
Article15. Akaza K, Motoori T, Nakamura S, et al. Clinicopathologic study of primary gastric lymphoma of B cell phenotype with special reference to low-grade B cell lymphoma of mucosa-associated lymphoid tissue among the Japanese. Pathol Int. 1995; 45:832–845.
Article16. Hirose Y, Kaida H, Ishibashi M, et al. Comparison between endoscopic macroscopic classification and F-18 FDG PET findings in gastric mucosa-associated lymphoid tissue lymphoma patients. Clin Nucl Med. 2012; 37:152–157.
Article17. Nonaka K, Ohata K, Matsuhashi N, et al. Is narrow-band imaging useful for histological evaluation of gastric mucosa-associated lymphoid tissue lymphoma after treatment? Dig Endosc. 2014; 26:358–364.
Article18. Musshoff K. Clinical staging classification of non-Hodgkin’s lymphomas (author’s transl). Strahlentherapie. 1977; 153:218–221.19. Copie-Bergman C, Gaulard P, Lavergne-Slove A, et al. Proposal for a new histological grading system for post-treatment evaluation of gastric MALT lymphoma. Gut. 2003; 52:1656.
Article20. Wotherspoon AC, Doglioni C, Diss TC, et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993; 342:575–577.
Article21. Yokoi T, Nakamura T, Kasugai K, et al. Primary low-grade gastric mucosa-associated lymphoid tissue (MALT) lymphoma with polypoid appearance. Polypoid gastric MALT lymphoma: a clinicopathologic study of eight cases. Pathol Int. 1999; 49:702–709.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastric Mucosa-associated Lymphoid Tissue Lymphoma Based on Outcome of Domestic Treatment
- Endoscopic Diagnosis of Gastric MALT Lymphoma
- A Polypoid Mucosa-Associated Lymphoid Tissue Lymphoma of the Stomach Treated with Endoscopic Polypectomy
- Endoscopic Findings and Follow-Up of Gastric MALT Lymphoma
- High-grade Hepatic Mucosa-associated Lymphoid Tissue (MALT) Lymphoma Probably Transformed from the Low-grade Gastric MALT Lymphoma