Obstet Gynecol Sci.
2020 Jan;63(1):42-54. 10.5468/ogs.2020.63.1.42.
Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyung Hee University School of Medicine, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Kyungpook National University Hospital, Daegu, Korea.
- 4Department of Obstetrics and Gynecology, Graduate School of Medicine, Dongguk University, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 6Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 7Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ohsymd@skku.edu
- KMID: 2467931
- DOI: http://doi.org/10.5468/ogs.2020.63.1.42
Abstract
OBJECTIVE
To provide a standardized protocol for the measurement of cervical strain elastography, present its reproducibility, and analyze baseline clinical factors affecting the measurement of elastographic parameters.
METHODS
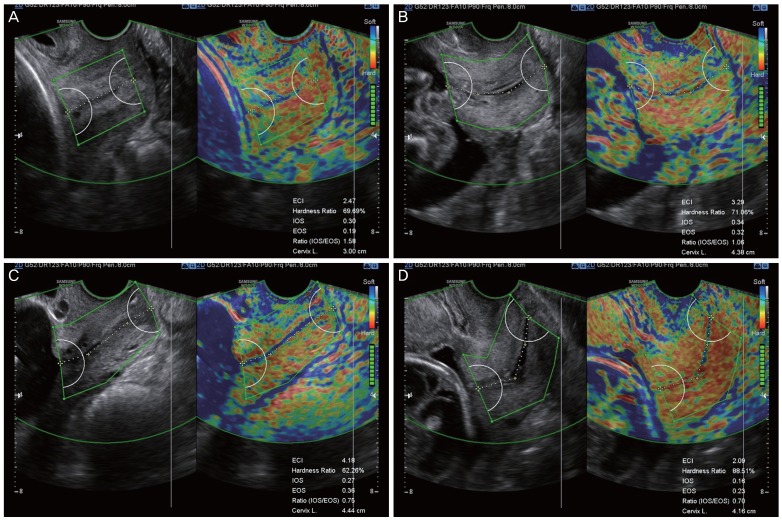
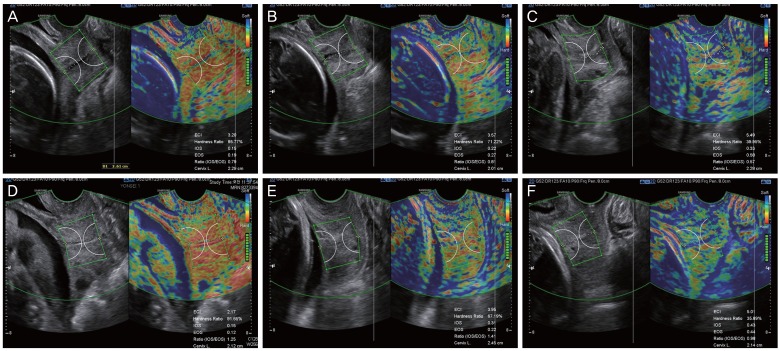
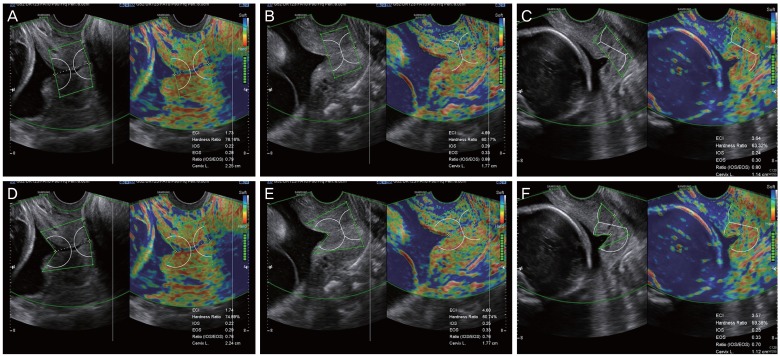
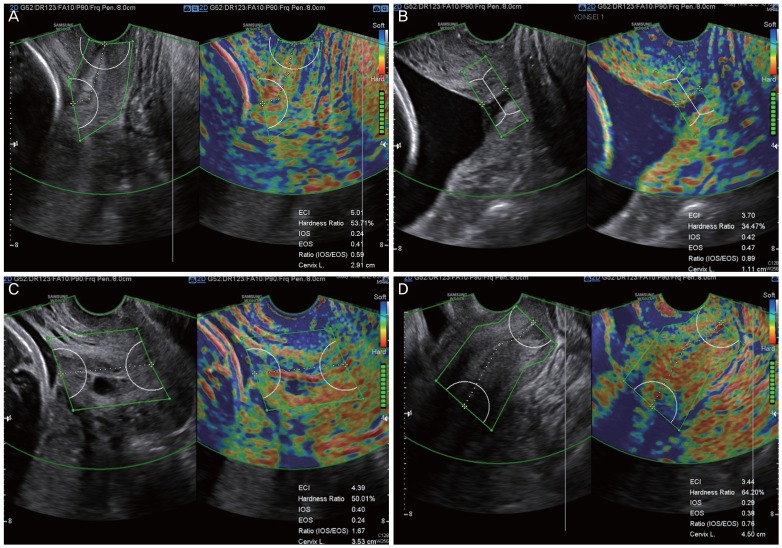
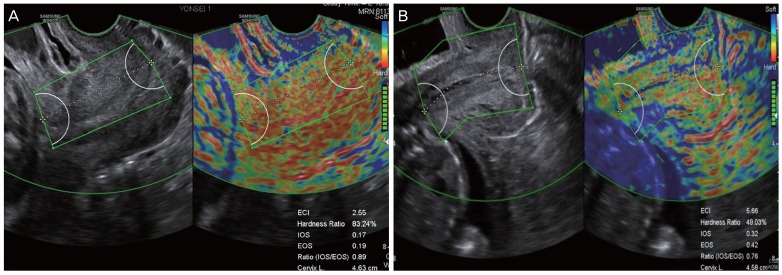
This study was performed by the Korean Research Group of Cervical Elastography. We enrolled pregnant women according to our study protocol. After measuring the cervical length, elastography was performed using the E-Cervixâ„¢ quantification tool to measure the strain of the cervix using intrinsic compression. We evaluated 5 elastographic parameters, namely, the strain of the internal os of the cervix (IOS), strain of the external os of the cervix (EOS), ratio of the strain of IOS and EOS, elasticity contrast index, and hardness ratio. For baseline clinical factors, we examined the maternal body mass index, blood pressure, heart rate, uterine artery Doppler indices, and fetal presentation.
RESULTS
We established a specific protocol for the measurement of cervical elastography using the E cervix program. For all elastographic parameters, the intra-observer intraclass correlation coefficient (ICC) ranged from 0.633 to 0.723 for single measures and from 0.838 to 0.887 for average measures, and the inter-observer ICC ranged from 0.814 to 0.977 for single measures and from 0.901 to 0.988 for average measures. Regression analysis showed that the measurement of the elastographic parameter was not affected by baseline clinical factors.
CONCLUSION
We present a standardized protocol for the measurement of cervical elastography using intrinsic compression. According to this protocol, reproducibility was acceptable and the measurement of elastographic parameters was not affected by the baseline clinical factors studied.
MeSH Terms
Figure
Reference
-
1. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996; 334:567–572. PMID: 8569824.2. Taipale P, Hiilesmaa V. Sonographic measurement of uterine cervix at 18–22 weeks' gestation and the risk of preterm delivery. Obstet Gynecol. 1998; 92:902–907. PMID: 9840546.
Article3. Committee on Practice Bulletins—Obstetrics, The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012; 120:964–973. PMID: 22996126.4. Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 2: breast. Ultrasound Med Biol. 2015; 41:1148–1160. PMID: 25795620.
Article5. Cosgrove D, Barr R, Bojunga J, Cantisani V, Chammas MC, Dighe M, et al. WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: part 4. Thyroid. Ultrasound Med Biol. 2017; 43:4–26. PMID: 27570210.
Article6. Ferraioli G, Filice C, Castera L, Choi BI, Sporea I, Wilson SR, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 3: liver. Ultrasound Med Biol. 2015; 41:1161–1179. PMID: 25800942.
Article7. Park HS, Kwon H, Kwak DW, Kim MY, Seol HJ, Hong JS, et al. Addition of cervical elastography may increase preterm delivery prediction performance in pregnant women with short cervix: a prospective study. J Korean Med Sci. 2019; 34:e68. PMID: 30863266.
Article8. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15:155–163. PMID: 27330520.
Article9. Vayssière C, Morinière C, Camus E, Le Strat Y, Poty L, Fermanian J, et al. Measuring cervical length with ultrasound: evaluation of the procedures and duration of a learning method. Ultrasound Obstet Gynecol. 2002; 20:575–579. PMID: 12493046.
Article10. Iams JD, Grobman WA, Lozitska A, Spong CY, Saade G, Mercer BM, et al. Adherence to criteria for transvaginal ultrasound imaging and measurement of cervical length. Am J Obstet Gynecol. 2013; 209:365.e1–365.e5. PMID: 23958649.11. Baños N, Murillo-Bravo C, Julià C, Migliorelli F, Perez-Moreno A, Ríos J, et al. Mid-trimester sonographic cervical consistency index to predict spontaneous preterm birth in a low-risk population. Ultrasound Obstet Gynecol. 2018; 51:629–636. PMID: 28370687.
Article12. Burger M, Weber-Rössler T, Willmann M. Measurement of the pregnant cervix by transvaginal sonography: an interobserver study and new standards to improve the interobserver variability. Ultrasound Obstet Gynecol. 1997; 9:188–193. PMID: 9165682.
Article13. In : Kim M, Kwak D, Oh S, Sajin K, Yang S, Choi E, Kim M, Park J, Kim K, editors. Intra- and interobserver variance of elastographic parameters measurement of uterine cervix during pregnancy. 26th World Congress on Ultrasound in Obstetrics and Gynecology; 2016 Sep 24–28; Rome, Italy. Hoboken: Wiley;2016. 9. p. 346.14. Feltovich H, Carlson L. New techniques in evaluation of the cervix. Semin Perinatol. 2017; 41:477–484. PMID: 29191290.
Article15. Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, Barr RG, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 1: basic principles and terminology. Ultrasound Med Biol. 2015; 41:1126–1147. PMID: 25805059.
Article16. Feltovich H, Hall TJ, Berghella V. Beyond cervical length: emerging technologies for assessing the pregnant cervix. Am J Obstet Gynecol. 2012; 207:345–354. PMID: 22717270.
Article17. Feltovich H, Hall TJ. Quantitative imaging of the cervix: setting the bar. Ultrasound Obstet Gynecol. 2013; 41:121–128. PMID: 23371343.
Article18. Issaoui M, Debost-Legrand A, Skerl K, Chauveau B, Magnin B, Delabaere A, et al. Shear wave elastography safety in fetus: a quantitative health risk assessment. Diagn Interv Imaging. 2018; 99:519–524. PMID: 29934239.
Article19. Swiatkowska-Freund M, Preis K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet Gynecol. 2011; 38:52–56. PMID: 21484905.
Article20. Bae U, Dighe M, Dubinsky T, Minoshima S, Shamdasani V, Kim Y. Ultrasound thyroid elastography using carotid artery pulsation: preliminary study. J Ultrasound Med. 2007; 26:797–805. PMID: 17526611.21. Dighe M, Bae U, Richardson ML, Dubinsky TJ, Minoshima S, Kim Y. Differential diagnosis of thyroid nodules with US elastography using carotid artery pulsation. Radiology. 2008; 248:662–669. PMID: 18539888.
Article22. Dighe M, Kim J, Luo S, Kim Y. Utility of the ultrasound elastographic systolic thyroid stiffness index in reducing fine-needle aspirations. J Ultrasound Med. 2010; 29:565–574. PMID: 20375375.
Article23. Lim DJ, Luo S, Kim MH, Ko SH, Kim Y. Interobserver agreement and intraobserver reproducibility in thyroid ultrasound elastography. AJR Am J Roentgenol. 2012; 198:896–901. PMID: 22451558.
Article24. Dighe M, Luo S, Cuevas C, Kim Y. Efficacy of thyroid ultrasound elastography in differential diagnosis of small thyroid nodules. Eur J Radiol. 2013; 82:e274–e280. PMID: 23410906.
Article25. Hernandez-Andrade E, Garcia M, Ahn H, Korzeniewski SJ, Saker H, Yeo L, et al. Strain at the internal cervical os assessed with quasi-static elastography is associated with the risk of spontaneous preterm delivery at ≤34 weeks of gestation. J Perinat Med. 2015; 43:657–666. PMID: 25781664.
Article26. Swiatkowska-Freund M, Preis K. Cervical elastography during pregnancy: clinical perspectives. Int J Womens Health. 2017; 9:245–254. PMID: 28461768.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Elastographic measurement of the cervix during pregnancy: Current status and future challenges
- Addition of Cervical Elastography May Increase Preterm Delivery Prediction Performance in Pregnant Women with Short Cervix: a Prospective Study
- Semi-quantitative strain elastography may facilitate pre-surgical prediction of mandibular lymph nodes malignancy in dogs
- Ultrasound-based Liver Elastography: Recent Advances
- Sonographic and Strain Elastographic Findings of a Clear Cell Hidradenoma that Looked Like an Epidermoid Tumor: A Case Report