Elastographic measurement of the cervix during pregnancy: Current status and future challenges
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Research Institute of Medical Science, Konkuk University School of Medicine, Seoul, Korea. hwanghs@kuh.ac.kr
- KMID: 2383201
- DOI: http://doi.org/10.5468/ogs.2017.60.1.1
Abstract
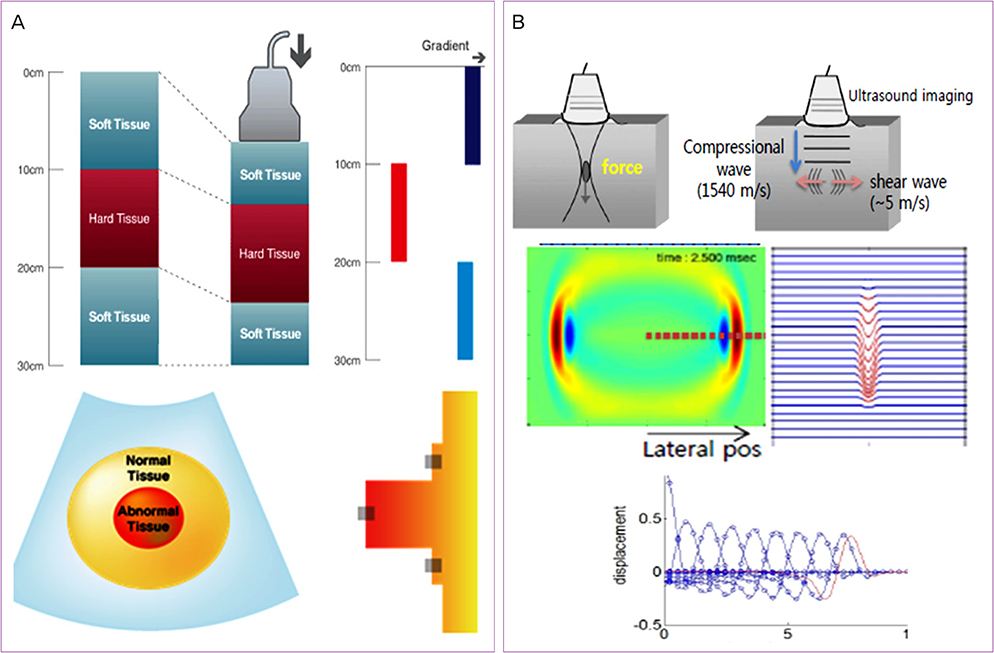
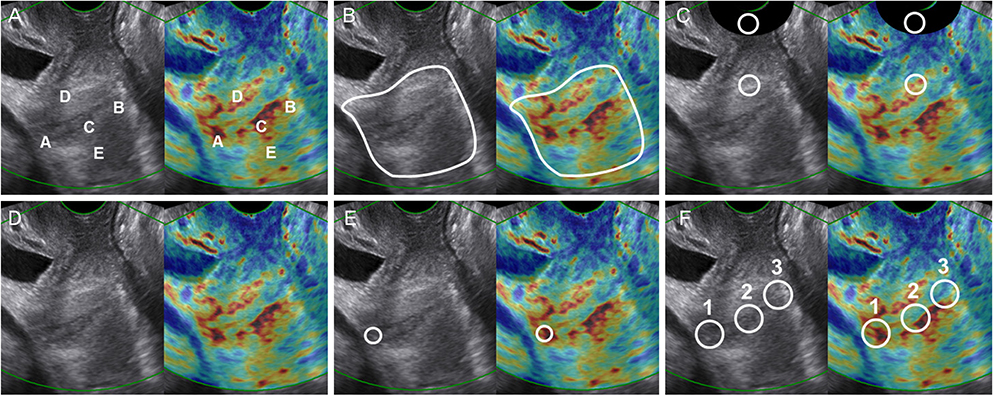
- The cervix is a cylindrical structure that is proximally connected to the uterus and distally to the vaginal cavity. The Bishop score has been used to evaluate the cervix during pregnancy. However, alternatives have been evaluated because the Bishop score is uncomfortable for patients, relies on a subjective examination, and lacks internal os data. Elastography has been used to assess the cervix, as it can estimate tissue stiffness. Recent articles on elastography for cervical assessment during pregnancy have focused on its usefulness for prediction of preterm birth and successful labor induction. There is a clinical need for cervical elastography, as an evaluation of biomechanical factors, because cervical length only assesses morphological changes. However, until now, cervical elastography has been studied in the limited field, and not shown a uniformed methodological technique. In this review, the current status, limitations, and future possibility of cervical elastography were discussed. Future studies should focus on overcoming the limitations of cervical elastography. Although the cervical elastography is presently an incompletely defined technique, it needs to be improved and evaluated as a method for use in combination with cervical length.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Addition of Cervical Elastography May Increase Preterm Delivery Prediction Performance in Pregnant Women with Short Cervix: a Prospective Study
Hyun Soo Park, Hayan Kwon, Dong Wook Kwak, Moon Young Kim, Hyun-Joo Seol, Joon-Seok Hong, Jae-Yoon Shim, Sae-Kyung Choi, Han-Sung Hwang, Min Jeong Oh, Geum Joon Cho, Kunwoo Kim, Soo-young Oh,
J Korean Med Sci. 2019;34(9):. doi: 10.3346/jkms.2019.34.e68.Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters
Hyun-Joo Seol, Ji-Hee Sung, Won Joon Seong, Hyun Mi Kim, Hyun Soo Park, Hayan Kwon, Han-Sung Hwang, Yun Ji Jung, Ja-Young Kwon, Soo-young Oh
Obstet Gynecol Sci. 2020;63(1):42-54. doi: 10.5468/ogs.2020.63.1.42.
Reference
-
1. Danforth DN. The morphology of the human cervix. Clin Obstet Gynecol. 1983; 26:7–13.2. Timmons B, Akins M, Mahendroo M. Cervical remodeling during pregnancy and parturition. Trends Endocrinol Metab. 2010; 21:353–361.3. House M, Kaplan DL, Socrate S. Relationships between mechanical properties and extracellular matrix constituents of the cervical stroma during pregnancy. Semin Perinatol. 2009; 33:300–307.4. Crane JM. Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol. 2006; 49:573–584.5. Wilson LS, Robinson DE. Ultrasonic measurement of small displacements and deformations of tissue. Ultrason Imaging. 1982; 4:71–82.6. Ginat DT, Destounis SV, Barr RG, Castaneda B, Strang JG, Rubens DJ. US elastography of breast and prostate lesions. Radiographics. 2009; 29:2007–2016.7. Lim DJ, Luo S, Kim MH, Ko SH, Kim Y. Interobserver agreement and intraobserver reproducibility in thyroid ultrasound elastography. AJR Am J Roentgenol. 2012; 198:896–901.8. Lerner RM, Parker KJ, Holen J, Gramiak R, Waag RC. Sono-elasticity: medical elasticity images derived from ultrasound signals in mechanically vibrated targets. Acoust Imaging. 1988; 16:317–327.9. Parker KJ, Huang SR, Musulin RA, Lerner RM. Tissue response to mechanical vibrations for “sonoelasticity imaging”. Ultrasound Med Biol. 1990; 16:241–246.10. Samsung Medison. ElastoScan enables the imaging of malignant tumors and other diseases that would normally be undetectable through conventional studies [Internet]. Seoul: Samsung Medison;c2011. cited 2016 Dec 1. Available from: http://www.samsungmedison.com/technology/elastoscan.jsp.11. Shin DK. Principles of ultrasound elastography. In : Korean Society of Ultrasound in Obstetrics and Gynecology. Korean Society of Ultrasound in Obstetrics and Gynecology workshop; 2015 Oct 24; Seoul, Korea. Seoul: Korean Society of Ultrasound in Obstetrics and Gynecology.12. Hernandez-Andrade E, Aurioles-Garibay A, Garcia M, Korzeniewski SJ, Schwartz AG, Ahn H, et al. Effect of depth on shear-wave elastography estimated in the internal and external cervical os during pregnancy. J Perinat Med. 2014; 42:549–557.13. Muller M, Ait-Belkacem D, Hessabi M, Gennisson JL, Grange G, Goffinet F, et al. Assessment of the cervix in pregnant women using shear wave elastography: a feasibility study. Ultrasound Med Biol. 2015; 41:2789–2797.14. Swiatkowska-Freund M, Preis K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet Gynecol. 2011; 38:52–56.15. Hwang HS, Sohn IS, Kwon HS. Imaging analysis of cervical elastography for prediction of successful induction of labor at term. J Ultrasound Med. 2013; 32:937–946.16. Hee L, Rasmussen CK, Schlutter JM, Sandager P, Uldbjerg N. Quantitative sonoelastography of the uterine cervix prior to induction of labor as a predictor of cervical dilation time. Acta Obstet Gynecol Scand. 2014; 93:684–690.17. Muscatello A, Di Nicola M, Accurti V, Mastrocola N, Franchi V, Colagrande I, et al. Sonoelastography as method for preliminary evaluation of uterine cervix to predict success of induction of labor. Fetal Diagn Ther. 2014; 35:57–61.18. Pereira S, Frick AP, Poon LC, Zamprakou A, Nicolaides KH. Successful induction of labor: prediction by preinduction cervical length, angle of progression and cervical elastography. Ultrasound Obstet Gynecol. 2014; 44:468–475.19. Wozniak S, Czuczwar P, Szkodziak P, Paszkowski T. Usefulness of elastography in predicting the outcome of Foley catheter labour induction. Aust N Z J Obstet Gynaecol. 2015; 55:245–250.20. Swiatkowska-Freund M, Traczyk-Los A, Preis K, Lukaszuk M, Zielinska K. Prognostic value of elastography in predicting premature delivery. Ginekol Pol. 2014; 85:204–207.21. Wozniak S, Czuczwar P, Szkodziak P, Milart P, Wozniakowska E, Paszkowski T. Elastography in predicting preterm delivery in asymptomatic, low-risk women: a prospective observational study. BMC Pregnancy Childbirth. 2014; 14:238.22. Hernandez-Andrade E, Romero R, Korzeniewski SJ, Ahn H, Aurioles-Garibay A, Garcia M, et al. Cervical strain determined by ultrasound elastography and its association with spontaneous preterm delivery. J Perinat Med. 2014; 42:159–169.23. Hernandez-Andrade E, Garcia M, Ahn H, Korzeniewski SJ, Saker H, Yeo L, et al. Strain at the internal cervical os assessed with quasi-static elastography is associated with the risk of spontaneous preterm delivery at ≤34 weeks of gestation. J Perinat Med. 2015; 43:657–666.24. Sabiani L, Haumonte JB, Loundou A, Caro AS, Brunet J, Cocallemen JF, et al. Cervical HI-RTE elastography and pregnancy outcome: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2015; 186:80–84.25. Son M, Grobman WA, Ayala NK, Miller ES. A universal mid-trimester transvaginal cervical length screening program and its associated reduced preterm birth rate. Am J Obstet Gynecol. 2016; 214:365.e1–365.e5.26. Orzechowski KM, Boelig RC, Baxter JK, Berghella V. A universal transvaginal cervical length screening program for preterm birth prevention. Obstet Gynecol. 2014; 124:520–525.27. Nakashima K, Shiina T, Sakurai M, Enokido K, Endo T, Tsunoda H, et al. JSUM ultrasound elastography practice guidelines: breast. J Med Ultrason. 2013; 40:359–391.28. Kudo M, Shiina T, Moriyasu F, Iijima H, Tateishi R, Yada N, et al. JSUM ultrasound elastography practice guidelines: liver. J Med Ultrason. 2013; 40:325–357.29. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013; 34:238–253.30. Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol. 2015; 41:1148–1160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters
- Addition of Cervical Elastography May Increase Preterm Delivery Prediction Performance in Pregnant Women with Short Cervix: a Prospective Study
- A Case of Cervical Pregnancy which Required the Conservative Surgical Management after Methotrexate Treatment was Failed
- Cevix Cancer Associated with Pregnancy: A Case Report and Review of the Literature
- Ultrasonography: current status, challenges, and future directions